To what extent can a state legitimately restrict the liberties of its citizens in order to serve the common good? Furthermore, to what extent has the protection of the public's welfare been a pretext for governments to curtail or erode fundamental rights? These questions have formed the foundation of controversies and long-running debates about public health in the USA; conflicts that have been animated by a deep-rooted mistrust of overreaching authorities, concerns about arbitrary exercises of power, and by the anti-authoritarian ethos that is a historically prominent feature of US politics and civic culture.
The first tensions over the scope of public health and the acceptability of its measures arose during the fight against infectious disease in the nineteenth and early twentieth centuries. They resurfaced in the last decades of the twentieth century in the wake of efforts to address chronic conditions that began to inform the pattern of morbidity and mortality in industrial societies. They reveal an enduring tension between public health and individual rights—a tension that we ignore at our own peril.
Scientific advances in Europe during the nineteenth century, notably in the laboratories of Louis Pasteur (1822–1895) and Robert Koch (1843–1910), identified the causative agents of many infectious diseases. This ‘bacteriological revolution' transformed our understanding of how disease spreads and laid the foundations for a new public health ethos (Baldwin, 1999). In this regard, it is worth noting that the discoveries of infectious bacteria by Pasteur and Koch provoked sharp resistance in those nations that were concerned about whether and how the imposition of quarantines would interrupt the free movement of goods and people (Ackerknect, 1948).
Early advocates of public health in the USA, such as Mitchell Prudden (1849–1924) and Hermann Biggs (1859–1923), who was general medical officer of the city of New York's (NY, USA) Department of Health in the late nineteenth and early twentieth centuries, were unabashed as they defended the legitimacy of coercion in the face of public health threats. “[E]verything”, said Biggs when talking about efforts to curtail tuberculosis, “which is detrimental to health or dangerous to life, under the freest interpretation, is regarded as coming within the province of the Health Department. So broad is the construction of the law that everything which improperly or unnecessarily interferes with the comfort or enjoyment of life, as well as those things which are, strictly speaking, detrimental to health or dangerous to life, may become the subject of action on the part of the Board of Health.” Looking back almost a century later, Laurie Garrett commented in her book, Betrayal of Trust: The Collapse of Global Public Health, that, “[i]t was a declaration of war, not just against tuberculosis but against any group or individual who stood in the way of Public Health or the sanitarians' Hygeia” (Garrett, 2000).
…the often abysmal health situations in the rapidly growing cities of the USA and Europe required drastic measures, and public health officials were given the freedom to meet the problems…
Biggs was but the most articulate of the new cadre of public health officials who endorsed authoritarian attitudes in the name of public health; the often abysmal health situations in the rapidly growing cities of the USA and Europe required drastic measures, and public health officials were given the freedom to meet the problems with what, at times, were heavy-handed approaches. In turn, these provoked resistance to mandatory vaccination programmes, quarantines and surveillance. Efforts to control smallpox, which involved compulsory vaccination, acted as a rallying point for groups and individuals motivated both by anti-government ideology and concrete fears of the physical harm that sometimes resulted from the procedure. Anti-vaccine organizations throughout the USA were driven, among other things, by opponents of germ theory and groups generally opposed to government interference in their claims to privacy. In Milwaukee (WI, USA), for example, forceful application of the State's mandatory vaccination law sparked riots among the city's large German immigrant population in the 1890s. Health officers who went into neighbourhoods to vaccinate residents and remove sick individuals to quarantine hospitals were greeted by angry mobs throwing rocks (Colgrove, 2006).
In the state of Massachusetts (USA), a smallpox epidemic during the winter of 1901 provided the occasion for a legal challenge to the state's compulsory vaccination law. This led to a landmark ruling by the US Supreme Court in the case of Jacobson versus Commonwealth of Massachusetts, which established the government's right to use its ‘police powers' in order to control epidemic disease. In its seven-to-two decision, the Court affirmed the right of the people, through their elected representatives, to enact “health laws of every description to protect the common good” (Colgrove & Bayer, 2005).
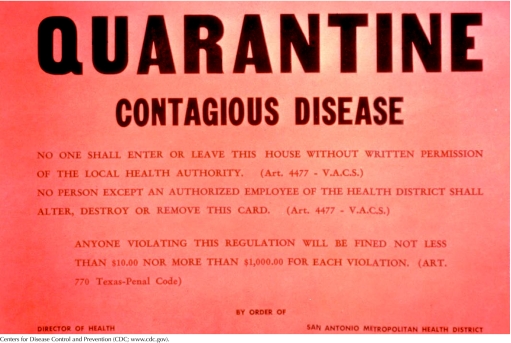
Efforts to impose quarantines on those viewed as a threat to public health has involved the use of measures that look excessive and profoundly unfair from the perspective of less troubled times. On several occasions, the outbreak of diseases among disfavoured minority groups has led to harsh measures being used against them. As Howard Markel noted in his book, Quarantine!, “[i]mmigrants arriving in New York City in 1892, for example, could be isolated and kept in squalid conditions to prevent the spread of cholera and typhus. At a time of massive immigration and concomitant nativist sentiment, health officials faced little popular opposition to their efforts” (Markel, 1997).
