Abstract
Osteonecrosis of the femoral head is a disabling condition affecting young patients and treatment of the disease in these patients is variable. We retrospectively reviewed 39 patients (43 hips) in whom a modified transtrochanteric rotational osteotomy was performed for osteonecrosis. The minimum followup was 24 months (mean, 36.6 months; range, 24–52 months). The mean patient age was 34.3 years (range, 20–51 years). Based on the ARCO classification, 17 hips were classified as Stage II and 26 as Stage III. We performed rotational osteotomy alone in 15 cases, in combination with simple bone grafting in three, and in combination with muscle-pedicle-bone grafting in 25. Sixteen of 17 ARCO Stage II cases and 24 of 26 ARCO Stage III cases had no progression of collapse or lesion size; three hips progressively collapsed. Of the 40 hips without progression the Harris hip score improved from a mean 70 to 92 points at final followup, as did the range of motion of the hip. Modified transtrochanteric rotational osteotomy is an effective method for delaying the progression of collapse in the treatment of selected cases of osteonecrosis of the femoral head.
Level of Evidence: Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Osteonecrosis of the femoral head is a disabling disease involving the hips of young people [6]. Despite many efforts, the etiology of osteonecrosis still has not been identified and the pathogenesis is not fully understood. Therefore, treatment methods are various and are often chosen according to stage, location, and size of the necrotic area. Surgery usually involves head-preserving procedures or total hip arthroplasty (THA). In general, the head-preserving treatments are used in Ficat-Arlet stage I or II and THA is used in Ficat-Arlet stage III or IV [25]. However, when performing THA in young patients, high rates of failure have been reported despite continuous improvement in the design and technique [4, 6, 15, 23, 24]. The etiology is unknown but the disease is characterized by the death of bone. Although in some cases the disease is static or progresses very slowly [20], in others it typically progresses to collapse of the subchondral bone and articular cartilage of the joint, ultimately leading to secondary degenerative change causing pain and limitation of joint motion.
Various head preservation procedures have been reported, such as core decompression which reduces bone-marrow pressure [8, 21], proximal femoral osteotomy [9], nonvascularized or vascularized bone graft [3, 5], and trochanteric or transtrochanteric rotational osteotomy [20, 27]. Sugioka’s transtrochanteric rotational osteotomy [27] especially is known as an effective head preservation procedure in younger patients. Despite some reports of good results, not all have reported success with this procedure [7, 26, 29]. Most complications and failure of this procedure are related to its technically demanding nature and the poor fixation stability provided by the screws, causing delayed union and increased varus [7, 14, 22]. This led several authors to recommend fixation with side plates and blade plates rather than with screws as originally described by Sugioka [2, 14, 26].
We modified Sugioka’s osteotomy technique so the greater trochanter was not detached, presuming our modification of the transtrochanteric rotational osteotomy (TRO) produces less tissue trauma, and provides better hip function. This method of TRO allows muscle-pedicle-bone grafting to be performed at the same time. We believe subsequent total hip arthroplasty would be easier in the event of failure of this procedure.
We asked whether: (1) this modified technique of TRO could prevent further collapse of most hips with ARCO II and III osteonecrosis; (2) blood flow to the femoral head would be restored following this procedure; (3) patients would have improved functional abilities postoperatively; and (4) there would be no increase in complication rates.
Materials and Methods
We retrospectively reviewed 39 patients (43 hips) with osteonecrosis of the femoral head treated by a modified TRO, and in whom followup was possible for at least 2 years. Association Research Circulation Osseous (ARCO) stages [1] were used for classification of osteonecrosis (Table 1). The study population included 33 men and six women, and the average patient age was 34.3 years (range, 20–51 years). The causes of osteonecrosis were excessive alcohol consumption in 15, steroid use in 11, idiopathic in 12, and posttraumatic in five. The indications for this surgery were (1) ARCO Stage II and ARCO Stage III with less than 50% involvement, and (2) intact area of the posterior or anterior femoral head greater than a third of the total articular surface. We performed MTRO alone in 15 cases, a combination of MTRO and simple bone grafting in three, and a combination of MTRO and muscle-pedicle-bone grafting in 25. Anterior rotation was performed in 40 cases and posterior rotation in three cases. Bilateral surgery was performed in four patients. The minimum followup duration was 24 months (average, 36.6 months; range, 24–52 months). No patients were lost to followup.
