Abstract
Study Objectives:
The Cologne Children's Sleep Study intended to provide information on prevalence and course of difficulties of initiating and maintaining sleep in childhood.
Design:
Longitudinal study.
Setting:
Children of the fourth grade of elementary schools in Cologne.
Participants:
832 children and their parents; the mean age of the children was 9.4, 10.7, and 11.7 years at the 3 assessments.
Measurements and Results:
Children and parents were surveyed using questionnaires 3 times on an annual basis. In self- and parental reports, about 30%-40% of the children of the longitudinal sample had problems falling asleep at the first assessment. One year later, about 30% to 40% of these children did not describe any difficulties initiating sleep, whereas about 60% did report continuing difficulties initiating sleep. Difficulties maintaining sleep are less common in childhood. The analysis of self- and parental reports revealed that in general children described significantly more difficulties initiating and maintaining sleep than their parents report.
Conclusions:
Difficulties initiating and maintaining sleep may be transient or persistent. In practice, children and adolescents should be included in the diagnostic and therapeutic process.
Citation:
Fricke-Oerkermann L; Plück J; Schredl M; Heinz K; Mitschke A; Wiater A; Lehmkuhl G. Prevalence and course of sleep problems in childhood. SLEEP 2007;30(10):1371-1377.
Keywords: Sleep disorders, children, longitudinal survey
INTRODUCTION
SLEEP PROBLEMS ARE FREQUENT IN CHILDREN.1–4 IPSIROGLU ET AL. SURVEYED SCHOOL CHILDREN AGED 11 TO 15 YEARS; 12% OF THE CHILDREN REPORTED SLEEP problems every night, 76% reported occasional sleep problems, and 12% had no sleep problems.5 Difficulty initiating and maintaining sleep is one of the most frequent sleep problems in childhood.6 Archbold et al. assessed the frequency of childhood sleep problems in a clinical sample in which 41% of the parents reported insomnia in their children, aged 2 to 14 years.7 In a normal school-age population, 31% of children aged 6 to 13 years reported having disorders of initiating and maintaining sleep.1 In the study of Liu et al., 16% of the parents of the U.S. sample reported that their children aged 4 to 11 years “sometimes” and 5% “usually” have difficulties falling asleep.8 Johnson et al. found that the prevalence of current insomnia defined by DSM-IV was 9% and that the lifetime prevalence of insomnia was 11% in adolescents aged 13 to 16 years.9 Liu et al. reported that 17% of the adolescents aged 12 to 18 years described insomnia symptoms.10 The differences in the prevalence rates are based on different methods, samples, and ages of the children.
Little is known, however, about the course of school children's sleep disorders, because longitudinal data are still underrepresented. Jenni et al. longitudinally followed almost 500 children up to the age of 10 years. Bed sharing, as well as nocturnal waking, increased with age and reached a maximum at 4 years. Bed sharing and night waking during early infancy were not predictive for bed sharing or night waking during childhood, but bed sharing and night waking during childhood tended to persist over time.11 In contrast, bedtime resistance and difficulties initiating sleep seemed to be transient phenomena at all ages. Another longitudinal study analyzed data of more than 1000 children from the ages of 10 to 13 years.12 This study focussed on children's sleep patterns, but mothers were also asked about the difficulties of initiating sleep of their child. The proportion of children with difficulties initiating sleep significantly diminished from ages 10 to 13 years. The decreasing of sleep problems during childhood was also reported by Gregory et al.13 Sleep problems decreased from the age of 4 years to mid-adolescence. Clarkson et al. described that only 0.3% of the children between 5 to 9 years of age had a sleep problem which persisted over the whole period of the survey.14 In comparison, Strauch et al. reported that the mean frequencies of difficulties initiating sleep among school children aged 10 to 14 years did not change significantly over the period of 5 years.15 However, the individual stability of self-rating was low: 30% of the adolescents reported having difficulties initiating sleep once, 12% twice, 10% three times, 4% four times, and only 2% always. Altogether, there is a lack of longitudinal studies which describe the course of insomnia symptoms in childhood and adolescence in order to emphasize the relevance of these problems for the development in childhood. Discrepancies of self- and parent-reported sleep difficulties16 reveal the need to include both children's and parents' assessments. Owens et al. described that parents underestimate the sleep problems of their children, for example, difficulties initiating sleep and night wakings.17 In addition, Amschler and McKenzie demonstrated that a large number of fifth graders stayed up late without their parents' knowledge and admitted that they woke up during the night regularly without their parents' knowing.18
The Cologne Children's Sleep Study intended to provide information on sleep problems in school-aged children. The present analyses focus on the prevalence and course of sleep disorders in childhood. In detail, longitudinally assessed data were collected from children of the fourth grade of the elementary school; the children were surveyed annually for the subsequent 3 years.
