Abstract
Background
Childhood factors have been associated with increased risk of developing post-traumatic stress disorder (PTSD). Previous studies assessed only a limited number of childhood factors retrospectively. We examined the association between childhood neurodevelopmental, temperamental, behavioral and family environmental characteristics assessed before age 11 years and the development of PTSD up to age 32 years in a birth cohort.
Method
Members of a 1972–73 New Zealand birth cohort (n=1037) who were assessed at ages 26 and 32 years for PTSD as defined by DSM-IV.
Results
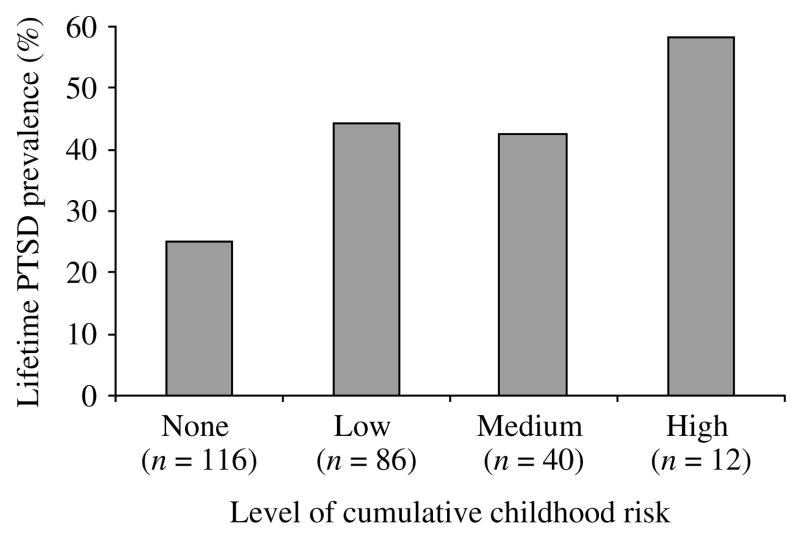
We identified two sets of childhood risk factors. The first set of risk factors was associated both with increased risk of trauma exposure and with PTSD assessed at age 26. These included childhood externalizing characteristics and family environmental stressors, specifically maternal distress and loss of a parent. The second set of risk factors affected risk for PTSD only and included low IQ and chronic environmental adversity. The effect of cumulative childhood factors on risk of PTSD at age 26 was substantial; over 58% of cohort members in the highest risk quartile for three developmental factors had PTSD as compared to only 25% of those not at high risk on any factors. Low IQ at age 5, antisocial behavior, and poverty before age 11 continued to predict PTSD related to traumatic events that occurred between the ages of 26 and 32.
Conclusions
Developmental capacities and conditions of early childhood may increase both risk of trauma exposure and the risk that individuals will respond adversely to traumatic exposures. Rather than being solely a response to trauma, PTSD may have developmental origins.
INTRODUCTION
Childhood risk factors are thought to play an important role in the development of post-traumatic stress disorder (PTSD). The extant literature points to relatively small but significant effects on risk for PTSD for both within-individual characteristics, such as pre-trauma psychopathology, and environmental factors, such as family psychiatric history and general childhood adversity (Brewin et al. 2000; Ozer et al. 2003). Analyses of data from the National Vietnam Veterans Readjustment Study (Kulka et al. 1990), the single epidemiologic study to retrospectively assess a wide range of childhood risk factors, found that childhood antisocial behavior, unstable family environment and prior trauma history were significantly associated with increased risk of PTSD in male veterans. The authors argued that ‘more attention should be given to critical developmental conditions, especially family instability and earlier trauma exposure, in conceptualizing PTSD in adults’ (King et al. 1996, p. 520). The current study examines the contribution of early childhood factors to risk of PTSD in a prospective birth cohort.
PTSD is diagnostically unique among psychiatric disorders, in that exposure to a traumatic event is a diagnostic criterion. Thus, the risk for PTSD can be decomposed (1) into the risk of exposure to a qualifying traumatic event and then, given exposure, (2) into the risk for developing PTSD. Epidemiologic studies have shown that trauma exposure is not randomly distributed in the general population (Breslau, 2002). Factors that lead to trauma exposure may be different than those that increase vulnerability to the effects of that exposure. The identification of factors that contribute to risk at each point is needed to inform interventions aimed at preventing exposure versus those aimed at preventing the development of PTSD in exposed persons.
We tested the hypothesis that childhood factors contribute to the development of PTSD using data from adult members of the Dunedin Multidisciplinary Health and Development Study, a New Zealand cohort followed from birth and first assessed for trauma exposure and PTSD at age 26. We examined the contribution of three sets of early childhood factors (neurocognitive, temperament/behavior, and family environment) to trauma exposure reported at age 26. Next, we examined those same factors in relation to lifetime risk for PTSD at age 26 among those who reported exposure to a traumatic event. Then, we examined the cumulative contribution of these factors to the risk of developing PTSD. One limitation of the age-26 PTSD assessment was that the interview did not ascertain the age of onset for trauma exposure or PTSD. It could not be determined with certainty, therefore, whether or not the childhood risk factors were antecedent to trauma exposure. To address this question, we further report on the association of childhood factors with PTSD that occurred between the ages of 26 and 32 to determine whether a similar pattern of findings emerged.
METHOD
Participants
Participants were members of the Dunedin Multidisciplinary Health and Development Study, a longitudinal investigation of the health and behavior of a complete cohort of children born during a 1-year period in 1972–73 in Dunedin, New Zealand (Silva & Stanton, 1996). Perinatal data were obtained at delivery and when the children were later traced for follow-up at age 3; 1037 individuals (52% male; 91% of eligible births) participated in the assessment, forming the base sample for the longitudinal study. Cohort members represent the full range of socio-economic status (SES) in the general population of New Zealand’s South Island, and are primarily white.
The Dunedin sample had been assessed at ages 3, 5, 7, 9, 11, 13, 15, 18, 21 and 26 years when we saw 980 participants (96% of living cohort members). The research procedure involves bringing four study members per day (including emigrants living overseas) to the research unit within 60 days of their birthday for a full 8-hour day of tightly scheduled individual interviews and tests. Each research topic was presented, in private, as a standardized module by a different trained examiner in counterbalanced order throughout the day. Data were also gathered from other sources, including parents, schools, partners, and courts. After complete description of the study to the subjects, written informed consent was obtained.