Table 1.
Classification of ARCO [1] stage and treatment method
| Stage | Number of cases | MTRO | MTRO with simple bone graft | MTRO with MPBG | Cases with progression |
|---|---|---|---|---|---|
| 2-A-central | 4 | 3 | 1 | ||
| 2-B-central | 2 | 2 | |||
| 2-B-lateral | 4 | 2 | 2 | ||
| 2-C-central | 3 | 1 | 2 | ||
| 2-C-lateral | 4 | 4 | 1 | ||
| 3-A-lateral | 2 | 2 | |||
| 3-B-lateral | 5 | 2 | 1 | 2 | 1 |
| 3-C-central | 1 | 1 | |||
| 3-C-lateral | 18 | 2 | 1 | 15 | 1 |
MTRO = modified transtrochanteric rotational osteotomy; MPBG = muscle-pedicle-bone graft.
Preoperative assessment of the patients included anteroposterior and lateral radiographs of the affected hip, MRI, and bone scans. The extent of necrosis was determined by the method described by Kerboul et al. [13] and the exact location of the lesion was determined by MRI. This information was used to determine the rotation angle required for the modified transtrochanteric rotational osteotomy. Anterior rotated osteotomy was indicated if the lesion involved less than the posterior third of the entire femoral head on true lateral radiograph. Posterior rotated osteotomy was indicated if the lesion involved more than the posterior third of the entire femoral head but the anterior portion of the head was still intact.
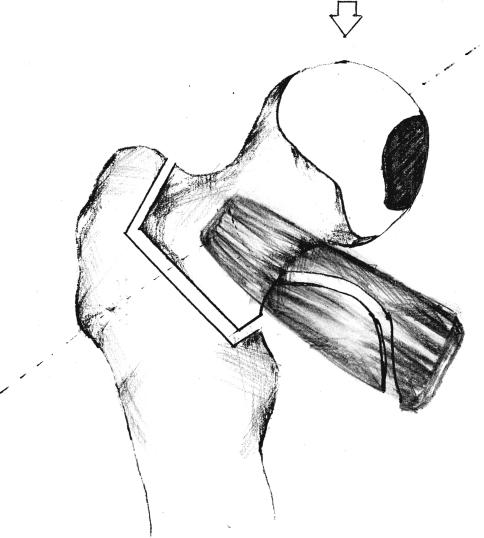
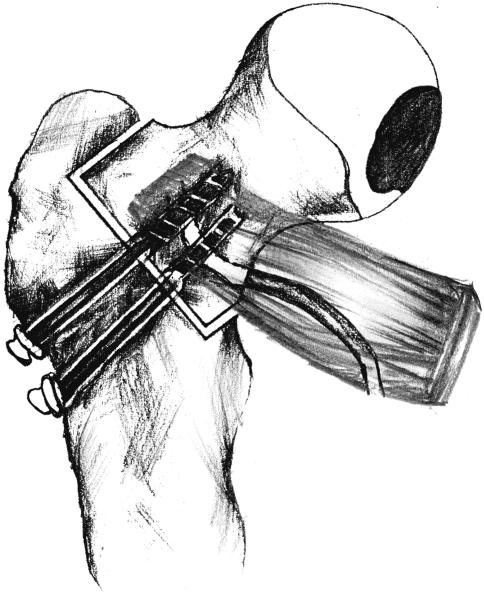
The surgery was performed by one surgeon (TRY). The patient was placed in a lateral decubitus position, and a lateral, straight, longitudinal skin incision of 12 to 17 cm was made, depending on the size and weight of the patient. The incision was centered over the greater trochanter and extended from 5 cm below the vastus lateralis ridge of the greater trochanter to 5 to 7 cm proximal to the greater trochanter. We used a posterior approach to the hip joint. The presence of the posterior branch of the medial circumflex artery was confirmed using Doppler (Minidop ES-100VX; Habeco, Tokyo, Japan), and protected from injury by not detaching the quadratus femoris. The short external rotator muscles, except the quadratus femoris, were completely transected. The joint capsule was circumferentially incised close to the acetabular rim. A 3.5-mm Steinman pin was driven centrally along the axis of the femoral neck from the lateral aspect of the greater trochanter. Using a k-wire bent to 90° as a guide, the transtrochanteric osteotomy site was determined perpendicular to the wire just proximal to the intertrochanteric line. In contrast to Sugioka’s technique [27], the greater trochanter was not detached (Fig. 1). With mobilization of the proximal fragment, any remnants of the capsule attachment to the proximal fragment was confirmed and detached. A Steinman pin was inserted into the proximal fragment and was used as a joystick to rotate the proximal fragment 70° to 90° in the anterior direction or 90° to 100° in the posterior direction. (Fig. 2). Two or three Steinman pins were inserted to fix the transtrochanteric osteotomy site temporarily. The position and rotation were confirmed by fluoroscopy. We used two or three 6.5-mm cancellous screws to fix the osteotomy