METHODS
Participants
Children of the fourth grade of elementary schools were surveyed from October 2002 to January 2003. All elementary schools in Cologne were asked to participate in the study. Only 2 schools refused to participate (N = 74). A total of 8599 children and their parents received questionnaires, distributed by their teachers; 4563 cases responded. Both questionnaires from parents and child were analyzable from 4531 participants. Consequently, the response rate was 53%. From 3580 families we received their postal address in the first survey so we were able to follow these children over a course of several years. These families were reevaluated one and two years later (February to March 2004 and 2005). The first follow-up included 1125 cases (response rate: 32%), and 1314 cases were included in the second follow-up (response rate: 37%). The higher response rate of the third survey may have been the result of a “reminder” sent to all families 3 weeks after the questionnaire. Parents and their children were requested to fill in and to return the questionnaires. Eight hundred thirty-two families sent back questionnaires from the child and parent with completed information concerning age, sex, and all insomnia items in the first (t1), second (t2), and third (t3) assessment.
The mean age of participating children was 9.4 years (range: 8–11 years) at t1, 10.7 years (range: 9–12 years) at t2, and 11.7 years (range: 10–13 years) at t3. In Germany, children usually start school at the age of 6 to 7. However, some children start as early as 5 and others do not start until 8. For this reason, the age range comprises 4 different age groups. The gender relation was balanced (male 49.4% and female 50.6%).
MATERIALS
Sleep questionnaire (parents and child version)
For the purpose of the study, a sleep questionnaire for children (28 items) and a parental questionnaire (33 items) were developed. In order to maximize the sample, a screening questionnaire was designed which contained few questions but covered as many areas as possible. The items followed a 3-point format (1 = not present, 2 = sometimes, 3 = often). Several areas concerning sleep and waking behavior were elicited: sleep behavior (e.g. regular bedtime, watching TV prior to bedtime, playing computer games prior to bedtime [child version only]), sleep problems (e.g., difficulties initiating and maintaining sleep, nightmares, night terrors, and sleepwalking [both parents version only]), daytime behavior (e.g., daily fatigue), and environmental factors (e.g., noise, light at night). As this screening questionnaire was designed to cover many different symptoms in few questions, there were only 2 questions on difficulties initiating and maintaining sleep: Parent questionnaire, “My child has difficulties initiating sleep” and “My child has difficulties maintaining sleep”; child questionnaire, “I have problems falling asleep in the evening” and “I wake up in the night and find it difficult to get back to sleep.” Demographic data were not collected in order to keep the questionnaire short and more anonymous. In this way, more families were able to be persuaded to participate in the study.
Study Design
Teachers of the fourth grade classes were informed by a leaflet. They distributed the questionnaires and handouts to the parents. The handout informed the parents and requested that they and their child participate in the study. The questionnaires were completed separately at home and anonymously returned to the teacher. At first assessment, the parents were asked to give their post address so they could be contacted at a later stage. Those families who gave us their address were contacted again one year (t2) and 2 years later (t3).
The questionnaire data were analyzed with the statistical software package SPSS 12.0 for Windows. Descriptive methods, Spearman and Pearson correlations, and ANOVA were applied. For some analyses, the rating scale was dichotomized in the following way: “sometimes / often” vs. “not present.” According to the high statistical power resulting from the number of cases included into the analyses, values of P ≤0.01 were ascribed to be significant.
