Abstract
To evaluate the role of preoperative bone scintigraphy in determining the operative treatment method for femoral neck fracture, we reviewed the data of 83 patients who underwent preoperative bone scanning after femoral neck fracture. Fractures were classified using the Garden staging system. Radioisotope uptake in femoral heads was evaluated visually. Of 28 patients with Garden stage I or II, radioactivity of the femoral head was normal in 26, partially reduced in one, and generally reduced in one patient. Twenty-seven patients were treated by closed reduction and multiple pinning, and one patient was treated by bipolar hemiarthroplasty. Of 55 patients with Garden stage III or IV, femoral-head radioactivity was normal in three, partially reduced in seven and generally reduced in 45 patients. Fifty-four patients were treated by bipolar hemiarthroplasty or total hip arthroplasty, and one patient was treated by closed reduction and multiple pinning. In only one of the 83 cases was the operative method changed because of bone scan findings. Isotope uptake of the femoral head after femoral neck fracture generally corresponded with the degree of fracture displacement. Preoperative bone scans appear to have no significant role to play in determining the operative treatment method for femoral neck fracture.
Résumé
Afin d’évaluer le rôle préopératoire de la scintigraphie osseuse dans les fractures du col du fémur, nous avons revu les dossiers de 83 patients qui ont présenté une fracture du col fémoral. La fracture a été classée selon la classification de Garden. Sur les 28 patients Garden I et II, la réponse scintigraphique de la tête fémorale est normale pour 26 patients, avec une hypofixation osseuse pour un patient et une fixation peu importante chez un autre patient. 27 patients ont été traités par réduction orthopédique et embrochage à foyer fermé, un patient par hémiarthroplastie. Pour les 55 patients présentant une fracture Garden III ou IV, la scintigraphie de la tête fémorale a été normale chez trois patients avec une hypofixation chez 7 patients, une fixation très réduite chez 45 patients. 54 patients ont été traités par hémiarthroplastie ou par prothèse totale et un patient traité par réduction orthopédique et embrochage. Chez un seul des 83 patients, la méthode opératoire a été changée après les constatations scanographiques. La fixation isotopique après fracture du col fémoral correspond tout à fait au degré et au déplacement de la fracture. Le scanner préopératoire ne semble pas avoir d’intérêt pour déterminer le traitement optimum chez ces patients.
Introduction
Femoral neck fracture is still known as “unsolved fracture” because it is frequently complicated by avascular necrosis or non-union [3, 5]. Because of these complications, arthroplasty or internal fixation is frequently performed as a primary treatment. Generally, the degree of fracture displacement and age are the main factors considered when determining the method of operation [13]. In our department, we perform internal fixation for Garden stage I and II femoral neck fractures regardless of patient age. For Garden stage III and IV fractures, we perform arthroplasty for patients older than 65 years, and internal fixation after reduction for younger patients.
Blood supply to the femoral head can be disturbed by a femoral neck fracture due to anatomical characteristics, and this is considered to be a major cause of non-union or avascular necrosis of the femoral head [8, 12]. Thus, if the status of blood flow to the femoral head could be evaluated before surgery, it would be helpful when deciding on the method of operation. Tc-99m methylenediphosphonate (99mTc-MDP) bone scans are used to determine prognosis after internal fixation of femoral neck fractures, because these scans reflect blood flow in bone tissue [1, 4, 7, 11, 14].
In this study, we evaluated the role of preoperative bone scan for determining the operative method for femoral neck fracture.
Materials and methods
Between January 1998 and December 2003, a total of 83 patients with femoral neck fracture had a preoperative bone scintigram. They were 21 men and 62 women with an average age of 67.0 years (range, 18–93 years). The main cause of fracture was a mis-step or a fall. To classify fractures we applied the Garden stage system, which is based on fracture displacement [6, 10].
99mTc-MDP bone scan
Preoperative bone scanning was performed using 99mTc-MDP. Bone scanning was possible only in limited cases, because femoral neck fractures are treated surgically as soon as possible. No operation was delayed in any patient for a bone scan, since only those patients who needed special investigations for problems that might affect anesthesia or surgery received a bone scan.
Four hours prior to bone scanning, patients were injected with 30mCi 99mTc-MDP (Amersham, UK) intravenously. After catheterisation, anterior and posterior scintigrams of the pelvis, including both hips, were obtained using a gamma camera (Siemens, Germany).
