Abstract
Human coronary anatomy allows for a wide range of anatomic variants while maintaining certain consistent features. The use of specific descriptions and names is helpful in talking about variants that have an implicit potential for clinical consequences. In reviewing the angiograms of 813 patients, we newly identified a coronary pattern that we propose to name “acute takeoff of the circumflex artery” in 16 patients (2%). This previously unreported pattern angiographically features a ≤45° angle between the mainstem of the left main stem and the circumflex coronary artery in 2 orthogonal, caudal projections. The acute angle is associated with a substantially longer left main trunk than that seen in the general population (24.9 vs 9.8 mm, respectively). This anomaly increases the technical difficulty and failure rate of percutaneous coronary intervention unless the operator makes specific adaptations, some of which we describe herein.
Key words: Circumflex coronary artery, coronary angiography, coronary vessel anomalies, left main trunk, percutaneous coronary intervention/methods
Human coronary artery anatomy is highly variable among individuals.1 It is only because of a special clinical interest that, from time to time, cardiovascular experts are led to identify unusual morphologic forms, describe them and their associated features, and label them with specific names. We present a newly identified coronary pattern that we propose to call “acute takeoff of the circumflex artery” (ATO-Cx). This pattern, which features an unusual configuration of the proximal circumflex artery, can hinder percutaneous coronary interventions (PCIs) in this territory. Having investigated the incidence of ATO-Cx in a general catheterization-laboratory population, we describe its angiographic features, discuss the technical challenges that it poses during PCI, and suggest some procedural adaptations for overcoming these difficulties.
Methods
We prospectively reviewed 1,044 consecutive selective digital coronary angiographic examinations that we performed in the catheterization laboratories of St. Luke's Episcopal Hospital in 2005 and 2006. Angiograms were excluded if the left coronary artery and its proximal branches were inadequately visualized in the right anterior oblique (RAO)/caudal and left anterior oblique (LAO)/caudal projections, if the left main trunk or proximal circumflex artery was totally occluded, or if the circumflex territory was diminutive (luminal size, <2.0 mm).
In the remaining cases, we visually determined whether the angle α between the left main artery and the circumflex proximal trunk was ≤45° (the ATO-Cx group) or >45° (the control group) (Fig. 1). In targeted cases, we measured the angle between the left main trunk and the proximal circumflex artery in the LAO/caudal and RAO/caudal projections (see Fig. 1) with Encompass® online quantitative angiography software (Heartlab, Inc., Agfa HealthCare; Westerly, RI). Using the same software, we measured the length of the proximal left main trunk in all ATO-Cx patients and in 50 consecutive “normal” patients. The incidence of coronary atherosclerotic disease that required PCI in the circumflex branch was recorded. Five additional PCI procedures that involved the ATO-Cx in patients outside our study group were reviewed to identify technical difficulties and their procedural solutions.
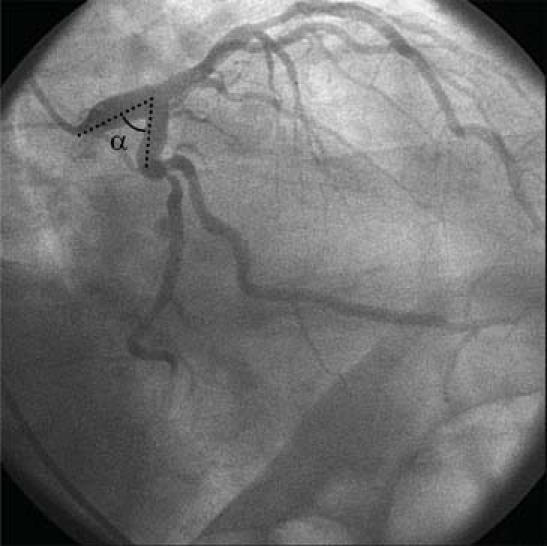
Fig. 1 Method of measuring the angle in the left anterior oblique/caudal projection. Minor systolo-diastolic variations in the angle should be averaged.