RESULTS
Representativeness of the Sample
Excluded from the study were families who either did not write down their address or did not fill out the questionnaire completely at assessments t1 / t2 / t3. For this reason the longitudinal sample, which consists of all families who completed the questionnaire at all 3 assessments, is much smaller than the total sample at t1. Data about reasons for not completing the questionnaire or not writing down the postal address were not collected. However, it was checked if the families who participated at all assessments were different from the families who did not participate in longitudinal study. Therefore both the longitudinal sample and the total sample were compared at assessment t1 in terms of age, sex, and prevalence of difficulties initiating and maintaining sleep.
The comparisons of the longitudinal sample to the total sample revealed only slight differences of the measured variables (Tables 1 and 2). The total sample (age = 9.48 ± 0.61) had a marginally lower age than the longitudinal sample (age = 9.39 ± 0.56) at t1 (unpaired t-test: t = 5.39, P < 0.000, effect size: d = 0.16). There were no differences concerning gender (total sample: male 48.0% and female 52.0%, longitudinal sample: male 49.3% and female 50.7%; χ2 test, P = 0.42). Concerning insomnia symptoms, there was only a significant difference between self-reports of sleep onset problems. About 40% of the children in the total sample in comparison to about 35% in the longitudinal sample described having sleep onset problems “sometimes” (U-test: z = −3.34, P < 0.01).
Table 1.
Parent-Reported Prevalence of Insomnia Symptoms
| sample | total sample: n = 4474 | longitudinal sample: n = 832 |
||
|---|---|---|---|---|
| Sleep onset problems | t1 | t1 | t2 | t3 |
| often | 6.1 (271) | 5.9 (49) | 4.4 (37) | 4.4 (37) |
| sometimes | 22.4 (1000) | 25.1 (209) | 30.4 (253) | 28.1 (234) |
| no | 71.6 (3203) | 69.0 (574) | 65.1 (542) | 67.4 (561) |
| Difficulties maintaining sleep | t1 | t1 | t2 | t3 |
| often | 2.6 (117) | 1.8 (15) | 2.0 (17) | 1.4 (12) |
| sometimes | 10.8 (485) | 11.3 (94) | 11.9 (99) | 10.8 (90) |
| no | 86.5 (3872) | 86.9 (723) | 86.1 (716) | 87.7 (730) |
Table 2.
Self-reported Prevalence of Insomnia Symptoms
| sample | total sample: n = 4474 | longitudinal sample: n = 832 |
||
|---|---|---|---|---|
| Sleep onset problems* | t1 | t1 | t2 | t3 |
| often | 9.8 (438) | 9.7 (81) | 6.6 (55) | 5.3 (44) |
| sometimes | 34.6 (1549) | 40.6 (338) | 42.9 (357) | 41.3 (344) |
| no | 55.6 (2487) | 49.6 (413) | 50.5 (420) | 53.4 (444) |
| Difficulties maintaining sleep | t1 | t1 | t2 | t3 |
| often | 5.8 (260) | 4.6 (38) | 3.4 (28) | 2.3 (19) |
| sometimes | 20.5 (916) | 23.1 (192) | 23.9 (199) | 21.2 (176) |
| no | 73.7 (3298) | 72.4 (602) | 72.7 (605) | 76.6 (637) |
Dropout and Follow-up sample significantly different at t1 (U-Test; P = 0.001)
Prevalence of Insomnia Symptoms
At t1, 25% of the parents reported that their child “sometimes” and 6% “often” had difficulties initiating sleep. At t2, 30% of the parents reported that their child “sometimes” and 4% “often” had this problem. At t3, the rates were about 30% for “sometimes” and 4% for “often.” Regarding children's ratings, the values were considerably higher: About 40% of the children reported that they “sometimes” and about 10% “often” had difficulties initiating sleep at t1. At t2, about 40% of the children reported that they “sometimes” and 7% “often” had this problem. At t3, the rates were about 40% for “sometimes” and 5% for “often.”
Concerning difficulties maintaining sleep, the prevalence rates were lower: About 10% of the parents reported that their child “sometimes” and 2% “often” had difficulties maintaining sleep at t1. At t2, 12% of the parents reported that their child “sometimes” and 2% “often” had this problem. At t3, the rates were 11% for “sometimes” and 1% for “often.” Regarding children's ratings, the values were higher: 23% of the children reported that they “sometimes” and 5% “often” had difficulties maintaining sleep at t1. At t2, 24% of the children reported that they “sometimes” and 3% “often” had this problem. At t3, the rates were 21% for “sometimes” and 2% for “often.”