Measures
PTSD was assessed using a modified version of the Diagnostic Interview Schedule for DSM-IV (DIS-IV; Robins et al. 1995). The validity of diagnoses has been demonstrated by treatment seeking and functional impairment (Newman et al. 1996). Interviews were conducted by clinicians with degrees in social work, medicine or clinical psychology, blind to participants’ psychiatric history.
For PTSD diagnosis, participants were asked the gate question: ‘Now I would like to ask you about terrible or frightening experiences you may have had at any time in your life. After a frightening or horrible experience, some people can’t get it out of their mind. They may lose interest in other people or activities, they may not sleep well, they may become very jumpy and easily startled or frightened. Have you ever had an experience that caused you problems like these?’ Participants who experienced more than one ‘horrible experience’ were asked to choose their worst experience, get that experience clear in their minds, and answer PTSD diagnostic questions based on that experience.
For participants who reported a ‘horrible experience’, the interviewer asked about specific PTSD symptoms. If the participant met the (B, C, D) symptom criteria for PTSD, the interviewer asked whether the symptoms went away within a month (E criterion). At the end of the PTSD interview module, interviewers asked about the degree these symptoms interfered with daily life in the past year (F criterion), whether or not they spoke with a doctor about their PTSD symptoms in the past year, and whether they still had symptoms in the past year. Participants received a PTSD diagnosis if they met the B, C, D, E, and F criteria for PTSD according to DSM-IV.
PTSD was assessed in a similar fashion at 32 years of age; n=972 (96% of those living). Participants were queried as to whether ‘since [they] were 26, they had had a frightening or horrible experience’. (Recall for the years between age 26 and 32 was enhanced using a life history calendar in the mental health interview session.) Those who endorsed such an experience were then evaluated for PTSD related to that experience. Participants who had more than one ‘horrible experience’ since age 26 were asked to choose their worst experience, get that experience clear in their minds, and answer PTSD diagnostic questions based on that experience. Participants received a PTSD diagnosis if they met the B, C, D, E, and F criteria for PTSD according to DSM-IV.
Childhood characteristics
Our choice of childhood characteristics was informed by two meta-analyses of risk factors for PTSD (Brewin et al. 2000; Ozer et al. 2003). We examined risk factors assessed before age 11 years to maximize the probability that they occurred before the first onset of PTSD. Prevalence of PTSD before age 11 is rare (<0.3%) in community samples (Costello et al. 2003; Ford et al. 2003). All risk factors have been described in detail previously and are summarized here (Moffitt & Caspi, 2001; Cannon et al. 2002; Jaffee et al. 2002; Moffitt et al. 2002).
Neurodevelopmental factors
One meta-analysis (Brewin et al. 2000) cited six studies that included low IQ as a risk factor for PTSD. We also examined additional neurodevelopmental factors to test whether this association was specific to low IQ or represented generalized neurodevelopmental deficits underlying risk for PTSD. ‘Number of perinatal insults’ included a count of 12 prenatal or 12 neonatal problems recorded by clinicians during the mother’s pregnancy (Stanton et al. 1991). Participants were coded as having none, one, or two or more perinatal insults. ‘Gross motor skills’ were measured with the Bayley Motor Scale at age 3 years (Bayley, 1969), the McCarthy Motor Scales at age 5 years (McCarthy, 1972), and the Basic Motor Ability Test at ages 7 and 9 years (Arnheim & Sinclair, 1974). Scores on these measures were standardized and averaged (α=0.71). ‘Binet IQ’ at age 5 years was measured by the Stanford–Binet Intelligence Scales. ‘WISC Fullscale IQ’ at ages 7, 9 and 11 years was assessed by the Wechsler Intelligence Scale for Children – Revised (Weschler, 1990) and was standardized and averaged (α=0.79).
Childhood temperament/behavior
Temperament ratings were made by an examiner during a developmental testing session when the children were ages 3 and 5 years. Three temperament factors emerged from these ratings (difficult, sluggish, and approach) and these were averaged across the two ages (Caspi et al. 1995). Behavior ratings were made at ages 5, 7, 9 and 11 years by teachers who completed the Rutter Child Scale (Elander & Rutter, 1996), which assesses children’s antisocial, worried/fearful, and hyperactive behavior. Scores on each scale were averaged across the ages (all, α>0.70). Participants were classified into quartiles for each temperament factor and behavior scale.
Family environment
Childhood SES was measured with a scale that places each occupation into one of six categories based on the educational level and income associated with that occupation in the New Zealand census (Elley & Irving, 1976). Measures of both parents’ SES were averaged from birth to age 11 years (α=0.79). SES was divided into four categories as follows: highest (scores ⩾5, 16.2%), high (scores ⩾4 and <5, 26.3%), medium (scores ⩾3 and <4, 36.7%) and low (scores <3, 20.9%). ‘Mother’s internalizing symptoms’ were assessed by the Rutter Malaise Inventory when the study members were ages 5, 7 and 9 years (Rodgers et al. 1999). Scores were averaged across the three assessments (α=0.90). Participants were classified into quartiles for mother’s internalizing symptoms. ‘Harsh discipline’ was measured at ages 7 and 9 years using a checklist of 10 disciplinary behaviors that parents indicated they used, such as ‘smack [your child]’. Scores were averaged across the two ages. Other family adversity factors before age 11 years included recording the number of residence changes, number of parent-figure changes, and whether a participant lost a parent to death, divorce or separation.
Statistical analyses
Trauma exposure and PTSD at age 26
Participants who answered no to the gate question were classified as ‘unexposed’ (n=701). Those who answered yes were classified as ‘trauma exposed’ (n=267) and then divided into two groups: those who never met diagnostic criteria for PTSD (n=172) and those who met criteria for PTSD at some point in their lives (n=93). (Two participants from the trauma group did not have complete PTSD data and were excluded from PTSD analyses.) Women were more likely to be diagnosed with PTSD in this cohort [χ2(1, n=966)=4.93, p<0.05]. Therefore, regression analyses were sex-adjusted.
We evaluated group differences on childhood factors using logistic regression. For each risk factor, we conducted two comparisons: (1) unexposed versus trauma-exposed and (2) within the trauma-exposed, never PTSD versus lifetime PTSD. Strength of association between risk factors and outcomes was evaluated using the odds ratio (OR) with 95% confidence intervals (CIs).