The evaluation of bone scans
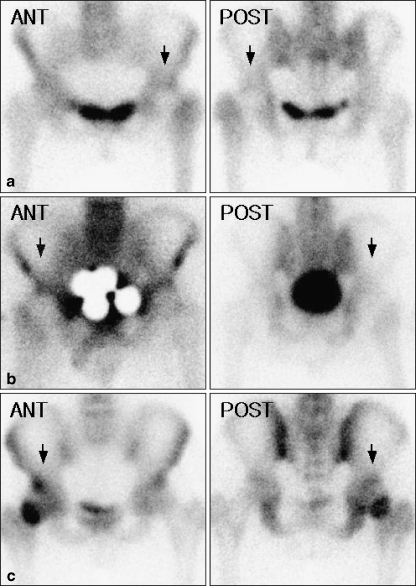
Visual evaluations of radioisotope uptake in femoral heads were performed independently by three orthopaedic surgeons who were unaware of patient clinical information and radiological findings. Uptake in the femoral head on the fractured side was compared with that of the contralateral side and classified as R (reduced uptake in both anterior and posterior views); P (reduced uptake in only one view); and N (normal or increased uptake) (Fig. 1).
Fig. 1.
Categories of radioactivity in the femoral head on the fractured side (arrow). a Radioisotope uptake is reduced in both anterior and posterior views (category R: overall reduction in activity). b Radioisotope uptake is reduced in the anterior or posterior view (category P: partial reduction in activity). c Radioisotope uptake is normal or increased (category N: normal or increased activity)
Results
According to the Garden stage system, there were 27 cases of stage I, one case of stage II, 24 cases of stage III and 31 cases of stage IV.
In general, preoperative radioisotope uptake in the femoral head on the fractured side corresponded with the degree of fracture displacement. There were 28 cases of Garden stages I and II. Radioisotope uptake was N in 26 cases, P in one case, and R in one case (Table 1). In all cases except one, internal fixation with multiple pins was performed. In the remaining Garden stage I case with a radioisotope uptake of R, bipolar hemiarthroplasty was performed after considering the bone scan finding, together with the age of the patient (73 years) (Fig. 2). This is the only case in this series in which the operative method was changed because of bone scan findings. There were 55 cases of Garden stages III and IV. Radioisotope uptake was R in 45 cases, P in seven cases, and N in three cases (Table 1). Of these 55 cases, 48 were treated by bipolar hemiarthroplasty and six by total hip arthroplasty. In one case of Garden stage III with a radioisotope uptake of P, internal fixation with multiple pins was performed because of age (47 years). The fracture healed well, and no evidence of avascular necrosis of the femoral head was detected at 2 years after the operation (Fig. 3). In three cases with radioisotope uptake of N, replacement arthroplasty was performed because of their age (74, 80 and 87).
Table 1.
Qualitative evaluation of preoperative radionuclide deposition in the femoral head for fractured femoral neck
| Garden stage | Femoral head activity | Total | ||
|---|---|---|---|---|
| R | P | N | ||
| I | 1(1*+0) | 1(0+0) | 25(0+0) | 27 |
| II | 0 | 0 | 1(0+1) | 1 |
| III | 15(15+0) | 6(5+1) | 3(3+0) | 24 |
| IV | 30(30+0) | 1(1+0) | 0 | 31 |
| Total | 46 | 8 | 29 | 83 |
(n+n′) : (arthroplasty+internal fixation)
*: Operative method was changed based on the bone scan findings
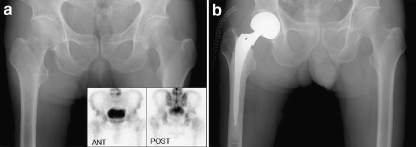
Fig. 2.
A 73-year-old man with a right hip pain. a A preoperative radiograph shows a Garden stage I femoral neck fracture. Bone scan shows overall reduction in radioisotope uptake (category R) in the right femoral head. b Bipolar hemiarthroplasty was performed
Fig. 3.
A 47-year-old man with a left hip pain. a Preoperative radiograph shows a Garden stage III femoral neck fracture. Bone scan shows a partial reduction in radioisotope uptake (category P) in the left femoral head. b A postoperative 2-year follow-up radiograph shows good union of the fracture and no evidence of avascular necrosis
Discussion
Many studies have reported that 99mTc-MDP bone scans are useful for assessing the prognosis of femoral neck fractures. In most studies, bone scans were performed after internal fixation of the fractures. Holmberg and Thorngren reported that if a preoperative bone scan is normal (i.e., the femoral head uptake ratio of the fractured side to the contralateral side is >0.9) then the possibility of complete healing is high [9].