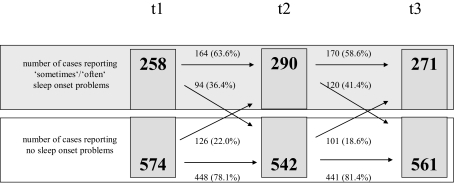
Course of Difficulties Initiating Sleep
Regarding sleep onset problems, the course of sleep behavior of children is illustrated in Figures 1 and 2. Sixty-four percent of the children with difficulties of sleep onset in parental reports had continuing sleep problems one year later (term t2). However, 36% of the participants were characterized by an improvement concerning sleep problems. Similar results were calculated in the comparison between t2 and t3: 59% of the children had ongoing sleep onset problems and 41% did not. Problems falling asleep were obvious in 22% (t2) / 19% (t3) for children without sleep problems at the previous term.
Figure 1.
Parent-reported sleep onset problems from term t1 to term t3 (n = 832).
→Number of cases in which sleep pattern did not change
↘Number of cases in which sleep pattern changed for the positive
↗Number of cases in which sleep pattern changed for the negative
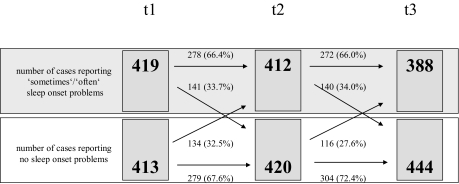
Figure 2.
Self-reported sleep onset problems from term t1 to term t3 (n = 832).
→Number of cases in which sleep pattern did not change
↘Number of cases in which sleep pattern changed for the positive
↗Number of cases in which sleep pattern changed for the negative
Self-reports of children were characterized by almost 65% of the children with ongoing sleep problems between t1 and t2. However, 36% of the participants reported improvement in their sleep problems. Equal results were calculated in the comparison between t2 and t3: 59% of the children were affected by continuing sleep problems and 41% were not. Problems falling asleep were obvious in 22% (t2) / 18% (t3) for children without any sleep problems at term t1 / t2.
The parents who reported sleep onset problems of their child at t1, t2, and t3 were 13.5% (112) of the longitudinal sample. Many parents (376 parents; 45.2%) described no sleep onset problems at all terms. Significant correlations (Spearman Rank correlation) were calculated between t1 and t2 (r = 0.43), between t2 and t3 (r = 0.42), and between t1 and t3 (r = 0.34).
In comparison, 24.0% of the children (200) reported difficulties initiating sleep. Only 25.7% (214) reported no sleep onset problems at all assessments. Significant correlations (Spearman rank correlations) were calculated between t1 and t2 (r = 0.35), between t2 and t3 (r = 0.39), and between t1 and t3 (r = 0.34).
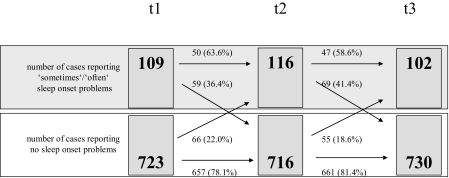
Course of Difficulties Maintaining Sleep
Regarding difficulties maintaining sleep, the course of sleep behavior of the children is illustrated in Figures 3 and 4. Almost 65% of the children with difficulties maintaining sleep in parental reports had continuing sleep problems one year later (term t2). However, more than 35% of the participants were characterized by an improvement concerning sleep problems. Equal results were calculated in the comparison between t2 and t3: almost 60% of the children had ongoing sleep problems and about 40% did not. Difficulties maintaining sleep were obvious in 22% (t2) / 19% (t3) for children without any sleep problems at term t1 / t2.
Figure 3.
Parent-reported difficulties maintaining sleep from term t1 to term t3 (n = 832).
→Number of cases in which sleep pattern did not change
↘Number of cases in which sleep pattern changed for the positive
↗Number of cases in which sleep pattern changed for the negative
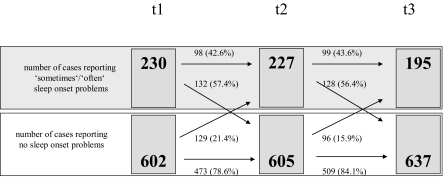
Figure 4.