site and then removed the temporary Steinman pins (Fig. 3). If we performed anterior rotation of the proximal fragment, one of the cancellous screws was inserted from the anteroinferior aspect of the trochanteric area to the posterosuperior area of the femoral neck to obtain fixation through the cortical bone, providing added stability and vice-versa in a case of posterior rotation of the proximal fragment. The remaining one or two cancellous screws were fixed from the lateral side of the greater trochanter to the femoral head. In the cases of ARCO Stage III ON, bone grafting was performed. In a small collapsed lesion, we performed simple bone grafting. However, if the lesion was relatively large, muscle-pedicle-bone grafting from the distal gluteus medius muscle and its attachment to the anterior greater trochanter was performed. We created a window in the neck-head junction for insertion of this muscle-pedicle-bone graft. Two cannulated cancellous screws were used for fixation in 29 cases, and three cannulated cancellous screws were used in 14 cases. The average operation time was 159.3 minutes (range, 125–220 minutes). Hemoglobin level changed from a preoperative mean of 12.4 gm/dL (range, 9.3–15.6 gm/dL) to 10.2 gm/dL (range, 7.6–13.2 gm/dL) postoperatively. Hematocrit levels dropped from 36.1% (range, 27.2%–45.1 %) to 26.6 % (range, 19.8%–32.3%).
Fig. 1.
The osteotomy sparing the greater trochanter is shown.
Fig. 2.
The femoral head was rotated anteriorly depending on the location of the necrotic area.
Fig. 3.
Fixation of the osteotomy with two cannulated screws is shown.
We reconfirmed the presence of the artery with Doppler (Minidop ES-100VX; Habeco, Tokyo, Japan) after confirmation of the fixation by fluoroscopy again and prior to repair of the deep fascia, subcutaneous layer, and skin.
Postoperatively, patients began nonweightbearing crutch walking within 1 week, depending on the general condition of the patient. Range-of-motion exercises were recommended during the postoperative period. The crutch walking with nonweightbearing was continued until the radiological bone union was confirmed, usually for 3 to 4 months. Radiological bone union was defined as absence of the radiolucent transtrochanteric osteotomy line. Postoperative scintigram was performed at 2 to 3 weeks and 3 months postoperatively.
We (TRY, SGC, JHL) performed a clinical evaluation using the Harris hip score (HHS) [11]. Other hip functions such as squatting and range of motion were also evaluated.
We (TRY, AAA, CIH) used regular anteroposterior and lateral radiographs to monitor femoral head collapse or degenerative changes. Radiographs were taken at 3 weeks, 6 months, and 1 year, then annually after the operation. Bone scan with pin-hole spectrometry was performed at 2 to 3 weeks and 3 months postoperatively.
If there was progression of osteonecrosis, if THAs were performed for any reason, or if collapse occurred in the followup period, the results were considered a “failure.” We considered the surgery successful if there was no further collapse or increase in apparent necrotic area within the minimum 24-month followup.