We then conducted analyses to assess the cumulative contribution of each set of developmental factors (neurodevelopmental, temperament and behavior, family environment) to risk of developing PTSD. We performed a principal components analysis on the risk factors associated with PTSD at p<0.10 within each of the three sets of factors, and extracted the first principal component for each set. We then examined the association between cumulative childhood risk and the lifetime prevalence of PTSD. Cumulative risk was calculated from the principal components for each developmental factor. One point was given for each factor on which a participant scored in the highest risk quartile (range 0–3). For childhood IQ, the highest risk quartile is the worst quartile on the principal component. Statistical significance was evaluated using the χ2 statistic. We created three dummy variables that categorized participants as being high risk on one, two or three developmental factors, with zero as the reference category. The dummy variables were entered simultaneously into a regression predicting lifetime PTSD. Strength of the association was evaluated using the OR with 95% CI.
PTSD between the ages of 26 and 32
Participants who reported experiencing a traumatic event between the ages of 26 and 32 were divided into two groups: (1) those who met diagnostic criteria for PTSD in relation to an event occurring between the ages of 26 and 32 (n=35) and (2) those who reported a traumatic event but did not meet diagnostic criteria (n=204). Logistic regression analyses evaluated group differences on childhood factors significant at p<0.05 in the age 26 analyses. We then evaluated the association between cumulative childhood risk and PTSD from age 26 to 32 using the cumulative risk variable and procedures.
RESULTS
Childhood characteristics and trauma exposure at age 26
The prevalence of reported trauma exposure in this cohort at age 26 was 27.6% (31.5% for women, 23.8% for men). The types of worst events included: sudden unexpected death of a close family member or friend (38%), personal assault or victimization (32%), serious accidents (14%), hearing about or witnessing a close friend or relative experiencing an assault or serious injury (12%), personal illness (3%), and natural disaster (1%).
Table 1 reports descriptive statistics on neurodevelopmental, temperamental, behavioral, and family environmental characteristics for the entire cohort and then for two groups defined according to their trauma exposure (‘No Trauma’ versus ‘Trauma’). Descriptive statistics for the entire cohort are presented so the reader is able to place the data for the two groups into a normative context. Analyses and results presented below focus only on the ‘No Trauma’ versus ‘Trauma’ groups.
Table 1.
Risk factors for potentially traumatic events reported at age 26 follow-up (n=968)
| Cohorta(n=1037) | No Trauma (n=701) | Trauma (n=267) | Trauma versus No Trauma Univariate OR (95% CI) adjusted for sex | |
|---|---|---|---|---|
| Neurodevelopmental | ||||
| Number of perinatal insults (%) | ||||
| 0 | 54.3 (563) | 55.5 (389) | 54.7 (146) | 1.0 |
| 1 | 26.5 (275) | 26.0 (182) | 27.0 (72) | 1.1 (0.8–1.5) |
| 2 or more | 19.2 (199) | 18.5 (130) | 18.4 (49) | 1.0 (0.7–1.5) |
| Gross motor skills, average ages 3–9, z score, mean (S.D.) | 0.00 (1.00) | 0.07 (0.93) | 0.03 (0.95) | 0.9 (0.8–1.1) |
| Binet IQ age 5, z score, mean (S.D.) | 0.00 (1.00) | 0.06 (0.96) | 0.01 (0.92) | 0.9 (0.8–1.1) |
| WISC Fullscale IQ, average ages 7, 9, 11, z score, mean (S.D.) | 0.00 (1.00) | 0.06 (0.94) | 0.03 (0.89) | 1.0 (0.8–1.1) |
| Childhood temperament and behavior | ||||
| Difficult temperament, average ages 3, 5 (% highest quartile) | 24.6 (254) | 21.8 (152) | 27.3 (73) | 1.5 (1.1–2.2)* |
| Sluggish temperament, average ages 3, 5 (% highest quartile) | 22.6 (233) | 21.1 (147) | 24.3 (65) | 1.0 (0.7–1.5) |
| Approach temperament, average ages 3, 5 (% highest quartile) | 22.6 (233) | 22.9 (160) | 22.9 (61) | 1.3 (0.8–2.0) |
| Teacher-rated antisocial behavior, average ages 5, 7, 9, 11 (% highest quartile) | 26.4 (269) | 24.8 (172) | 30.6 (81) | 1.6 (1.1–2.4)* |
| Teacher-rated worried/fearful, average ages 5, 7, 9, 11 (% highest quartile) | 27.2 (276) | 25.7 (178) | 28.8 (76) | 1.2 (0.7–2.0) |
| Teacher-rated hyperactivity, average ages 5, 7, 9, 11 (% highest quartile) | 27.0 (274) | 25.5 (177) | 29.2 (77) | 1.6 (1.1–2.4)* |
| Teacher-rated as unpopular (% highest quartile) | 24.3 (247) | 22.5 (156) | 24.6 (65) | 1.1 (0.8–1.6) |
| Family environment | ||||
| Socio-economic status, averages ages 1–15 | ||||
| Highest (reference) | 16.2 (167) | 17.1 (119) | 14.3 (38) | 1.0 |
| High v. highest | 26.3 (271) | 27.4 (191) | 24.5 (65) | 1.1 (0.7–1.7) |
| Medium v. highest | 36.7 (378) | 35.1 (245) | 40.4 (107) | 1.4 (0.9–2.1) |
| Low v. highest | 20.9 (215) | 20.5 (143) | 20.8 (55) | 1.2 (0.7–1.9) |
| Mother’s internalizing symptoms, ages 5–11 | 28.9 (291) | 27.3 (188) | 33.1 (87) | 1.2 (1.0–1.4)* |
| Harsh discipline, ages 7, 9 | 24.4 (239) | 24.5 (165) | 23.0 (59) | 1.0 (0.7–1.3) |
| Resident changes birth to age 11 (%) | ||||
| None (reference) | 30.0 (311) | 30.0 (210) | 30.7 (82) | 1.0 |
| 1 v. none | 22.7 (235) | 21.8 (153) | 23.6 (63) | 1.1 (0.7–1.6) |
| 2 v. none | 15.6 (162) | 16.4 (115) | 13.9 (37) | 0.8 (0.5–1.3) |
| 3 or more v. none | 31.7 (328) | 31.8 (223) | 31.8 (85) | 1.0 (0.7–1.4) |
| Any parent change from birth to age 11 (%) | 15.4 (144) | 14.0 (91) | 18.0 (43) | 1.3 (0.9–2.0) |
| Lost a parent before age 11 (%) | 14.6 (151) | 12.7 (89) | 18.7 (50) | 1.6 (1.1–2.3)* |
OR, Odds ratio; CI, confidence interval; WISC, Wechsler Intelligence Scale for Children.
n varies slightly for some risk factors due to missing data.
p<0.05.