Self-reported difficulties maintaining sleep from term t1 to term t3 (n = 832).
→Number of cases in which sleep pattern did not change
↘Number of cases in which sleep pattern changed for the positive
↗Number of cases in which sleep pattern changed for the negative
Self-reports of children were characterized by 66% of the children with ongoing sleep problems between t1 and t2. However, the 34% of participants improved their sleep problems. Equal results were calculated in the comparison between t2 and t3: 66% of the children were affected by continuing sleep problems and 34% were not. Difficulties maintaining sleep were obvious in 33% (t2) / 28% (t3) for children without any sleep problems at t1 / t2.
Parents reporting difficulties maintaining sleep at all terms were 3.0% (25) of the sample; 74.2% (617) of the parents described no difficulties maintaining sleep of their child at all terms. Significant correlations (Spearman rank correlations) were calculated between t1 and t2 (r = 0.36), between t2 and t3 (r = 0.35), and between t1 and t3 (r = 0.30).
In comparison, 6.3% (52) of the children reported difficulties maintaining sleep; 49.8% (414) reported no problems at all terms. Significant correlations (Spearman rank correlations) were calculated between t1 and t2 (r = 0.23), between t2 and t3 (r = 0.31), and between t1 and t3 (r = 0.23).
Differences of Child- and Parent-Reported Insomnia Symptoms
The comparison of the child- and parent-reported insomnia symptoms from t1 to t3 clearly indicated that children described difficulties initiating and maintaining sleep more frequently than their parents (P <0.000; effect size: t1 = 0.32, t2 = 0.25, t3 = 0.25). The Pearson correlation was 0.50 at t1, 0.38 at t2, and 0.54 at t3. Moreover, sleep problems decreased marginally over time (P = 0.01). There was also an interaction effect (P <0.01), because parent-reported sleep problems marginally decreased and self-reported sleep problems marginally increased at t2 and decreased at t3.
DISCUSSION
The results of the study indicate that sleep problems in childhood are quite frequent. Difficulties initiating sleep were reported more frequently than difficulties maintaining sleep. In parent reports, 4% to 6% of the children of this age group “often” had difficulties initiating sleep, whereas up to 5% to 10% of the children reported difficulties initiating sleep. About 40% of the children reported difficulties initiating sleep which occur “sometimes,” compared to 25% to 30% of the parents. However the prevalence rates in both child and parent reports concerning difficulties maintaining sleep are about 5% “often” and 10% to 20% “sometimes.” Overall, the prevalence rates are comparable to other studies taking into account the different measurement instruments.1,8
Difficulties initiating and maintaining sleep can be categorized into 2 groups: children with transient symptoms of insomnia at only one of the 3 measurement times, and children with persistent sleep problems. Sleep onset problems in all surveys were present in 13.5% of the children according to the parents' ratings and 24% of the children according to the children's ratings. In child and parent reports about 30% to 40% of the children who had sleep onset problems did not describe any sleep problems one year later. In the parent reports, the percentage of children improving their sleep onset behavior during one year is marginally higher than the child reports, whereas the percentage of children who develop difficulties initiating sleep during one year is about 20% lower in parent reports than in child reports (approximately 30%). Overall, the results indicate that in child and parent reports, more children improve their sleep onset behavior than become worse during one year. Nevertheless, about 60% of the children reported continuing sleep problems longer than one year.
Difficulties maintaining sleep are less common. In self reports about 40% (parent-reported about 60%) describe ongoing difficulties maintaining sleep one year later. More than 55% of the children described improved sleep maintenance after one year, whereas only about 35% to 40% of the parents reported that the difficulties maintaining sleep disappeared one year later. About 20% of those children who have no difficulties maintaining sleep developed difficulties maintaining sleep one year later in parent and child reports. Difficulties maintaining sleep are less common than difficulties initiating sleep, and the results indicate that children of this age group have a higher risk of developing difficulties initiating sleep than difficulties maintaining sleep during one year.
