Abstract
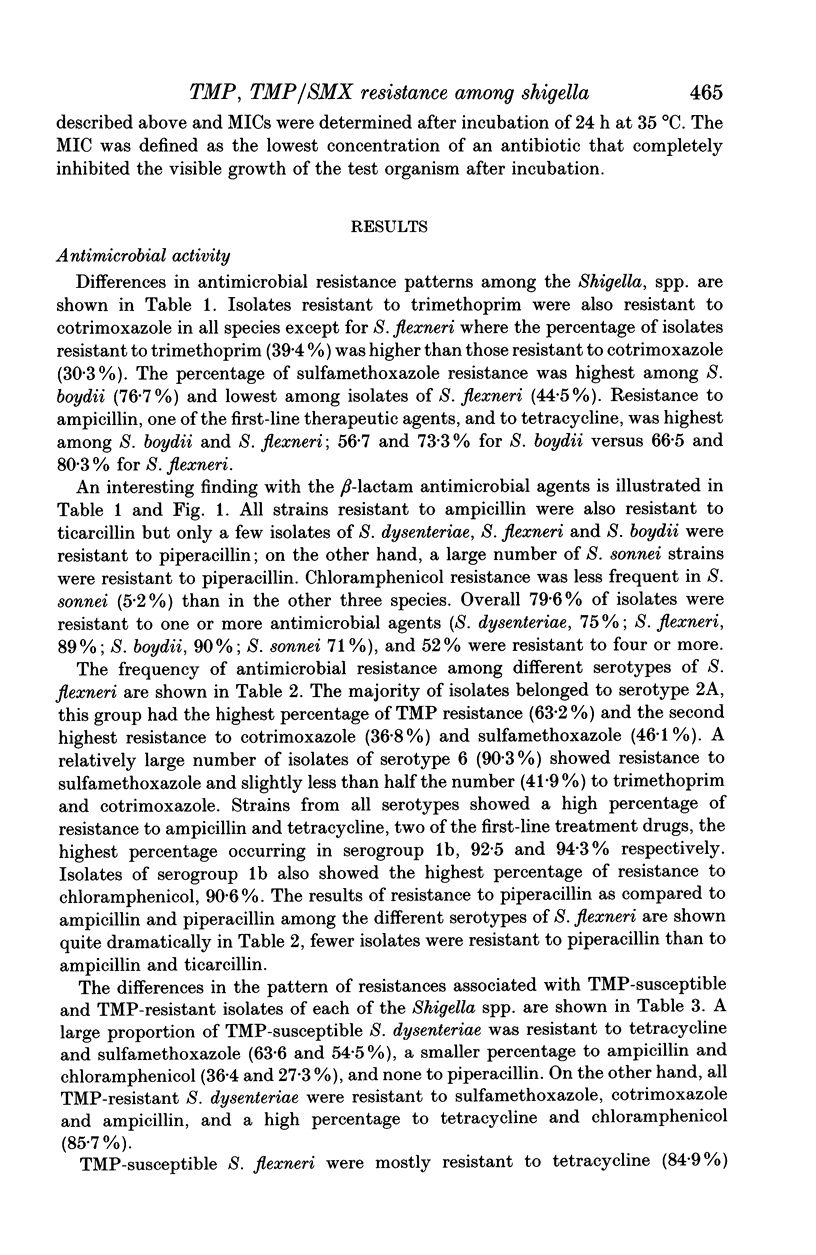
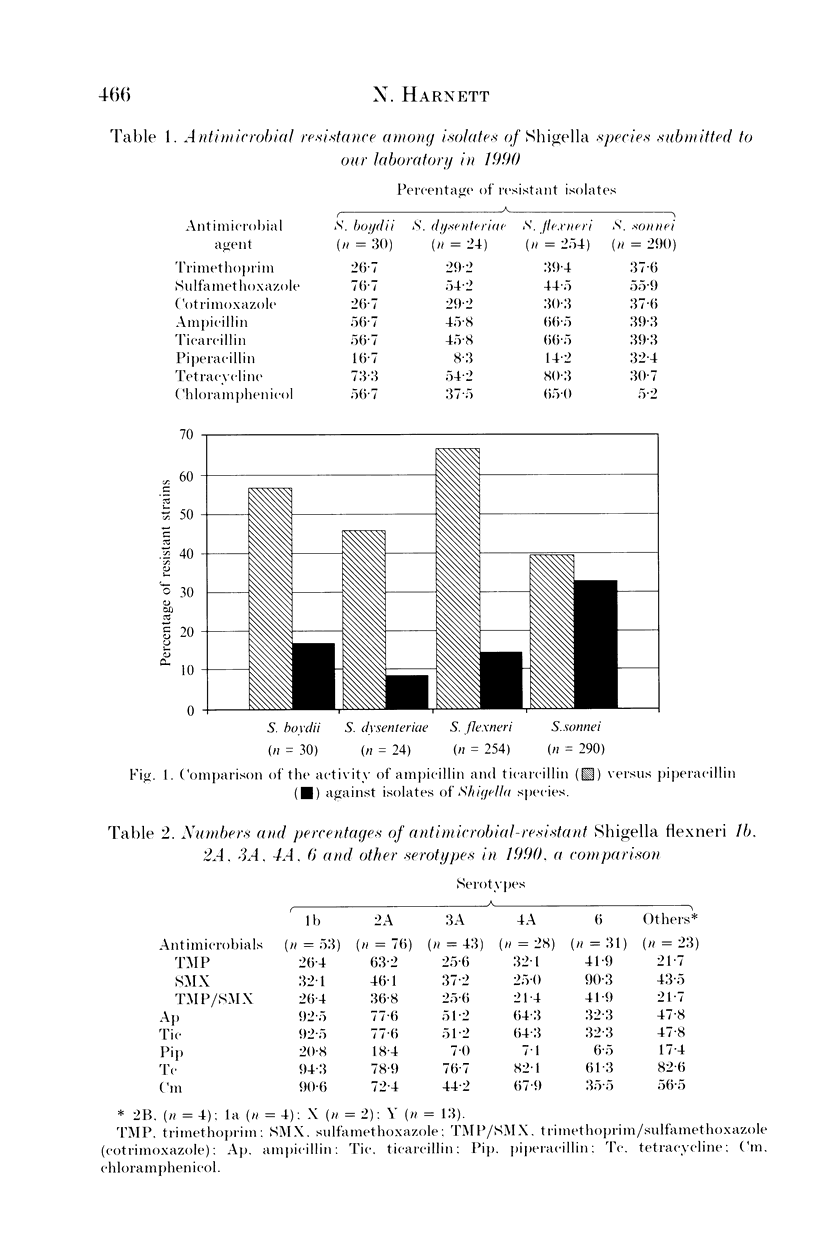
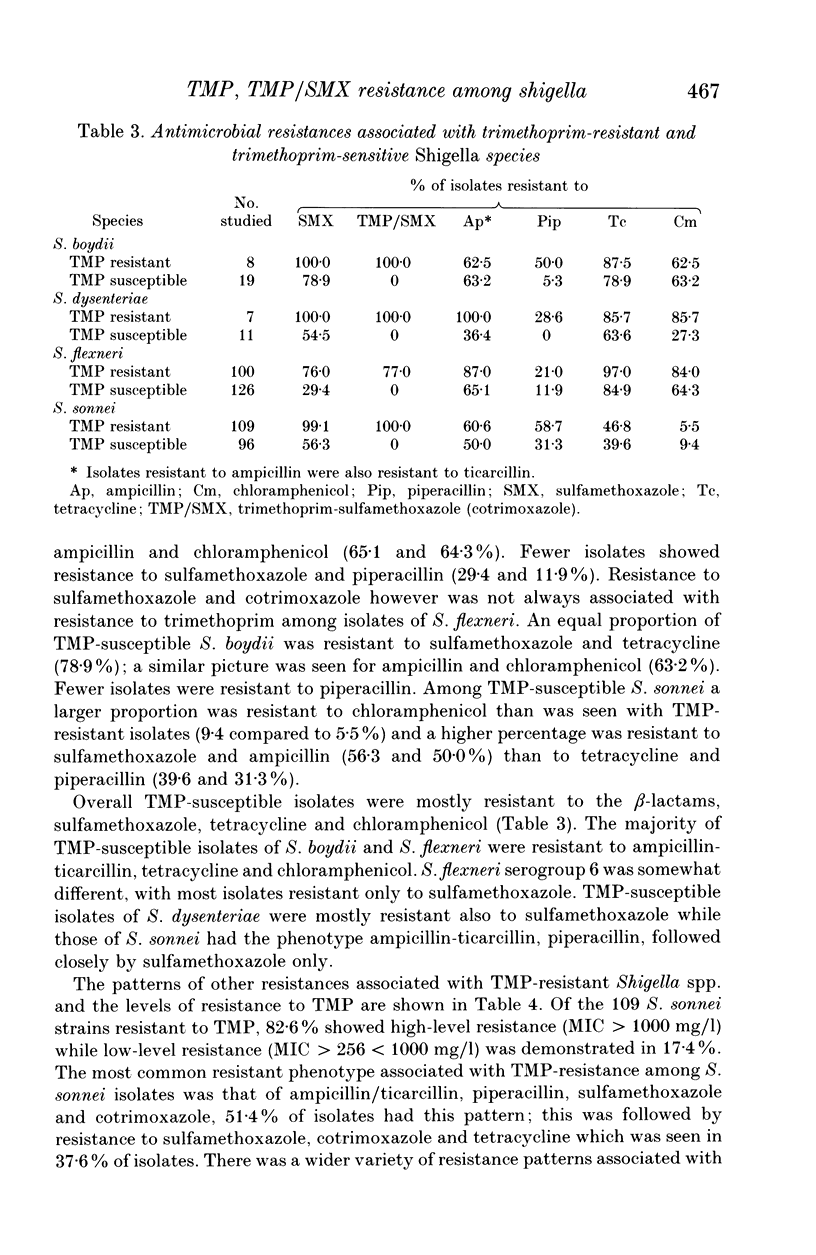
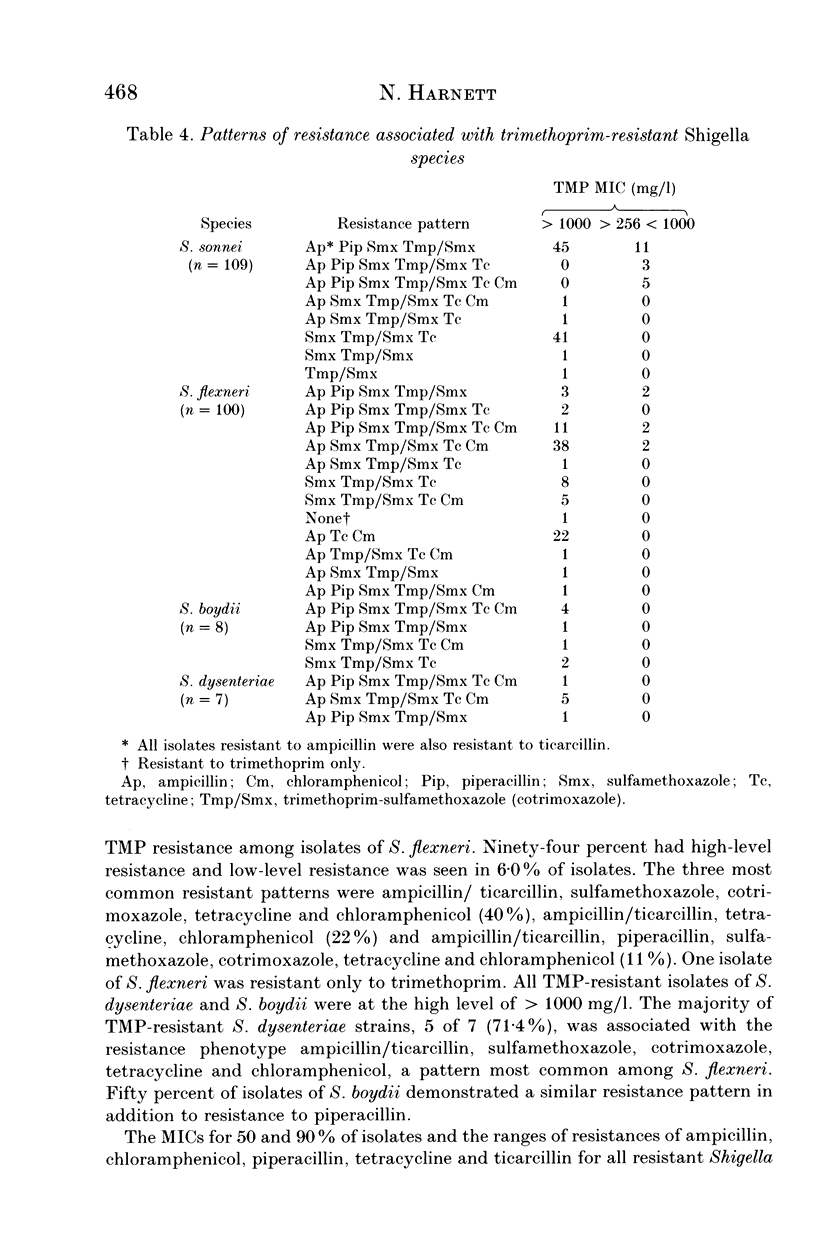
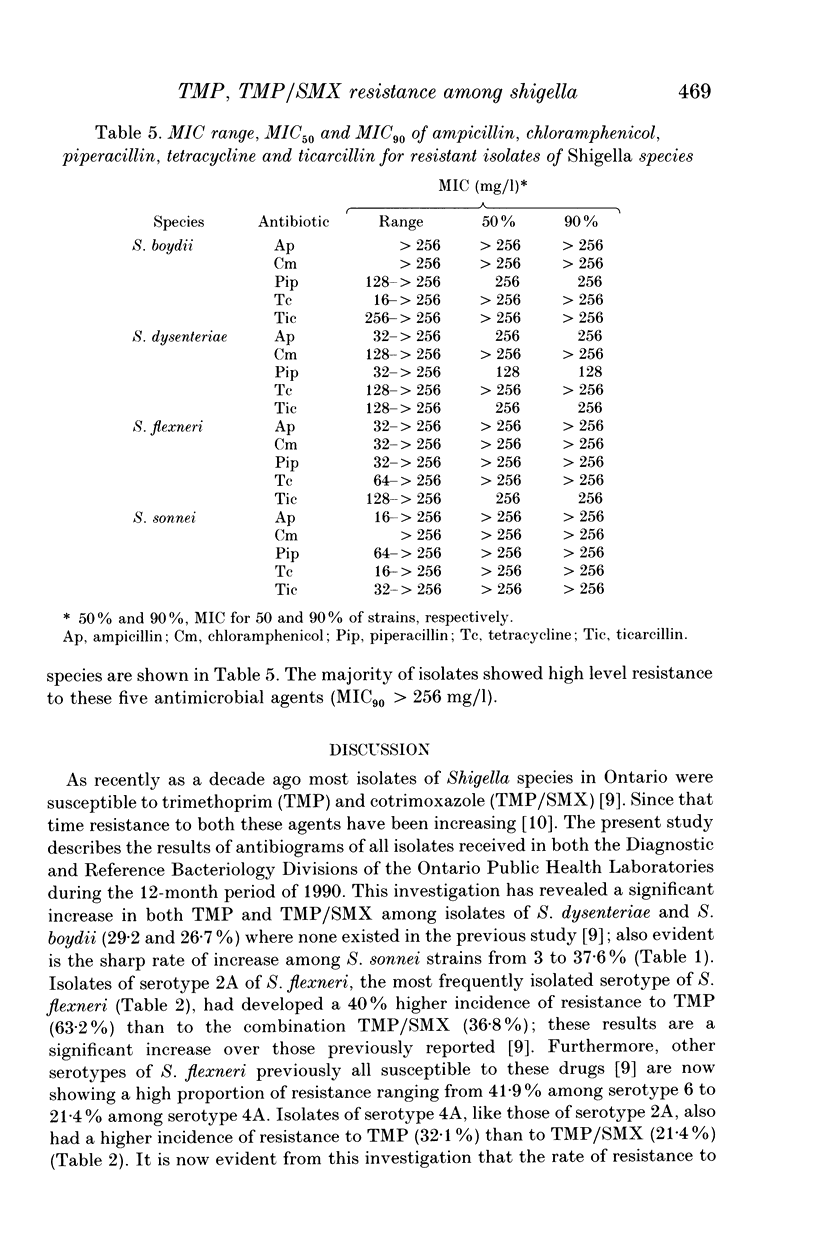
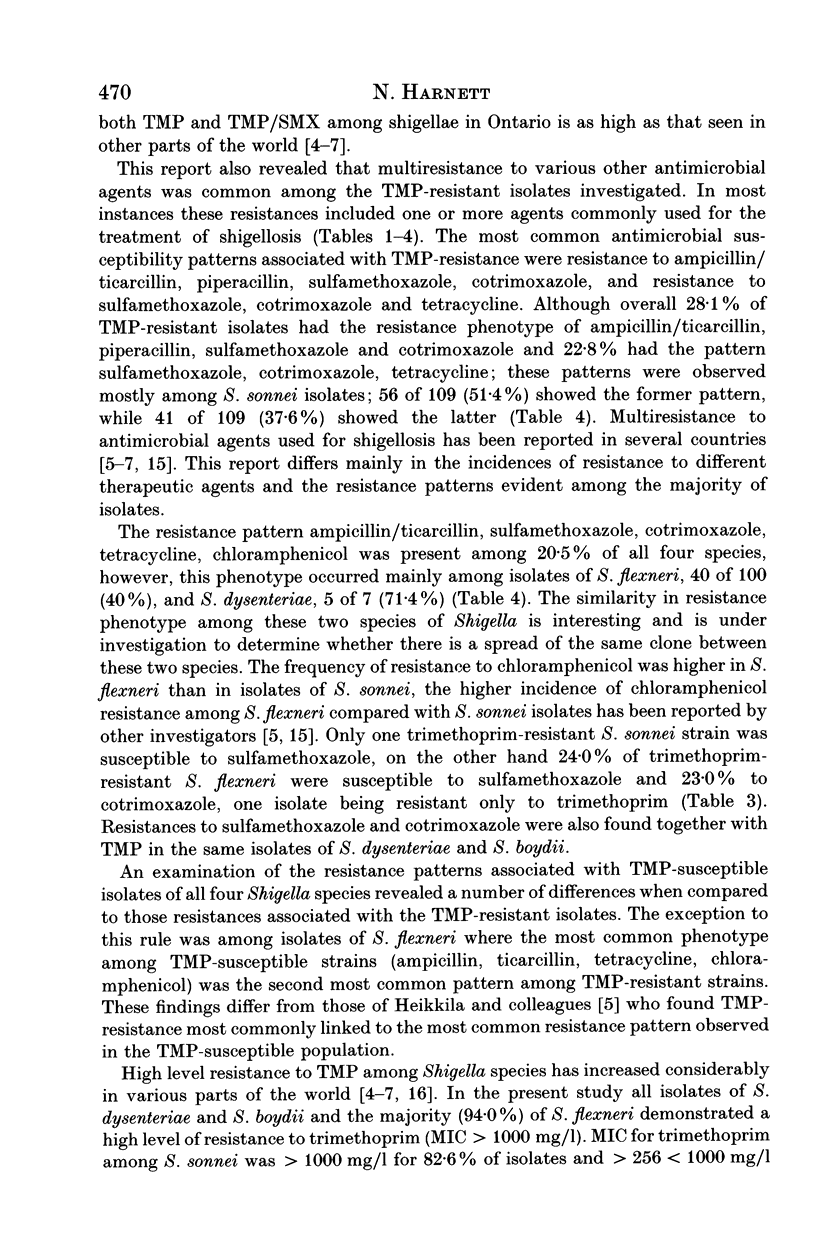
A total of 598 isolates of Shigella species (24 S. dysenteriae, 254 S. flexneri, 30 S. boydii, 290 S. sonnei) submitted to the Ontario Public Health Laboratories in 1990 were tested for their susceptibility to 14 antimicrobial agents by the agar dilution method. Overall 79.6% of isolates were resistant to one or more antimicrobial agents and 52.0% were resistant to four or more. Trimethoprim resistance ranged from 26.7% among isolates of S. boydii to 39.4% among S. flexneri strains. The majority of the 224 TMP resistant isolates (88.8%) demonstrated high level resistance (MIC > 1000 mg/l) to trimethoprim. Resistance to cotrimoxazole increased from 3% in 1978 to between 26.7 