Neurodevelopmental characteristics were not significantly associated with increased risk of trauma exposure. Of the childhood temperament and behavior characteristics, difficult temperament, antisocial behavior and hyperactivity were significantly associated with increased risk of trauma exposure. Cohort members rated as high on difficult temperament at ages 3–5 years had 50% greater odds of experiencing trauma than those without difficult temperament. Of the family environmental characteristics, cohort members whose mothers self-reported high levels of internalizing symptoms and who experienced loss of a parent before age 11 years were significantly more likely to report trauma exposure.
Childhood characteristics and the development of PTSD at age 26
The lifetime prevalence of PTSD was 9.6% (11.8% for women, 7.6% for men). Of those with lifetime PTSD, 43% (n=40) met criteria for PTSD in the past year and all of these past-year cases (n=40) reported that their PTSD symptoms interfered moderately or severely during the past year with their ‘life, friends, work or everyday activities’.
Table 2 reports descriptive statistics on neurodevelopmental, temperament/behavioral, and family environmental characteristics for the entire cohort and then separately for cohort members who reported a ‘horrible experience’ classified into two groups according to lifetime PTSD diagnosis (Trauma, never PTSD versus Lifetime PTSD). Of the neurodevelopmental characteristics, only childhood IQ was robustly linked to the development of PTSD. Each standard deviation increase in IQ score at age 5 was associated with 29% (95% CI 5–47) reduced odds of developing PTSD.
Table 2.
Risk factors for post-traumatic stress disorder (PTSD) among cohort members reporting potentially traumatic events at age 26 follow-up (n=265)a
| Cohortb (n=1037) | Trauma, never PTSD (n=172) | Trauma, lifetime PTSD (n=93) | Never versus lifetime PTSD Univariate OR (95% CI) adjusted for sex | |
|---|---|---|---|---|
| Neurodevelopmental | ||||
| Number of perinatal insults, % (n) | ||||
| 0 (reference) | 54.3 (563) | 54.7 (94) | 54.8 (51) | 1.0 |
| 1 | 26.5 (275) | 27.3 (47) | 25.8 (24) | 0.9 (0.5–1.7) |
| 2 or more | 19.2 (199) | 18.0 (31) | 19.4 (18) | 1.0 (0.5–2.1) |
| Gross motor skills, average ages 3–9, z score, mean (S.D.) | 0.00 (1.00) | 0.06 (0.92) | −0.01 (1.00) | 0.9 (0.7–1.2) |
| Stanford–Binet IQ age 5, z score, mean (S.D.) | 0.00 (1.00) | 0.12 (0.89) | −0.15 (0.93) | 0.7 (0.5–1.0)** |
| WISC Fullscale IQ, average ages 7, 9, 11, z score, mean (S.D.) | 0.00 (1.00) | 0.12 (0.83) | −0.11 (0.96) | 0.7 (0.5–1.0)** |
| Childhood temperament and behavior | ||||
| Difficult temperament, average ages 3, 5, % highest quartile (n) | 24.6 (254) | 22.7 (39) | 35.5 (33) | 2.1 (1.1–4.0)** |
| Sluggish temperament, average ages 3, 5, % highest quartile (n) | 22.6 (233) | 26.2 (45) | 19.4 (18) | 0.9 (0.4–1.7) |
| Approach temperament, average ages 3, 5, % highest quartile (n) | 22.6 (233) | 22.7 (39) | 22.6 (21) | 1.4 (0.6–3.2) |
| Teacher-rated antisocial behavior, average ages 5, 7, 9, 11, % highest quartile (n) | 26.4 (269) | 27.1 (46) | 37.6 (35) | 2.0 (1.0–4.0)** |
| Teacher-rated worried/fearful, average ages 5, 7, 9, 11, % highest quartile (n) | 27.2 (276) | 26.0 (44) | 33.3 (31) | 1.6 (0.6–3.9) |
| Teacher-rated hyperactivity, average ages 5, 7, 9, 11, % highest quartile (n) | 27.0 (274) | 26.0 (44) | 33.3 (31) | 1.9 (0.9–3.9)* |
| Teacher-rated as unpopular n (% highest quartile) | 24.3 (247) | 20.7 (35) | 32.3 (30) | 1.8 (1.0–3.2)** |
| Family environment | ||||
| Socio-economic status, averages ages 1–15, % (n) | ||||
| Highest (reference) | 16.2 (167) | 17.0 (29) | 9.8 (9) | 1.0 |
| High v. highest | 26.3 (271) | 24.6 (42) | 25.0 (23) | 1.8 (0.7–4.4) |
| Medium v. highest | 36.7 (378) | 40.9 (70) | 39.1(36) | 1.7 (0.7–3.9) |
| Low v. highest | 20.9 (215) | 17.5 (30) | 26.1 (24) | 2.6 (1.0–6.6)** |
| Mother’s internalizing symptoms, ages 5–11, % highest quartile (n) | 28.9 (291) | 31.0 (52) | 37.6 (35) | 1.4 (1.1–1.8)** |
| Harsh discipline, ages 7, 9, % highest quartile (n) | 24.4 (239) | 22.0 (36) | 25.3 (23) | 1.2 (0.7–2.3) |
| Resident changes birth to age 11, % (n) | ||||
| None (reference) | 30.0 (311) | 33.7 (58) | 24.7 (23) | 1.0 |
| 1 v. none | 22.7 (235) | 25.6 (44) | 20.4 (19) | 1.1 (0.5–2.3) |
| 2 v. none | 15.6 (162) | 13.4 (23) | 15.1 (14) | 1.6 (0.7–3.5) |
| 3 or more v. none | 31.7 (328) | 27.3 (47) | 39.8 (37) | 2.0 (1.1–3.8)** |
| Any parent change from birth to age 11, % (n) | 15.4 (144) | 13.6 (21) | 25.6 (21) | 2.2 (1.1–4.4)** |
| Lost a parent before age 11, % (n) | 14.6 (151) | 14.0 (24) | 28.0 (26) | 2.4 (1.3–4.5)*** |
OR, Odds ratio; CI, confidence interval; WISC, Wechsler Intelligence Scale for Children.