US courts have almost always deferred to public health authorities that have deprived individuals of their liberty in the name of public health
A central strategy of the emergent public health regime in the nineteenth and early twentieth centuries involved the mandatory reporting of patients' names to public health registries. Physicians attending patients in private practices often opposed such requirements as impinging on their autonomy and as a violation of the doctor–patient relationship. Biggs, when reflecting on the controversies that had greeted his efforts to mandate the reporting of tuberculosis cases—as he moved forward to begin the surveillance of sexually transmitted diseases in the early twentieth century—remarked that, “[t]he ten year long opposition to the reporting of tuberculosis will doubtless appear a mild breeze compared with the stormy protest against the sanitary surveillance of the venereal diseases” (Biggs, 1913). Despite the existence of much opposition, the reporting of cases by name to local and state health departments and to special confidential registries ultimately became part of the tradition and practice of public health.
US courts almost always deferred to public health authorities that have deprived individuals of their liberty in the name of public health. One US state high court declared at the beginning of the twentieth century that, “[i]t is unquestionable that the legislature can confer police powers upon public officers for the protection of the public health. The maxim Salus populi suprema lex is the law of all courts in all countries. The individual right sinks in the necessity to provide for the public good” (Parmet, 1985). Even more remarkably, a plenary grant of authority was still found to be constitutional in the 1960s. In upholding the detention of a person with tuberculosis pursuant to a statute that provided virtually no procedural protections, a California appellate court declared in 1966 that, “[h]ealth regulations enacted by the state under its police power and providing even drastic measures for the elimination of disease...in a general way are not affected by constitutional provisions, either of the state or national government.”
The breadth of powers that public health authorities had enjoyed remained virtually unchallenged through most of the twentieth century, but finally came under increasing scrutiny during the last decades of that era. The development of a robust jurisprudence of privacy, and the “due process revolution”, which extended rights to prisoners, mental patients and others under the authority of the state, ultimately questioned the long-held assumptions that had protected public health from constitutional scrutiny. The groundwork for this profound change was laid in the transformations that occurred in American politics, law and culture during the 1960s and 1970s. But it was the HIV/AIDS epidemic that forced a fundamental rethinking of the dominant ideology of public health. The methods of mandatory screening and examination, reporting the names of those who were sick or infected to public health registries and the imposition of quarantine once again became the subject of controversy and dispute (Bayer, 1989).
The debates that raged during the 1980s when HIV/AIDS emerged in the USA revealed the profound influence that political and historical contexts had had on the enforcement of public health. In the early years of the epidemic, a broad coalition of gay rights' activists and advocates of civil liberties were largely successful in their efforts to put the protection of privacy and individual rights at the forefront of the public health agenda. Fierce battles ensued when proposals were made to mandate the reporting of people infected with HIV to public health registries, and it was not until many years later that such reporting became universal. Intense controversy also surrounded the efforts to preserve the right of individuals to determine whether they would be tested for HIV infection. Newly adopted policies required exacting and specific informed consent for testing, and it was not until the 1990s that significant support among physicians emerged to help relax these standards. Finally, every attempt to use the power of quarantine to control those whose behaviour might place their sexual partners at risk provoked extensive debate about the counterproductive impact of recourse to coercion.
The HIV/AIDS epidemic provided the occasion to articulate a new paradigm of public health
The HIV/AIDS epidemic provided the occasion to articulate a new paradigm of public health. Given the biological, epidemiological and political factors that shaped the public policy discussion, proponents and defenders of civil liberties were able to assert that no tension existed between public health and civil liberties, that policies that protected the latter would foster the former and that policies that intruded on rights would subvert public health. What was true for HIV/AIDS was also true for public health generally. Indeed, the experience of dealing with HIV/AIDS provided the opportunity to rethink the very foundations of public health and to re-examine the legacy of compulsory state powers. Even when some elements of the privacy- and rights-based approaches to HIV/AIDS were modified in the 1990s as the epidemic ‘normalized', the core values of privacy and civil liberties that had taken hold retained their influence.