Results
Sixteen of 17 ARCO Stage II cases and 24 of 26 ARCO Stage III cases had no progression of collapse or lesion size. The location of the lesion in all three cases with collapse was lateral and the size of lesion in two was over 30%. All three cases with progression were treated by MTRO in combination with muscle-pedicle-bone graft or simple bone graft. One of the three cases underwent THA.
The early postoperative scintigrams revealed increased blood flow that gradually increased during the 3-month followup studies.
Excluding the three failed cases, the average preoperative Harris hip score was 70 points (range, 59–82 points), and it improved to 92 points (range, 77–100 points) at the last followup. The average range of motion of hips at last followup improved compared to that of preoperative values (Table 2). Thirty-nine cases (90.7%) could squat down and 40 cases (93%) could sit cross-legged.
Table 2.
Average range of motion of hip at last followup versus preoperative values
| Motion | Hip range of motion | |
|---|---|---|
| Preoperative | Postoperative | |
| Flexion | 90.9° | 98.7° |
| Internal rotation | 8° | 13.3° |
| External rotation | 36.1° | 48.4° |
| Abduction | 24.3° | 27° |
| Adduction | 13.1° | 14.8° |
Bone union occurred at the osteotomy site in all cases. The average union time was 14 weeks (range, 11–22 weeks). The complications included delayed union in one case, valgus angulation over 140° in two cases, and osteophyte formation in three cases. In the two cases with valgus angulation, the average postoperative neck-shaft angle was 146°, but no additional treatment was performed. We had no cases of infection or deep vein thrombosis. Three patients had subcapital osteophyte formation on radiograph, but no additional treatment was performed because these patients were free of pain.
Discussion
We asked whether our technique of modified transtrochanteric rotational osteotomy could prevent further collapse of most hips with ARCO II and III osteonecrosis, whether blood flow to the femoral head would be restored following this procedure, whether patients would have improved functional abilities postoperatively and whether these can be achieved without increased complication rates.
Our study is limited by the short-term followup. Longer followup would be necessary in this cohort of patients to determine the true survivability of this procedure. This study also lacked controls and the patients were not randomized to any other treatment methods.
Osteonecrosis of the femoral head is a devastating condition because of its propensity to affect young people and its often unrelenting progression despite treatment [30]. Treatments for osteonecrosis of the femoral head are varied and can be largely categorized into joint-preserving procedures and THA. Most patients are treated by THA. However, THA is not a definitive treatment because new problems such as liner wear, osteolysis, and loosening have developed, requiring later revision surgery. For these reasons we believe THA is not the best choice for young patients. Therefore, we prefer head-preserving procedures for those who are young and diagnosed early.
A report on 474 patients treated with the Sugioka osteotomy [27] revealed a success rate of 78%, with higher success rates seen in cases in earlier stages (stage II had an 89% success rate, stage III 73%, and stage IV 70%), and in cases involving smaller lesions. A comparison of several joint-preserving techniques was made by Saito et al. [22]. In their study, 54 hips were classified according to the classification of Inoue and Ono [12] and treated with core decompression (stage I, 17 cases), bone grafting (stage II, 18 cases), or osteotomy (stage III, 15 rotation, 4 varus). Overall, good or excellent results were seen in 67% of cases. For Stage II and III lesions, necrosis involving less than 50% of the femoral head resulted in a success rate of 91% compared to 27% success in cases involving larger lesions.
Sugioka [27] proposed a transtrochanteric rotational osteotomy (TRO) to preserve the femoral head in young patients when the posterior portion of the femoral head was not involved. By rotating the femoral head, the diseased weight-bearing surface is reestablished by repositioning the femoral head, reducing the forces on the diseased part to prevent collapse and allow healing [16, 28]. Sugioka [28] reported successful outcomes with rotation angles of 55°–70° in anterior rotated TRO and Atsumi and Kuroki [2] reported successful outcomes with rotation angles of up to 180° when performing a TRO with posterior rotation. As with THA, TRO is not permanent but it can delay THA for those young patients who have neither metabolic bone disease nor articular destruction.