PTSD diagnosis was not available for two participants who reported trauma exposure. Thus, n=265 for these analyses.
n varies slightly for some risk factors due to missing data.
p<0.10,
p<0.05,
p<0.01.
Of the childhood temperament and behavioral characteristics, difficult temperament, antisocial behavior and being unpopular were significantly associated with increased risk of developing PTSD. Children with a difficult temperament and children who were antisocial had a 100% increase in the odds of developing PTSD as compared to members without such problems.
Five of six indices of family environment were significantly associated with increased risk of developing PTSD. Cohort members from low-SES families who changed residences three or more time before age 11 years or had experienced changes in a parent figure had over a 100% increase in the odds of developing PTSD compared to controls. Cohort members whose mothers had high levels of internalizing symptoms were also at increased risk of developing PTSD.
The first principal component extracted from the neurodevelopmental measures (accounting for 85% of the variance) was labeled ‘childhood IQ’; the first principal component extracted from the childhood temperament and behavior measures (60% of the variance) was labeled ‘externalizing-spectrum problems’; the first principal component extracted from the family environment measures (40% of the variance) was labeled ‘family adversity’.
Cumulative childhood risk and the development of PTSD at age 26
Fig. 1 shows that over 58% of cohort members in the highest risk quartile for all three developmental factors had PTSD as compared to only 25% of those not high risk on any factors [χ2(3, n=254)=11.95, p=0.008]. PTSD prevalence was higher in those with one (OR 2.4, 95% CI 1.3–4.3, p=0.005), two (OR 2.2, 95% CI 1.0–4.7, p=0.04) and three (OR 4.7, 95% CI 1.4–16.5, p=0.01) high-risk factors versus those with none.
Fig. 1.
The prevalence (%) of lifetime post-traumatic stress disorder (PTSD) at age 26 by level of cumulative childhood risk among cohort members reporting exposure to a potentially traumatic event.
Childhood characteristics and PTSD from age 26 to 32
The number of PTSD cases was much smaller for the age 32 (n=35) than the age 26 analysis (n=93). Thus, interpretation of the results focused on comparing the strength of the association (ORs) between childhood factors and PTSD at the two time points rather than on statistical significance; ORs at the two time points may be similar but not statistically significant at age 32 due to reduced power. Among the 239 participants who reported an event between the ages of 26 and 32, the types of worst events included: sudden unexpected death of a close family member or friend (22.2%), personal assault or victimization (15.5%), serious accidents (9.6%), hearing about or witnessing a close friend or relative experiencing an assault or serious injury (23.8%), personal illness (10.0%), natural disaster (1.7%), terrorism or war (1.3%), and other personal traumas (15.9%).
Table 3 presents the descriptive statistics for the ‘Trauma no PTSD’ versus ‘PTSD’ groups. IQ measured at age 5 years was approximately 0.40 S.D. lower among study members who developed PTSD compared to study members who were trauma-exposed but did not develop PTSD. The association between IQ at ages 7 to 11 and PTSD was slightly attenuated (from OR 0.7 to 0.8). Childhood externalizing characteristics were associated with increased risk of PTSD, but the strength of the association was attenuated for difficult temperament and being unpopular. Childhood antisocial behavior remained a robust and significant predictor of PTSD. The association between family environmental factors and PTSD was largely attenuated, except for low SES. The association between low SES and PTSD was stronger at age 32 than at age 26; cohort members from low SES families had over a 200% increase in the odds of developing PTSD.
Table 3.
Risk factors for post-traumatic stress disorder (PTSD) among participants reporting potentially traumatic events occurring between the ages of 26–32 (n=239)
| Trauma, no PTSD (n=204) | PTSD (n=35) | Trauma, no PTSD versus PTSD Univariate OR (95% CI) adjusted for sex | |
|---|---|---|---|
| Neurodevelopmental | |||
| Stanford–Binet IQ age 5, z score, mean (S.D.) | 0.03 (0.99) | −0.40 (0.99) | 0.6 (0.4–1.0)* |
| WISC full-scale IQ, average ages 7, 9, 11, z score, mean (S.D.) | −0.01 (0.98) | −0.18 (0.84) | 0.8 (0.6–1.1) |
| Childhood temperament and behavior | |||
| Difficult temperament, average ages 3, 5 (% highest quartile) | 25.0 (51) | 37.1 (13) | 1.8 (0.9–3.9) |
| Teacher-rated antisocial behavior, average ages 5, 7, 9, 11 (% highest quartile) | 26.1 (53) | 42.9 (15) | 2.1 (1.0–4.4)* |
| Teacher-rated as unpopular (% highest quartile) | 22.2 (45) | 28.6 (10) | 1.4 (0.6–3.1) |
| Family environment | |||
| Socio-economic status, averages ages 1–15 | |||
| Highest+high (reference) | 43.6 (89) | 25.7 (9) | 1.0 |
| Medium v. highest or high | 39.2 (80) | 40.0 (14) | 1.7 (0.7–4.2) |
| Low v. highest or high | 17.2 (35) | 34.3 (12) | 3.4 (1.3–8.7)* |
| Mother’s internalizing symptoms, ages 5–11 (% highest quartile) | 34.3 (70) | 24.2 (8) | 0.9 (0.6–1.3) |
| Resident changes birth to age 11 (%) | |||
| None+1 (reference) | 49.5 (101) | 48.6 (17) | 1.0 |
| 2 or more v. none or 1 | 50.5 (103) | 51.4 (18) | 1.1 (0.5–2.2) |
| Any parent change from birth to age 11 (%) | 21.0 (39) | 22.6 (7) | 1.1 (0.4–2.8) |
| Lost a parent before age 11 (%) | 19.6 (40) | 17.1 (6) | 0.8 (0.3–2.2) |
OR, Odds ratio; CI, confidence interval; WISC, Wechsler Intelligence Scale for Children.
p<0.05.
Of cohort members who reported experiencing a traumatic event between the ages of 26 and 32, over 23% of those in the highest risk quartile for two or three developmental factors had PTSD. (The two highest cumulative risk categories were combined because of the small number of PTSD cases.) By contrast, 17.2% of those high risk on one factor and only 8% of those not high risk on any factors met criteria for the disorder [χ2(2, n=228)=7.04, p=0.03]. PTSD prevalence was higher in those with one (OR 2.3, 95% CI 0.9–5.8, p=0.09) and two or three (OR 3.2, 95% CI 1.3–8.0, p=0.01) high-risk factors versus those with none.