But is it true that there is no tension between public health and civil liberties? Public health surveillance for both infectious and non-infectious diseases is crucial in order to understand the patterns of diseases, and for the planning and execution of remedial action. This is true for tuberculosis, as it is true for cancer (Fairchild et al, 2007). Surveillance, to be effective, necessitates that either physicians or laboratories comply with public health mandates that clearly intrude on privacy. Only if we acknowledge this fact can we determine whether the public health benefits of surveillance justify this price.
 |
Mandatory immunization of school children clearly intrudes on or burdens parental autonomy. Yet, both the protection of children from infectious disease and the ensuing ‘herd immunity' by high-level vaccination coverage, which protects those who cannot be vaccinated, depend on such mandates. Various outbreaks of measles and pertussis (whooping cough) underscore the toll that we have to pay when we privilege parental choice; it might be a cost worth bearing but we will only know if we are forced to acknowledge the trade-offs involved.
Another central tenet of public health is the requirement that people with certain diseases undergo treatment—as in the case of tuberculosis—or that people with highly infectious diseases be isolated or quarantined. Such measures always require that we address questions of whether the health threats, their severity and transmissibility all justify depriving individuals of their liberty. These questions cannot be answered without confronting the tension between the interests of the individual and those of the collective. If SARS (severe acute respiratory syndrome) taught us anything, it was how difficult it is to make such decisions in the face of uncertainty. It might turn out in retrospect that the quarantines we impose when faced with a potential epidemic are more extensive than necessary. But in the face of an evolving threat, public health officials have no choice but to weigh personal liberty against potential grave threats (Gostin et al, 2003).
To this point I have focused on infectious diseases, which compel us to address the powers of public health when there is a direct risk or a potential risk to third parties. But the scope of public health in industrial and post-industrial societies extends to chronic diseases (Knowles, 1977). Many such conditions involve lifestyle choices; patterns of behaviour which, in the first instance, harm oneself. What is the legitimate role of the state in modifying, discouraging, burdening or even prohibiting behaviours that increase both morbidity and mortality?
At stake here is the question of paternalism. Is it appropriate for the State to impose restrictions on competent adults in order to protect them from harming themselves? Those who are inspired by the tradition of John Stuart Mill answer with a resounding ‘No'. They claim that public health officials can educate and warn, but not compel. As these ideas have gained wide influence, advocates of public health often need to assert that they intervene because the social consequences or negative externalities of certain behaviours warrant intervention; thus, self-regarding harms are transformed into other-regarding harms. In any event, the state seeks to use its authority to change individual behaviour.
Two examples will illustrate this point. It has long been known that wearing helmets drastically decreases a motorcyclist's risk of death or severe injury in the case of an accident. During the 1970s, pressure by the federal government in the USA led virtually all states to mandate the use of motorcycle helmets (Jones & Bayer, 2007). These statutes provoked the wrath of motorcyclists who asserted that the state deprived them of the right to cycle in the way that was most pleasurable and exciting, and that failure to use helmets posed no threat to others. In short, these laws were, they asserted, an example of overreaching state intrusion, of gross paternalism. Nevertheless, when the courts reviewed these statutes, they were almost never overturned as unconstitutional. A court in Massachusetts noted, “From the moment of the injury, society picks the person up off the highway; delivers him to a municipal hospital and municipal doctors; provides him with unemployment compensation if, after recovery, he cannot replace his lost job; and if the injury causes permanent disability many assure the responsibility for his and his family's continued sustenance. We do not understand a state of mind that permits a plaintiff to think that only he himself is concerned” (Cronin, 1980).
What is the legitimate role of the state in modifying, discouraging, burdening or even prohibiting behaviours that increase both morbidity and mortality?
Although efforts to justify the regulation of behaviour in non-paternalistic terms might be effective in the short term, they are almost always transparent subterfuges. It would be more honest—and in the long term more protective of public health—to acknowledge that intervention is sometimes necessary to protect individuals from their own foolish or dangerous behaviour because such efforts can have a broad and enormous impact at a population level. An explicit acknowledgement would also help to understand the trade-offs involved. Ironically, the use of the social impact argument can, in the end, be more subversive of rights than the explicit embrace of paternalism. After all, everything can be shown to have a social impact.
The failure to make a strong case for paternalistic restrictions with regard to motorcycle helmets set the stage for repeals of compulsory helmet laws for adults; now, only half the states have such statutes. The consequences were predictable: in 2004, approximately 4,000 cyclists died, the seventh year to show an increase in fatalities. The triumph of individual rights has transformed a public health success story into a public health defeat. Recognizing the right to ride a motorcycle without a helmet might be a right we want to protect—but there should be no confusion about the price we pay.
The case of tobacco control gives more reason for optimism (Feldman & Bayer, 2004), but here too, recent history underscores that achievements in public health often carry a price in individual freedom. It would be convenient to think about tobacco as similar to other environmental toxins, which we simply ban when we find that they cause morbidity and mortality; however, tobacco is different. Millions consume it because of addiction, habit, desire or social convention. It is therefore impossible to consider public policy without addressing the extent to which the state might exert pressure and impose limits in the name of health. The answer to this question will determine whether we will be able to save the lives of smokers both now and in the future.