and 37.6% in 1990. MICs for 90% of isolates (MIC90s) for ampicillin, ticarcillin and piperacillin were 128 to > 256 mg/l, > 256 for tetracycline and chloramphenicol, and > 2.0/38.0 for cotrimoxazole. These results from the Canadian Province of Ontario emphasize the need for prudent use of antimicrobial agents in the treatment of shigellosis.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bannatyne R. M., Toma S., Cheung R., Hu G. Resistance to trimethoprim and other antibiotics in shigellae isolated in the province of Ontario. Can J Microbiol. 1980 Oct;26(10):1256–1258. doi: 10.1139/m80-209. [DOI] [PubMed] [Google Scholar]
- Bannatyne R. M., Toma S., Cheung R. Nalidixic acid analogues and Shigella. Lancet. 1984 Jul 21;2(8395):172–173. doi: 10.1016/s0140-6736(84)91094-8. [DOI] [PubMed] [Google Scholar]
- Bratoeva M. P., John J. F., Jr Dissemination of trimethoprim-resistant clones of Shigella sonnei in Bulgaria. J Infect Dis. 1989 Apr;159(4):648–653. doi: 10.1093/infdis/159.4.648. [DOI] [PubMed] [Google Scholar]
- DuPont H. L. Use of quinolones in the treatment of gastrointestinal infections. Eur J Clin Microbiol Infect Dis. 1991 Apr;10(4):325–329. doi: 10.1007/BF01967006. [DOI] [PubMed] [Google Scholar]
- Griffin P. M., Tauxe R. V., Redd S. C., Puhr N. D., Hargrett-Bean N., Blake P. A. Emergence of highly trimethoprim-sulfamethoxazole-resistant Shigella in a native American population: an epidemiologic study. Am J Epidemiol. 1989 May;129(5):1042–1051. doi: 10.1093/oxfordjournals.aje.a115208. [DOI] [PubMed] [Google Scholar]
- Harnett N., McLeod S., AuYong Y., Krishnan C. Increasing incidence of resistance among shigellae to trimethoprim. Lancet. 1991 Mar 9;337(8741):622–622. doi: 10.1016/0140-6736(91)91694-p. [DOI] [PubMed] [Google Scholar]