DISCUSSION
Our findings suggest that both within-individual childhood characteristics and early environmental conditions increase risk of developing PTSD. Specifically, two sets of risk factors for PTSD at age 26 emerged. The first set of factors affected the risk of trauma exposure as well as the risk of developing PTSD once exposed. These risk factors included children’s externalizing characteristics (including difficult temperament, antisocial behavior, and hyperactivity), family history of mental-health difficulties (including maternal reports of distress), and family adversities (including loss of a parent). The second set of factors affected risk for PTSD only. These risk factors included low IQ and chronic environmental stressors such as low SES. The effect of cumulative childhood risk was substantial; over 58% of cohort members in the highest risk quartile for three developmental factors had PTSD by age 26 as compared to only 25% of those not at high risk on any factors.
One limitation of the age-26 PTSD assessment was that the interview did not ascertain the age of onset for trauma exposure or PTSD. PTSD before age 11 is rare in general population samples (Costello et al. 2003; Ford et al. 2003), and our risk factors were measured prior to age 11, suggesting that the risks preceded PTSD for most cases. However, to document with certainty that risks were antecedent to trauma exposure, we tested whether childhood factors predicted PTSD that occurred in relation to traumatic events between the ages of 26 and 32. The association of low IQ and externalizing behavior with PTSD was similar, albeit slightly attenuated, compared to that for the age 26 cases. In fact, both IQ at age 5 and antisocial behavior remained robust, significant predictors of PTSD, even though there were only 35 PTSD cases at the age-32 assessment. The most substantial attenuation was observed for family environmental factors, except for low SES, which remained a strong predictor of PTSD. The effect of family environment on many traits has been shown to stronger in childhood and attenuate in adulthood (Plomin et al. 2001; Jaffee et al. 2002). Moreover, PTSD related to childhood events was excluded from the age 26–32 data. Exclusion of childhood events has been related to attenuated associations between childhood characteristics (retrospectively assessed) and PTSD in one other study (Breslau et al. 1995). However, the effect of cumulative childhood risk on PTSD remained substantial. For participants who experienced traumatic events between the ages of 26 and 32, over 23% of cohort members in the highest risk quartile for two or three developmental factors had developed PTSD compared to only 8% of those not at high risk on any factors.
Three findings stand out. First, whereas some research suggests that low IQ and other cognitive deficits may be PTSD sequelae (De Bellis, 2001), the present study, along with prospective studies of military samples (Pitman et al. 1991; Macklin et al. 1998; Kremen et al. in press), implicates low IQ as a risk factor. The mechanism by which low IQ increases risk of PTSD is not understood. It is possible that individuals with more cognitive resources are better able to translate their traumatic event into a narrative (Pennebaker, 1999) and make meaning out of it (Janoff-Bulman, 1992). In addition, low IQ is a risk factor for other forms of psychopathology (Fergusson et al. 2005), including externalizing disorders, which are in turn associated with increased risk of trauma exposure and PTSD.
Second, the findings suggest unstable early environmental conditions may sensitize individuals to the adverse effects of later stressors. Animal models suggest that offspring reared under stressful conditions are insecurely attached, emotionally dysregulated (Rosenblum & Paully, 1984; Coplan et al. 1998), and show persisting alterations in functioning of the hypothalamic–pituitary–adrenal (HPA) axis (Gorman et al. 2002; Heim & Nemeroff, 2002). Dysregulation of the HPA axis is implicated in the etiology of PTSD and is a potential biological mechanism linking the association between early environmental conditions and the development of PTSD (Yehuda, 2002).
Third, the association between children’s externalizing-spectrum problems and risk of PTSD replicates an association previously documented using retrospective data (Kulka et al. 1990; Breslau et al. 1991; Kessler et al. 1995; Koenen et al. 2005). Difficult temperament, antisocial behavior and hyperactivity are manifestations of poor self-regulation that may place the individual at increased risk of trauma exposure. Individuals with poor self-regulation, broadly defined by the inability ‘to modulate behavior according to the cognitive, emotional and social demands of a particular situation’ (Calkins & Fox, 2002, p. 479), may be more likely to develop PTSD once exposed to trauma because they lack the affect tolerance necessary for processing the traumatic event. Instead, they are likely to angrily act out, or to engage in avoidance, strategies shown to interfere with PTSD recovery in community samples (Koenen et al. 2003).
The strengths of the current study include the use of a birth cohort, prospective measures of a range of childhood characteristics, and a low attrition rate. However, the present study has several limitations. First, our ascertainment of trauma exposure asked respondents if they had had any horrible experience that gave them difficulties such as sleep disturbance or jumpiness. As a result of this protocol, our trauma-exposed group was selected for respondents who recalled at least a minor, acute reaction to the trauma. Trauma-exposed participants who experienced no acute reaction would not have been included in the trauma-exposed group. Therefore, the childhood characteristics associated with trauma exposure in this sample may not apply to individuals who experienced an event but were not bothered by it. Our definition of exposure also probably increased the similarity between the trauma-exposed no-PTSD and PTSD groups, and therefore probably attenuated differences in childhood characteristics. Second, because of time constraints it was not possible for the Dunedin team to interview participants more extensively to ascertain details about the nature of their traumatic event, the possibility of repeated trauma exposures, their age at exposure, or other contextual details. Therefore, we could not test whether the association between early childhood risk factors and the development of PTSD was mediated by trauma type. Findings from other studies support such mediation (Bromet et al. 1998). Third, results of the present study are limited to a single, contemporary cohort of New Zealand young adults. Although lifetime rates of PTSD in this cohort (11.8% for women, 7.6% for men) are similar to those reported by the National Comorbidity Survey (NCS; Kessler et al. 1995) for young adults in the same age range (11.2% for women, 5.6% for men), further research is required to determine whether our findings will generalize to other times and places. Fourth, studies with larger sample sizes of PTSD cases are needed to examine the interplay of childhood characteristics and sex differences in the etiology of PTSD. Fifth, our study was not a genetically sensitive design. Genetic influences account for substantial variation in PTSD (True et al. 1993; Stein et al. 2002). Future research is needed to determine whether the link between the childhood risk factors we studied and PTSD is environmentally or genetically mediated.