We do not recommend TRO in Ficat Stage I hips in which core decompression seems more appropriate, or in Stage IV hips in which head-preserving surgery is no longer effective. For Stages II and III, although successful results have been reported on short-term followup, long-term followup results are variable and we believe unsatisfactory [10, 17]. We judged TRO had a high success rate for at least 24 months in Stage II, when success was defined by absence of progression of collapse or size of the osteonecrotic region (Table 1). Sugioka [28] reported 89% success in hips followed 2 to 11 years postoperatively and Masuda et al. [18] reported 82% success at average 5.1 years. In our series, “success” was defined as no evidence of further progression of osteonecrosis. The success rate for Stage II ON in our series was 94% (Fig. 4A–E). For Stage III, there is no consensus in the literature concerning results. Dean and Cabanela [7] had only 17% satisfactory results, but Saito et al. [23] had 45%, Sugano et al. [26] had 56%, and Sugioka [28] reported 73% satisfactory results. Atsumi and Kuroki [2] reported successful outcomes in 17 of 18 hips with FICAT III and IV treated with posterior rotated transtrochanteric osteotomy at a minimum of 24 months of followup (mean, 42 months; range, 24–94 months). However, our study revealed a 92% success rate in Stage III. The success rate in our study may be related to a more limited indication for the osteotomy and the use of supplementary bone and muscle pedicle-bone-grafting. Muscle pedicle-bone-grafts were indicated for ARCO Stage III hips where there was relatively large extent of necrosis and collapse of the femoral head. We believe the high success rate is partly attributable to this muscle pedicle-bone-grafting, which increased the vascularity of the femoral head. The location of the lesions in all three cases with progression was lateral and the size of the lesions in two cases was large; caution should be taken if a lesion is lateral and large as in all other preserving surgeries.
Fig. 4A–E.
(A) Radiographs from a 42-year-old man with osteonecrosis of the femoral head (Ficat-Arlet Stage II) are shown. (B) An axial MRI shows medial collapse. (C) A coronal MRI shows necrosis extending into the femoral neck. (D) An immediate radiograph after transtrochanteric rotational osteotomy with bone graft is shown. (E) Radiographs at 14 months postoperatively showed good union of the osteotomy site with good incorporation of grafted bone at the necrotic area.
Saito et al. [22] reported a high postoperative complication rate of 33% in the rotational osteotomy group of that series, consisting of femoral neck fracture in three patients with renecrosis of the femoral head in two and two late varus deformities. Sugioka [27] also reported complications related to his procedure, including lesser trochanteric fracture in one, femoral neck fracture in four, delayed union in five leading to increased varus deformities, and progression of osteonecrosis in two. Ohzono et al. [20] proposed a lack of skilled surgical technique or inappropriate patient selection or fixation causes a high failure rate. Our complications were not greatly different from those reported in the literature. There was one case of delayed union at 22.2 weeks, two cases had valgus angulation of the osteotomy, and three cases had osteophyte formation, all of which did not require any surgical intervention. Valgus position was one of our complications that developed during our early experience with the modified TRO technique, as part of the learning curve. As we gained more experience, we utilized intraoperative fluoroscopy and took extra care to avoid valgus positioning of the osteotomy. Varus positioning has the disadvantage of limb shortening so we did not perform intentional varus positioning to avoid limb length discrepancy. We believe the results of TRO depend on the indications for the surgery and the skill of the surgeons, both of which may vary.
In comparison with the original technique of TRO, a MTRO has several advantages. There is no need to detach and reattach the greater trochanter. Therefore, there is no concern about nonunion of the greater trochanter. The quadratus femoris is also not detached. By redirecting one of the screws for fixation of the osteotomy, we have had no cases of nonunion of the osteotomy site. Additional procedures such as muscle-pedicle-bone graft can be combined with MTRO. The postoperative rehabilitation as described by Sugioka [27] includes continuous skin traction for 1 week, followed by nightly skin traction for a further 2 weeks. Active hip exercises commenced within 2 weeks postoperatively. In our series, early rehabilitation is possible as skin traction is not required postoperatively and our patients begin hip mobilization exercises the day after surgery. Subsequent THA may be easier because the anatomy of the greater trochanter is not altered and the quadratus femoris, which may be important to preserve the circulation, is not detached. When the posterior branch of the medial circumflex artery is injured during surgery, the circulation through the quadratus femoris may be maintained. One study suggested quadratus femoris muscle-pedicle-bone grafting for treating displaced femoral neck fractures since the microcirculation in the muscle would theoretically provide additional blood flow through the quadratus femoris muscle [19].