- Harnett N. Transferable high-level trimethoprim resistance among isolates of Escherichia coli from urinary tract infections in Ontario, Canada. Epidemiol Infect. 1992 Dec;109(3):473–481. doi: 10.1017/s0950268800050469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heikkilä E., Siitonen A., Jahkola M., Fling M., Sundström L., Huovinen P. Increase of trimethoprim resistance among Shigella species, 1975-1988: analysis of resistance mechanisms. J Infect Dis. 1990 Jun;161(6):1242–1248. doi: 10.1093/infdis/161.6.1242. [DOI] [PubMed] [Google Scholar]
- Ling J., Kam K. M., Lam A. W., French G. L. Susceptibilities of Hong Kong isolates of multiply resistant Shigella spp. to 25 antimicrobial agents, including ampicillin plus sulbactam and new 4-quinolones. Antimicrob Agents Chemother. 1988 Jan;32(1):20–23. doi: 10.1128/aac.32.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litwin C. M., Ryan K. J., Chipowsky S., Storm A., McCombie S. Molecular epidemiology of Shigella sonnei in Pima County, Arizona: evidence for a Mexico-related plasmid. J Infect Dis. 1990 Apr;161(4):797–800. doi: 10.1093/infdis/161.4.797. [DOI] [PubMed] [Google Scholar]