A developmental perspective on the epidemiology of PTSD has implications for research and practice. Our findings suggest that a developmental perspective should not be limited to studies of childhood PTSD. Rather, developmental capacities and conditions of early childhood may increase both risk of trauma exposure and the risk that individuals will respond adversely to traumatic exposures. Further research into the developmental epidemiology of PTSD may improve understanding of its etiology. Clinicians may find their treatment approach informed by integrating information on clients’ childhood cognitive and temperamental characteristics and other environmental experiences, particularly those related to chronic adversity, into their case conceptualization. In fact, psychotherapy that combines a developmentally informed approach to addressing deficits in clients’ emotional and interpersonal capacities with more traditional trauma-focused treatment has been shown to be highly effective in treating adult PTSD (Cloitre et al. 2006). Finally, prevention efforts aimed at addressing some of these developmental capacities, such as antisocial behavior, or at improving conditions of chronic adversity, such as poverty, may ultimately reduce risk of PTSD.
Acknowledgments
Dr Koenen is supported in part by US-NIMH K08 MH070627. The Dunedin Multidisciplinary Health and Development Research Unit is supported by the New Zealand Health Research Council. This research received support from UK Medical Research Council grant G0100527, from US-NIMH grants MH45070 and MH49414, and from the William T. Grant Foundation. Terrie E. Moffitt and Avshalom Caspi are Royal Society-Wolfson Merit Award holders. We thank the Dunedin Study members, their parents, teachers, and Study founder Phil Silva. This study protocol was approved by the institutional review boards of the Institute of Psychiatry, University of Wisconsin, and the Dunedin School of Medicine. The data analysis was approved by the human subjects committee at the Harvard School of Public Health. Study members gave informed consent before participating.
Footnotes
DECLARATION OF INTEREST
None.
References
- Arnheim D, Sinclair W. The Clumsy Child. Mosby; St Louis, MO: 1974. [Google Scholar]
- Bayley N. The Bayley Scales of Infant Development. The Psychological Corporation; New York: 1969. [Google Scholar]
- Breslau N. Epidemiologic studies of trauma, posttraumatic stress disorder, and other psychiatric disorders. Canadian Journal of Psychiatry. 2002;47:923–929. doi: 10.1177/070674370204701003. [DOI] [PubMed] [Google Scholar]
- Breslau N, Davis GC, Andreski P. Risk factors for PTSD-related traumatic events: a prospective analysis. American Journal of Psychiatry. 1995;152:529–535. doi: 10.1176/ajp.152.4.529. [DOI] [PubMed] [Google Scholar]
- Breslau N, Davis GC, Andreski P, Peterson E. Traumatic events and posttraumatic stress disorder in an urban population of young adults. Archives of General Psychiatry. 1991;48:216–222. doi: 10.1001/archpsyc.1991.01810270028003. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology. 2000;68:317–336. doi: 10.1037//0022-006x.68.5.748. [DOI] [PubMed] [Google Scholar]
- Bromet E, Sonnega A, Kessler RC. Risk factors for DSM-III-R posttraumatic stress disorder: findings from the National Comorbidity Survey. American Journal of Epidemiology. 1998;147:353–361. doi: 10.1093/oxfordjournals.aje.a009457. [DOI] [PubMed] [Google Scholar]
- Calkins SD, Fox NA. Self-regulatory processes in early personality development: a multilevel approach to the study of childhood social withdrawal and aggression. Development and Psychopathology. 2002;14:477–498. doi: 10.1017/s095457940200305x. [DOI] [PubMed] [Google Scholar]
- Cannon M, Caspi A, Moffit TE, Harrington H, Taylor A, Murray R, Poulton R. Evidence for early-childhood, pan-developmental impairment specific to schizophreniform disorder. Archives of General Psychiatry. 2002;59:449–456. doi: 10.1001/archpsyc.59.5.449. [DOI] [PubMed] [Google Scholar]
- Caspi A, Henry B, McGee RO, Moffitt TE, Silva PA. Temperamental origins of child and adolescent behavior problems: from age three to age fifteen. Child Development. 1995;66:55–68. doi: 10.1111/j.1467-8624.1995.tb00855.x. [DOI] [PubMed] [Google Scholar]
- Cloitre M, Cohen LR, Koenen KC. Treating the Trauma of Childhood Abuse: Psychotherapy for the Interrupted Life. Guilford Press; New York: 2006. [Google Scholar]
- Coplan JD, Trost RC, Owens MJ, Cooper TB, Gorman JM, Nemeroff CB, Rosenblum LA. Cerebrospinal fluid concentrations of somatostatin and biogenic amines in grown primates reared by mothers exposed to manipulated foraging conditions. Archives of General Psychiatry. 1998;55:473–477. doi: 10.1001/archpsyc.55.5.473. [DOI] [PubMed] [Google Scholar]
- Costello JE, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2003;60:837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- De Bellis MD. Developmental traumatology: the psycho-biological development of maltreated children and its implications for research, treatment, and policy. Development and Psychopathology. 2001;13:539–564. doi: 10.1017/s0954579401003078. [DOI] [PubMed] [Google Scholar]
- Elander J, Rutter M. Use and development of the Rutter Parents’ and Teachers’ scales. International Journal of Methods in Psychiatric Research. 1996;6:63–78. [Google Scholar]
- Elley WB, Irving JC. Revised socio-economic index for New Zealand. New Zealand Journal of Educational Studies. 1976;7:153–167. [Google Scholar]
- Fergusson DM, Horwood LJ, Ridder EM. Show me the child at seven. II: Childhood intelligence and later outcomes in adolescence and young adulthood. Journal of Child Psychology and Psychiatry and Allied Disciplines. 2005;46:850–858. doi: 10.1111/j.1469-7610.2005.01472.x. [DOI] [PubMed] [Google Scholar]
- Ford T, Goodman R, Meltzer R. The British Child and Adolescent Mental Health Survey 1999: the prevalence of DSM-IV disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:1203–1211. doi: 10.1097/00004583-200310000-00011. [DOI] [PubMed] [Google Scholar]