It is striking that in most economically advanced democracies, the first decades of tobacco control were marked by a distinct reluctance to embrace measures that bore the taint of paternalism—especially in the USA. Pressure from the tobacco industry and its allies partly accounted for this phenomenon, but they do not provide a sufficient explanation. Here, as in the case of motorcycle helmets, there was considerable uncertainty about how far the state could go. As a consequence, much of public health policy focused on children and innocent bystanders.
When limits were proposed on tobacco advertising—a unique problem in the USA, where the Supreme Court has extended the protections of the First Amendment to commercial speech—they were commonly justified by the need to protect children from the seductions of tobacco. When arguments were made for radically increasing taxes on cigarettes, thus burdening consumption—especially for those with less disposable income—it was asserted that such levies were vital because of the social costs created by tobacco-associated morbidity and mortality. Finally, when increasingly restrictive measures were imposed on smoking in public settings, the central justification was that passive smoking was pathogenic and responsible for deaths associated with cancer and heart disease. It was almost never asserted that limits on advertising, increases in taxes and restrictions on public smoking were necessary to protect those who might begin to smoke or those who were smokers.
Clearly the public health—measured collectively in terms of the lives of individuals and on a population basis—requires intervention that involves restrictions of choice
As a result of changing social norms and public policies, the prevalence of smoking by adults in advanced democracies has declined markedly in the past 40 years. A steep social gradient has also emerged: those better educated smoke less; those with poorer education comprise an ever-greater proportion of smokers. Under these social conditions, it has become increasingly possible to assert that the aim of restrictive public health policy is to pressure, even cajole, smokers to give up their behaviour. Tobacco advertising must, where permissible, be banned. Taxes must make the price of cigarettes increasingly prohibitive. Limits on public smoking are necessary to make it more difficult for smokers to find a place where they can light up.
Given the human toll caused by tobacco consumption, who then but the most hidebound of libertarians would oppose measures to radically reduce, even end, the scourge associated with cigarette smoking? Clearly the public health—measured collectively in terms of the lives of individuals and on a population basis—requires intervention that involves restrictions of choice.
Across the spectrum of threats to the public health—from infectious diseases to chronic disorders—are inherent tensions between the good of the collective and the individual. To acknowledge this tension is not to foreordain the answer to the question ‘How far should the state go?'; rather, it is to insist that we are fully cognizant of difficult trade-offs when we make policy determinations.

References
- Ackerknect C (1948) Anticontagionism between 1821–1867. Bull History Med 22: 562–593 [PubMed] [Google Scholar]
- Baldwin P (1999) Contagion and the State in Europe 1820–1930. Cambridge, UK: Cambridge University Press [Google Scholar]
- Bayer R (1989) Private Acts Social Consequences: AIDS and the Politics of Public Health. New York, NY, USA: Free Press [Google Scholar]
- Biggs H (1913) The public health. Monthly Bulletin of the Department of Health of the City of New York 1913: 136 [Google Scholar]
- Colgrove J (2006) State of Immunity. Berkeley, CA, USA: University of California Press [Google Scholar]
- Colgrove J, Bayer R (2005) Jacobson v Massachusetts (2005) manifold restraints: liberty, public health, and the legacy of Jacobson v Massachusetts. Am J Public Health 95: 571–576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cronin TE (1980) A resurgent Congress and the Imperial Presidency. Polit Sci Q 95: 209–237 [Google Scholar]
- Fairchild A, Bayer R, Colgrove J (2007) Searching Eyes: Privacy & the State and Disease Surveillance in America. Berkeley, CA, USA: University of California Press [Google Scholar]
- Feldman E, Bayer R (2004) Unfiltered: Conflicts Over Tobacco Policy and Public Health. Cambridge, MA, USA: Harvard University Press [Google Scholar]
- Garrett L (2000) Betrayal of Trust: The Collapse of Global Public Health. New York, NY, USA: Hyperion [Google Scholar]
- Gostin L, Bayer R, Fairchild A (2003) Ethical and legal challenges posed by Severe Acute Respiratory Syndrome: implications for the control of severe infectious disease threats. JAMA 290: 3229–3237 [DOI] [PubMed] [Google Scholar]
- Jones M, Bayer R (2007) Paternalism and its discontents: motorcycle helmet laws, libertarian values, and public health. Am J Public Health 97: 208–217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knowles J (1977) The responsibility of the individual. Daedalus 106: 57–80 [PubMed] [Google Scholar]
- Markel H (1997) Quarantine: East European Jewish Immigrants and the New York City Epidermis of 1892. Baltimore, MD, USA: Johns Hopkins University Press [Google Scholar]
- Parmet W (1985) AIDS and quarantine: the revival of an archaic tradition. Hofstra Law Review 13: 53–90 [Google Scholar]