Three percent (parent-reported) versus 6% (self-reported) of the children had difficulties maintaining sleep at t1, t2 and t3. Hence, almost a quarter of the children of the fourth grade with moderate and frequent difficulties initiating sleep describe difficulties initiating sleep 1 and 2 years later. This does not correspond with the results of Jenni et al.11 In their study, sleep-onset difficulties seemed to be a transient phenomenon for most of the children, and night waking tended to persist during childhood. Our findings indicate that difficulties initiating sleep are not transient, even if a high percentage of children improve their sleep pattern after one year. Nevertheless, the results agree with Strauch et al.15: the overall stability of sleep problems in childhood is low.
Some studies describe decreasing sleep problems in childhood.12,13 Our results show only a slight decline in insomnia symptoms. Mild to severe sleep problems are often present regardless of the age of the child.
One of the striking results of the study is the difference between the children and parents in the assessment of sleep problems. Children described significantly more difficulties initiating and maintaining sleep than their parents. These findings are supported by other studies17 and imply that in epidemiological studies and in practical work the inclusion of children's and adolescents' self-reports is necessary. This also corresponds to findings in epidemiological studies concerning scales measuring a variety of children's behaviors.19 It might be that parents are not informed about the sleep problems by their child. On the other hand, it might be that children in this age range have difficulties estimating the severity of their sleep problems along the categories given in the questionnaire (not present, sometimes, often). The questionnaire was designed to elicit sleep problems present during the previous 3 months. Parents may have fewer problems assessing sleep problems in consideration of this long time interval.
One of the limitations of the study is the large dropout rate from t1 to t2. Unfortunately, there is no information about the reasons why these families did not participate in the longitudinal study. However, we were able to demonstrate that the longitudinal sample was comparable to the total sample regarding the sociodemographic and sleep variables. Furthermore, with more than 800 children, the size of the longitudinal sample is still large. Another limitation of the study is the lack of detailed demographic data. The questionnaire does not include questions about social or cultural background. The decision was made not to ask for this information in order to keep the questionnaire short and in order to motivate more families to participate in the study. The questionnaire itself had some limitations. As it has been designed as screening instrument, a large number of symptoms concerning different sleep problems were included, and thus does not allow the computation of sum scores over several items measuring the same problem. For the topic of the present study (difficulties in initiating and maintaining sleep), there were only 2 questions measuring these problems. In addition, the categories (not present, sometimes, often) are not very precise, and it would be preferable to develop categories with distinct frequencies, e.g., once a week, several times a week, and so on. Another limitation of the study is that the assessments did not take place in the same time of year. The second and the third assessments took place in autumn and winter, whereas the first assessment took place in winter and spring. Epidemiological studies could show that adults have more sleep problems in the summer.20 Lower prevalence rates of the second and the third assessment might be partly explained by the different seasons. This, however, strengthens the finding that sleep problems do not decrease with age.
Future studies are needed to look into the specific conditions which might cause chronic sleep problems. Several studies showed associations between sleep disorders and behavior problems.21–25,16
Our present results underline the importance of having treatment concepts available for children and adolescents with insomnia sleep disorders. Stores, Mindell and Owens provided guidelines for treating sleep disorders in children and adolescents.26,27 Moreover, Fricke and Lehmkuhl developed a psychological treatment program for children and adolescents with insomnia and parasomnia (nightmares, night terror, sleep walking).28 Very few studies have evaluated the effects of the treatment methods in this age group systematically.29–31
In summary, sleep problems in childhood and adolescence are a frequent and not always transient phenomenon. Sleep problems decrease only marginally with age; sleep problems might become chronic, requiring medical and psychological treatment. In clinical practice, children and adolescents should be included in the diagnostic and therapeutic process, as many parents seem to underestimate the severity of their children's sleep problems.
ACKNOWLEDGMENTS
We gratefully indicate that our work was supported by the Imhoff Foundation.
Footnotes
Disclosure Statement
This was not an industry supported study. The authors have reported no financial conflicts of interest.