- Gorman JM, Mathew S, Coplan J. Neurobiology of early life stress: nonhuman primate models. Seminars in Clinical Neuropsychiatry. 2002;7:96–103. doi: 10.1053/scnp.2002.31784. [DOI] [PubMed] [Google Scholar]
- Heim C, Nemeroff CB. Neurobiology of early life stress: clinical studies. Seminars in Clinical Neuropsychiatry. 2002;7:147–159. doi: 10.1053/scnp.2002.33127. [DOI] [PubMed] [Google Scholar]
- Jaffee SR, Moffitt TE, Caspi A, Fombonne E, Poulton R, Martin J. Differences in early childhood risk factors for juvenile-onset and adult-onset depression. Archives of General Psychiatry. 2002;59:215–222. doi: 10.1001/archpsyc.59.3.215. [DOI] [PubMed] [Google Scholar]
- Janoff-Bulman R. Shattered Assumptions: Towards a New Psychology of Trauma. The Free Press; New York: 1992. [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- King DW, King LA, Foy DW, Gudanowski DM. Prewar factors in combat-related posttraumatic stress disorder: structural equation modeling with a national sample of female and male Vietnam veterans. Journal of Consulting and Clinical Psychology. 1996;64:520–531. doi: 10.1037//0022-006x.64.3.520. [DOI] [PubMed] [Google Scholar]
- Koenen KC, Fu QJ, Lyons MJ, Goldberg J, Toomey R, Eisen SA, True W, Tsuang MT. Juvenile conduct disorder as a risk factor for posttraumatic stress disorder. Journal of Traumatic Stress. 2005;18:23–32. doi: 10.1002/jts.20010. [DOI] [PubMed] [Google Scholar]
- Koenen KC, Stellman JM, Stellman SD, Sommer JFJ. Risk factors for course of PTSD among Vietnam veterans: a 14-year follow-up of American legionnaires. Journal of Consulting and Clinical Psychology. 2003;71:980–986. doi: 10.1037/0022-006X.71.6.980. [DOI] [PubMed] [Google Scholar]
- Kremen W, Koenen KC, Purcell S, Boark C, Eisen SA, True W, Lyons MJ. A co-twin control study of cognitive ability and PTSD. Archives of General Psychiatry. doi: 10.1001/archpsyc.64.3.361. in press. [DOI] [PubMed] [Google Scholar]
- Kulka RA, Schlenger WE, Fairbank JA, Hough RL, Jordan BK, Marmar CR, Weiss DS. Trauma and the Vietnam War Generation: Report of Findings from the National Vietnam Veterans Readjustment Study. Bruner/Mazel; New York: 1990. [Google Scholar]
- Macklin ML, Metzger LJ, Litz BT, McNally RJ, Lasko NB, Orr SP, Pitman RK. Lower precombat intelligence is a risk factor for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 1998;66:323–326. doi: 10.1037//0022-006x.66.2.323. [DOI] [PubMed] [Google Scholar]
- McCarthy D. McCarthy Scales of Children’s Abilities. The Psychological Corporation; New York: 1972. [Google Scholar]
- Moffitt TE, Caspi A. Childhood predictors differentiate life-course persistent and adolescence-limited antisocial pathways among males and females. Development and Psychopathology. 2001;13:355–375. doi: 10.1017/s0954579401002097. [DOI] [PubMed] [Google Scholar]
- Moffitt TE, Caspi A, Honalee H, Milne BJ. Males on the life-course-persistent and adolescence-limited antisocial pathways: follow-up at age 26 years. Development and Psychopathology. 2002;14:179–207. doi: 10.1017/s0954579402001104. [DOI] [PubMed] [Google Scholar]
- Newman DL, Moffitt TE, Caspi A, Magdol L, Silva PA, Stanton WR. Psychiatric disorder in a birth cohort of young adults: prevalence, comorbidity, clinical significance, and new case incidence from ages 11 to 21. Journal of Consulting and Clinical Psychology. 1996;64:552–562. [PubMed] [Google Scholar]
- Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychological Bulletin. 2003;129:52–73. doi: 10.1037/0033-2909.129.1.52. [DOI] [PubMed] [Google Scholar]
- Pennebaker JW. The effects of traumatic disclosure on physical and mental health: the values of writing and talking about upsetting events. International Journal of Emergency Mental Health. 1999;1:9–18. [PubMed] [Google Scholar]
- Pitman RK, Orr SP, Lowenhagen MJ, Macklin ML, Altman B. Pre-Vietnam contents of posttraumatic stress disorder veterans’ service medical and personnel records. Comprehensive Psychiatry. 1991;32:416–422. doi: 10.1016/0010-440x(91)90018-8. [DOI] [PubMed] [Google Scholar]
- Plomin R, DeFries JC, McClearn GE, McGuffin P. Behavioral Genetics. Worth Publishers; New York: 2001. [Google Scholar]
- Robins LN, Cottler L, Bucholz K, Compton W. Diagnostic Interview Schedule for DSM-IV. Washington University Press; St Louis, MO: 1995. [Google Scholar]
- Rodgers B, Pickles A, Power C, Collishaw S, Maughan B. Validity of the Malaise Inventory in general population samples. Social Psychiatry and Psychiatric Epidemiology. 1999;34:333–341. doi: 10.1007/s001270050153. [DOI] [PubMed] [Google Scholar]
- Rosenblum LA, Paully GS. The effects of varying environmental demands on maternal and infant behavior. Child Development. 1984;55:305–314. [PubMed] [Google Scholar]
- Silva PA, Stanton WR. From Child to Adult: The Dunedin Multidisciplinary Health and Development Study. Oxford University Press; New York: 1996. [Google Scholar]
- Stanton WR, McGee R, Silva PA. Indices of perinatal complications, family background, child rearing, and health as predictors of early cognitive and motor development. Pediatrics. 1991;88:954–959. [PubMed] [Google Scholar]
- Stein MB, Jang KJ, Taylor S, Vernon PA, Livesley WJ. Genetic and environmental influences on trauma exposure and posttraumatic stress disorder: a twin study. American Journal of Psychiatry. 2002;159:1675–1681. doi: 10.1176/appi.ajp.159.10.1675. [DOI] [PubMed] [Google Scholar]
- True WJ, Rice J, Eisen SA, Heath AC, Goldberg J, Lyons MJ, Nowak J. A twin study of genetic and environmental contributions to liability for posttraumatic stress symptoms. Archives of General Psychiatry. 1993;50:257–264. doi: 10.1001/archpsyc.1993.01820160019002. [DOI] [PubMed] [Google Scholar]
- Weschler D. Weschler Preschool and Primary Scale of Intelligence–Revised. The Psychological Corporation, Harcourt Brace and Company; London: 1990. [Google Scholar]
- Yehuda R. Current status of cortisol findings in post-traumatic stress disorder. Psychiatric Clinics of North America. 2002;25:341–368. doi: 10.1016/s0193-953x(02)00002-3. [DOI] [PubMed] [Google Scholar]