Most of our patients had rotational osteotomy without a greater trochanteric osteotomy. With this method, we were able to perform anterior and posterior transtrochanteric rotation. Bone grafting was a supplementary procedure and was performed with a small window through the head-neck junction. We believe by adding this small procedure, the success rate could be improved. With the combination of rotational osteotomy and muscle pedicle bone grafting the indication for this MTRO could be further extended.
This procedure prevented progression (no collapse or increase regions of ON) in 93% by the minimum 24-month followup. In the short term the MTRO seems effective in Stages II and III with less than 50% involvement in either anterior or posterior portions of the femoral head. We therefore believe this technique is promising in young patients with Stage II or III osteonecrosis of the femoral head.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
References
- 1.ARCO (Association Research Circulation Osseous). Committee on Terminology and Classification. ARCO News. 1992;4:41–46.
- 2.Atsumi T, Kuroki Y. Modified Sugioka’s osteotomy: More than 130° posterior rotation for osteonecrosis of the femoral head with large lesion. Clin Orthop Relat Res. 1997;334:98–107. [DOI] [PubMed]
- 3.Bonfiglio M, Bardenstein MB. Treatment by bone-grafting of aseptic necrosis of the femoral head and non-union of the femoral neck (Phemister technique). J Bone Joint Surg Am. 1958;40:1329–1346. [PubMed]
- 4.Brinker MR, Rosenberg AG, Kull L, Galante JO. Primary total hip arthroplasty using noncemented porous coated femoral components in patients with osteonecrosis of the femoral head. J Arthroplasty. 1994;9:457–468. [DOI] [PubMed]
- 5.Buckley PD, Gearen PF, Petty RW. Structural bone-grafting for early atraumatic avascular necrosis of the femoral head. J Bone Joint Surg Am. 1991;73:1357–1364. [PubMed]
- 6.Coventry MB, Beckenbaugh RD, Nolan DR, Ilstrup DM. 2,012 total hip arthroplasties: A study of postoperative course and early complications. J Bone Joint Surg Am. 1974;56:273–284. [PubMed]
- 7.Dean MT, Cabanela ME. Transtrochanteric anterior rotational osteotomy for avascular necrosis of the femoral head. Long-term results. J Bone Joint Surg Br. 1993;75:597–601. [DOI] [PubMed]
- 8.Fairbank AC, Bhatia D, Jinnah RH, Hungerford DS. Long-term results of core decompression for ischemic necrosis of the femoral head. J Bone Joint Surg Br. 1995;77:42–49. [PubMed]
- 9.Fuchs B, Knothe U, Hertel R, Ganz R. Femoral osteotomy and iliac graft vascularization for femoral head osteonecrosis. Clin Orthop Relat Res. 2003;412:84–93. [DOI] [PubMed]
- 10.Ganz R, Buchler U. Overview of attempts to revitalize the dead head in aseptic necrosis of the femoral head–osteotomy and revascularization. In: Hungerford DS, ed. Hip. St Louis, MO: Mosby;1983:96–305. [PubMed]
- 11.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed]
- 12.Inoue A, Ono K. A histological study of idiopathic avascular necrosis of the head of the femur. J Bone Joint Surg Br. 1979;61-B:138–143. [DOI] [PubMed]
- 13.Kerboul M, Thomine J, Postel M, D’Aubigne RM. The conservative surgical treatment of idiopathic aseptic necrosis of the femoral head. J Bone Joint Surg Br. 1974;56:291–296. [PubMed]