REFERENCES
- 1.Spruyt K, O'Brien LM, Cluydts R, Verleye GB, Ferri R. Odds, prevalence and predictors of sleep problems in school-age normal children. J Sleep Res. 2005;14:163–76. doi: 10.1111/j.1365-2869.2005.00458.x. [DOI] [PubMed] [Google Scholar]
- 2.Wiater AH, Mitschke AR, von Widdern S, Fricke L, Breuer U, Lehmkuhl G. Sleep disorders and behavioural problems among 8- to 11-year-old children. Somnologie. 2005;9:210–4. [Google Scholar]
- 3.Ipsiroglu PS, Fatemi A, Werner I, Tiefenthaler M, Urschitz MS, Schwarz B. Prevalence of sleep disorders in school children between 11 and 15 years. Wiener klinische Wochenschrift. 2001;113:235–44. [PubMed] [Google Scholar]
- 4.Blader JC, Koplewicz HS, Abikoff H, Foley C. Sleep problems of elementary children. Arch Pediatr Adolesc Med. 1997;151:473–80. doi: 10.1001/archpedi.1997.02170420043007. [DOI] [PubMed] [Google Scholar]
- 5.Ipsiroglu PS, Fatemi A, Werner I, Paditz E, Schwarz B. Self-reported organic and nonorganic sleep problems in schoolchildren aged 11 to 15 years in Vienna. J Adolesc Health. 2002;31:436–42. doi: 10.1016/s1054-139x(02)00423-8. [DOI] [PubMed] [Google Scholar]
- 6.Kraenz S, Fricke L, Wiater A, Mitschke A, Breuer U, Lehmkuhl G. Prevalence and influencing factors of sleep disturbances in children just starting school. Praxis der Kinderpsychologie und Kinderpsychiatrie. 2004;53:3–18. [PubMed] [Google Scholar]
- 7.Archbold KH, Pituch KJ, Panabi P, Chervin RD. Symptoms of sleep disturbances among children at two general pediatric clinics. J Pediatr. 2002;140:97–102. doi: 10.1067/mpd.2002.119990. [DOI] [PubMed] [Google Scholar]
- 8.Liu X, Liu L, Owens JA, Kaplan DL. Sleep patterns and sleep problems among schoolchildren in the United States and China. Pediatrics. 2005;155:241–9. doi: 10.1542/peds.2004-0815F. [DOI] [PubMed] [Google Scholar]
- 9.Johnson EO, Roth T, Schultz L, Breslau N. Epidemiology of DSM-IV insomnia in adolescence: lifetime prevalence, chronicity, and an emergent gender difference. Pediatrics. 2006;117:e247–56. doi: 10.1542/peds.2004-2629. [DOI] [PubMed] [Google Scholar]
- 10.Liu X, Uchiyama M, Okawa M, Kurita H. Prevalence and correlates of self-reported sleep problems among Chinese adolescents. Sleep. 2000;23:27–34. [PubMed] [Google Scholar]
- 11.Jenni OG, Fuhrer HZ, Iglowstein I, Molinari L, Largo RH. A longitudinal study of bed sharing and sleep problems among Swiss children in the first 10 years of life. Pediatrics. 2005;115:233–40. doi: 10.1542/peds.2004-0815E. [DOI] [PubMed] [Google Scholar]
- 12.Laberge L, Petit D, Simard C, Vitaro F, Tremblay RE, Montplaisir J. Development of sleep patterns in early adolescence. J Sleep Res. 2001;10:59–67. doi: 10.1046/j.1365-2869.2001.00242.x. [DOI] [PubMed] [Google Scholar]
- 13.Gregory AM, O'Connor TG. Sleep problems in childhood: a longitudinal study of developmental change and association with behavioral problems. J Am Acad Child and Adolesc Psychiatry. 2002;41:964–71. doi: 10.1097/00004583-200208000-00015. [DOI] [PubMed] [Google Scholar]
- 14.Clarkson S, Williams S, Silva PA. Sleep in middle childhood – a longitudinal study of sleep problems in a large sample of Dunedin children aged 5–9 years. Aust Paediatr J. 1986;22:31–5. doi: 10.1111/j.1440-1754.1986.tb00179.x. [DOI] [PubMed] [Google Scholar]
- 15.Strauch I, Meier B, Kaiser F. Developmental aspects of sleep onset insomnia in adolescents. In: Koella WP, Rüther E, Schulz H, editors. Sleep '85. Stuttgart: Fischer; 1985. pp. 386–8. [Google Scholar]