Catto suggested that a displaced fracture has a poorer prognosis than a non-displaced fracture because blood supply to the femoral head is decreased [2]. Our data demonstrate that preoperative isotope uptake was reduced generally or partially in 52 (95%) of 55 fractures of Garden stages III and IV, and that preoperative isotope uptake was normal in 26 (93%) of 28 fractures of Garden stages I and II. In general, femoral head radioisotope uptake coincided with the degree of fracture displacement.
Degree of fracture displacement and patient age are important factors when deciding on the method of operation [13]. However, the criteria used to decide the operative method are so subjective that the result is often one of surgeon’s preference. We also use our own subjective criteria to decide on the operative method; and because we hoped that we could improve the objectivity of decision-making using bone scan results as a guide, we performed this study. However, we found that the method of operative treatment was changed in only one of 83 cases after reviewing preoperative bone scan findings.
One study found that blood flow improves after anatomical reduction of a displaced femoral neck fracture, and recommended anatomical reduction to reduce complications [10]. Thus, blood flow may improve with good reduction, even with poor preoperative bone scan findings. In view of this possibility and the findings of our study, we are forced to conclude that preoperative bone scan has no significant role in deciding on operative method in cases of femoral neck fracture.
Acknowledgement
This work was supported by a grant (No. 06-2003-063) from the Seoul National University Hospital Research Fund.
References
- 1.Bauer G, Weber DA, Ceder L, Darte L, Egund N, Hansson LI, Stromqvist B (1980) Dynamics of technetium-99m methylendiphosphonate imaging of the femoral head after hip fracture. Clin Orthop 152:85–92 [PubMed]
- 2.Catto M (1965) A histological study of avascular necrosis of the femoral head after transcervical fracture. J Bone Joint Surg Br 47:749–776 [PubMed]
- 3.Colemann SS, Comprere CL (1957) Femoral neck fracture. Pathogenesis of avascular necrosis, nonunion, and degenerative change. J Bone Joint Surg Am 39:1419
- 4.D’Ambrosia RD, Riggins RS, Stadalnik RC, Denardo GL (1976) Vascularity of the femoral head. Clin Orthop 121:143–148 [PubMed]
- 5.Dickson JA (1953) The “Unsolved” fracture. J Bone Joint Surg Am 35:805–822 [PubMed]
- 6.Garden RS (1961) Low-angle fixation in fractures of the femoral neck. J Bone Joint Surg Br 43:647–663
- 7.Greiff J, Lanng S, Höilund-Carlsen PF, Karle AK, Uhrenholdt A (1980) Early detection by 99mTc-Sn-pyrophophonate scintimetry of femoral head necrosis following medical femoral neck fracture. Acta Orthop Scand 51:119–125 [DOI] [PubMed]
- 8.Hoaglund FT, Low WD (1980) Anatomy of the femoral neck and head, with comparative data from Caucasians and Hong Kong Chinese. Clin Orthop 152:10–16 [PubMed]
- 9.Holmberg S, Thorngren KG (1984) Preoperative 99mTc-MDP scintimetry of femoral neck fracture. Acta Orthop Scand 55:430–435 [DOI] [PubMed]
- 10.Kyle RF, Cabanela ME, Russell TA, Swiontkowski MF, Winquist RA, Zuckerman JD, Schmidt AH, Koval KJ (1995) Fractures of the proximal part of the femur. Instr Course Lect 44:227–253 [PubMed]
- 11.Lewis SL, Rees JI, Thomas GV, Willians LA (1991) Pitfalls of bone scintigraphy in suspected hip fractures. Br J Radiol 64:403–408 [DOI] [PubMed]
- 12.Lucie RS, Fuller S, Burdick DC, Johnston RM (1981) Early prediction of avascular necrosis of the femoral head following femoral neck fractures. Clin Orthop 161:207–214 [PubMed]
- 13.Shah AK, Eissler J, Radomisli T (2002) Algorithms for the treatment of femoral neck fractures. Clin Orthop 399:28–34 [DOI] [PubMed]
- 14.Strömqvist B, Brismar J, Hansson LI, Palmer J (1984) Technetium-99m-methylediphosphonate scintimetry after femoral neck fracture. A three-year follow-up study. Clin Orthop 182:177–189 [PubMed]