- Mata L. J., Gangarosa E. J., Cáceres A., Perera D. R., Mejicanos M. L. Epidemic Shiga bacillus dysentery in Central America. I. Etiologic investigations in Guatemala, 1969. J Infect Dis. 1970 Sep;122(3):170–180. doi: 10.1093/infdis/122.3.170. [DOI] [PubMed] [Google Scholar]
- McCormack J. G. Nalidixic acid for shigellosis. Lancet. 1983 Nov 5;2(8358):1091–1091. doi: 10.1016/s0140-6736(83)91081-4. [DOI] [PubMed] [Google Scholar]
- Munshi M. H., Sack D. A., Haider K., Ahmed Z. U., Rahaman M. M., Morshed M. G. Plasmid-mediated resistance to nalidixic acid in Shigella dysenteriae type 1. Lancet. 1987 Aug 22;2(8556):419–421. doi: 10.1016/s0140-6736(87)90957-3. [DOI] [PubMed] [Google Scholar]
- Olukoya D. K., Oni O. Plasmid profile analysis and antimicrobial susceptibility patterns of Shigella isolates from Nigeria. Epidemiol Infect. 1990 Aug;105(1):59–64. doi: 10.1017/s0950268800047646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panhotra B. R., Desai B., Sharma P. L. Nalidixic-acid-resistant Shigella dysenteriae I. Lancet. 1985 Mar 30;1(8431):763–763. doi: 10.1016/s0140-6736(85)91310-8. [DOI] [PubMed] [Google Scholar]
- Rogerie F., Ott D., Vandepitte J., Verbist L., Lemmens P., Habiyaremye I. Comparison of norfloxacin and nalidixic acid for treatment of dysentery caused by Shigella dysenteriae type 1 in adults. Antimicrob Agents Chemother. 1986 May;29(5):883–886. doi: 10.1128/aac.29.5.883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tauxe R. V., Puhr N. D., Wells J. G., Hargrett-Bean N., Blake P. A. Antimicrobial resistance of Shigella isolates in the USA: the importance of international travelers. J Infect Dis. 1990 Nov;162(5):1107–1111. doi: 10.1093/infdis/162.5.1107. [DOI] [PubMed] [Google Scholar]