- 16.Paavonen EJ, Aronen ET, Moilanen I, et al. Sleep problems of school-aged children: a complementary view. Acta Paediatr. 2000;89:223–8. doi: 10.1080/080352500750028870. [DOI] [PubMed] [Google Scholar]
- 17.Owens JA, Spirito A, McGuinn M, Noble C. Sleep habits and sleep disturbance in elementary school-aged children. J Dev Behav Pediatr. 2000;21:27–36. doi: 10.1097/00004703-200002000-00005. [DOI] [PubMed] [Google Scholar]
- 18.Amschler DH, McKenzie JF. Elementary students' sleep habits and teacher observations of sleep-related problems. J Sch Health. 2005;75:50–6. doi: 10.1111/j.1746-1561.2005.tb00010.x. [DOI] [PubMed] [Google Scholar]
- 19.Plück J, Döpfner M, Berner W, et al. Die Bedeutung unterschiedlicher Informationsquellen bei der Beurteilung psychischer Störungen im Jugendalter – ein Vergleich von Elternurteil und Selbsteinschätzung Jugendlicher. Praxis der Kinderpsychologie und Kinderpsychiatrie. 1997;46:566–82. [PubMed] [Google Scholar]
- 20.Ohayon MM, Partinen M. Insomnia and global sleep dissatisfaction in Finland. J Sleep Res. 2002;11:339–46. doi: 10.1046/j.1365-2869.2002.00317.x. [DOI] [PubMed] [Google Scholar]
- 21.Gregory AM, Thalia CE, O'Connor TG, Plomin R. Etiologies of associations between childhood sleep and behavioral problems in a large twin sample. J Am Acad Child and Adolesc Psychiatry. 2004;43:744–51. doi: 10.1097/01.chi/0000122798.47863.a5. [DOI] [PubMed] [Google Scholar]
- 22.Chervin RD, Dillon JE, Archbold KH, Ruzicka DL. Conduct problems and symptoms of sleep disorders in children. J Am Acad Child and Adolesc Psychiatry. 2003;42:201–8. doi: 10.1097/00004583-200302000-00014. [DOI] [PubMed] [Google Scholar]
- 23.Lam P, Hiscock H, Wake M. Outcomes of infant sleep probems: a longitudinal study of sleep, behavior, and maternal well-being. Pediatrics. 2003;111:e203–7. doi: 10.1542/peds.111.3.e203. [DOI] [PubMed] [Google Scholar]
- 24.Stein MA, Mendelsohn J, Obermeyer WH, Amromin J, Benca R. Sleep and behavior problems in school-aged children. Pediatrics. 2001;107:1–9. doi: 10.1542/peds.107.4.e60. [DOI] [PubMed] [Google Scholar]
- 25.Aronen ET, Paavonen EJ, Fjällberg M, Soininen M, Törrönen J. Sleep and psychiatric symptoms in school-age children. J Am Acad Child and Adolesc Psychiatry. 1999;39:502–8. doi: 10.1097/00004583-200004000-00020. [DOI] [PubMed] [Google Scholar]
- 26.Stores G. A clinical guide to sleep disorders in children and adolescents. Cambridge: Cambridge University Press; 2001. [Google Scholar]
- 27.Mindell JA, Owens JA. Philadelphia: Lippincott, Williams – Wilkins; 2003. A clinical guide to pediatric sleep. [Google Scholar]
- 28.Fricke L, Lehmkuhl G, editors. Göttingen: Hogrefe; 2006. Schlafstörungen im Kindes- und Jugendalter – Ein Therapiemanual für die Praxis. [Google Scholar]
- 29.Fricke L, Mitschke A, Wiater A, Lehmkuhl G. A new treatment program for children with sleep disorders – concept, practicability, and first empirical results. Praxis für Kinderpsychologie und Kinderpsychiatrie. 2006;55:141–54. [PubMed] [Google Scholar]
- 30.Eckerberg B. Treatment of sleep problems in families with young children: effects of treatment on family well-being. Acta Paediatr. 2004;93:126–34. doi: 10.1080/08035250310007754. [DOI] [PubMed] [Google Scholar]
- 31.Mindell JA. Empirically supported treatments in pediatric psychology: bedtime refusal and night wakings in young children. J Pediatr Psychol. 1999;24:465–81. doi: 10.1093/jpepsy/24.6.465. [DOI] [PubMed] [Google Scholar]