- 14.Kinnard P, Lirette R. The Borden and Gearen modification of the Sugioka transtrochanteric rotational osteotomy in avascular necrosis: A preliminary report. Clin Orthop Relat Res. 1990;255:194–197. [PubMed]
- 15.Krackow KA, Mont MA, Maar DC. Limited femoral endoprosthesis for avascular necrosis of the femoral head. Orthop Rev. 1993;22:457–463. [PubMed]
- 16.Lafforgue P, Dahan E, Chagnaud C, Schiano A, Kasbarian M, Acquaviva PC. Early-stage avascular necrosis of the femoral head: MR imaging for prognosis in 31 cases with at least 2 years of follow-up. Radiology. 1993;187:199–204. [DOI] [PubMed]
- 17.Maistrelli G, Fusco U, Avai A, Bombelli R. Osteonecrosis of the hip treated by intertrochanteric osteotomy. A four- to 15-year follow-up. J Bone Joint Surg Br. 1988;70:761–766. [DOI] [PubMed]
- 18.Masuda T, Matsuno T, Hasegawa I, Kanno T, Ichioka Y, Kaneda K. Results of transtrochanteric rotational osteotomy for nontraumatic osteonecrosis of the femoral head. Clin Orthop Relat Res. 1988;228:69–74. [PubMed]
- 19.Morewessel R, Evarts CM. The use of quadratus femoris muscle pedicle bone graft for the treatment of displaced femoral neck fractures. Orthopedics. 1985;8:972–976. [DOI] [PubMed]
- 20.Ohzono K, Saito M, Takaoka K, Ono K, Saito S, Nishina T, Kadowaki T. Natural history of nontraumatic avascular necrosis of the femoral head. J Bone Joint Surg Br. 1991;73:68–72. [DOI] [PubMed]
- 21.Rosenwasser MP, Garino JP, Kiernan HA, Michelsen CB. Long term followup of thorough debridement and cancellous bone grafting of the femoral head for avascular necrosis. Clin Orthop Relat Res. 1994;306:17–27. [PubMed]
- 22.Saito S, Ohzono K, Ono K. Joint-preserving operations for idiopathic avascular necrosis of the femoral head: Results of core decompression, grafting and osteotomy. J Bone Joint Surg Br. 1988;70:78–84. [DOI] [PubMed]
- 23.Saito S, Saito M, Nishina T, Ohzono K, Ono K. Long-term results of total hip arthroplasty for osteonecrosis of the femoral head. A comparison with osteoarthritis. Clin Orthop Relat Res. 1989;244:198–207. [PubMed]
- 24.Stauffer RN. Ten-year follow-up study of total hip replacement. J Bone Joint Surg Am. 1982;64:983–990. [PubMed]
- 25.Steinberg ME. Management of avascular necrosis of the femoral head–an overview. Instr Course Lect. 1988;37:41–50. [PubMed]
- 26.Sugano N, Takaoka K, Ohzono K, Matsui M, Saito M, Saito S. Rotational osteotomy for non-traumatic avascular necrosis of the femoral head. J Bone Joint Surg Br. 1992;74:734–739. [DOI] [PubMed]
- 27.Sugioka Y. Transtrochanteric anterior rotational osteotomy of the femoral head in the treatment of osteonecrosis affecting the hip: a new osteotomy operation. Clin Orthop Relat Res. 1978;130:191–201. [PubMed]
- 28.Sugioka Y. Transtrochanteric rotational osteotomy in the treatment of idiopathic and steroid induced femoral head necrosis, Perthes’ disease, slipped capital femoral epiphysis, and osteoarthritis of the hip. Indications and results. Clin Orthop Relat Res. 1984;184:12–23. [PubMed]
- 29.Tooke SMT, Amstutz HC, Hedley AK. Results of transtrochanteric rotational osteotomy for femoral head osteonecrosis. Clin Orthop Relat Res. 1987;224:150–157. [PubMed]
- 30.Vail TP, Covington DB. The incidence of osteonecrosis. In Urbaniak JR, Jones JP, eds. Osteonecrosis : Etiology, Diagnosis, and Treatment. Chicago, Ill: American Academy of Orthopaedic Surgeons; 1997:43–49.