All statistical analyses were performed with Statistical Analysis Software version 9.1 (SAS Institute Inc.; Cary NC). Intergroup differences were evaluated via the Student t test. A P value of <0.05 was considered significant.
Results
Of the 1,044 consecutive patients whose angiograms were reviewed, 813 qualified for inclusion in the study. This group included 560 men and 253 women, whose ages ranged from 19 to 90 years (mean, 65.2 yr). Sixteen (2%) of these patients had a ≤45° α angle between the left main artery and the circumflex trunk (Figs. 2 and 3), and the remaining 797 patients (the control group) had a >45° (normal) angle.
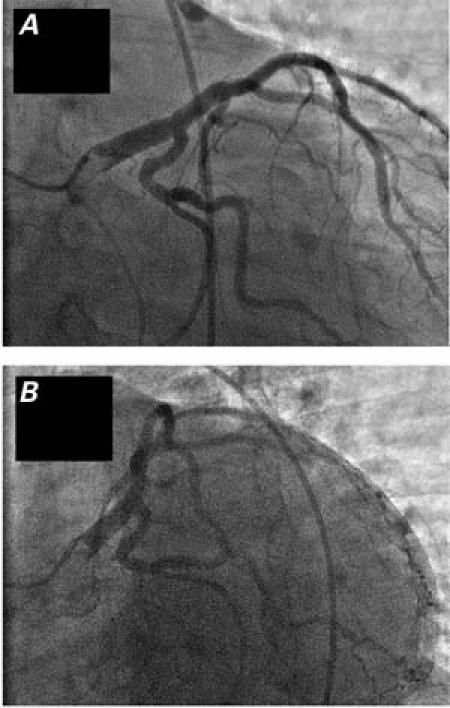
Fig. 2 Angiograms obtained in the left anterior oblique/caudal (A) and right anterior oblique/caudal (B) projections in the same patient, who has acute takeoff of the circumflex artery.
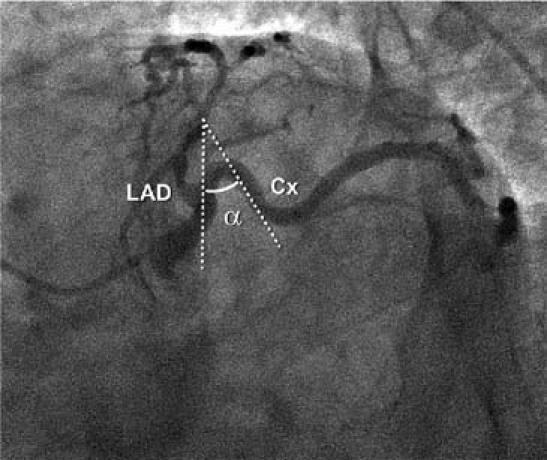
Fig. 3 S-shaped variant of acute takeoff of the circumflex artery, in which the initial wide left main/circumflex angle hinders calculation of the α angle. This variant is less common than the abrupt takeoff and enables easier percutaneous intervention for circumflex lesions. Cx = circumflex artery; LAD = left anterior descending artery
The 11 men and 5 women with ATO-Cx ranged in age from 50 to 87 years (mean, 66.6 yr). Three patients had severe coronary obstructive disease of the circumflex artery, and 1 of them underwent coronary stent angioplasty. In the 16 patients, the mean α angle was 36° in the RAO/caudal projection and 39° in the LAO/caudal (range, 20°-45°) (Table I). Occasionally, in the RAO/caudal view, the circumflex artery presented an acute angle, then reoriented itself anteriorly, in an S-shaped configuration (Fig. 3), rather than having a more typical straight course after the acute takeoff angle (Figs. 1 and 2). Interestingly, the length of the left main trunk averaged 24.9 mm in the ATO-Cx group but only 9.8 mm in the control group (P <0.0001). Figure 4 shows the typical appearance of the ATO-Cx on computerized axial tomography.
TABLE I. Characteristics of Acute Takeoff of the Circumflex Artery (ATO-Cx) versus Normal Circumflex Anatomy
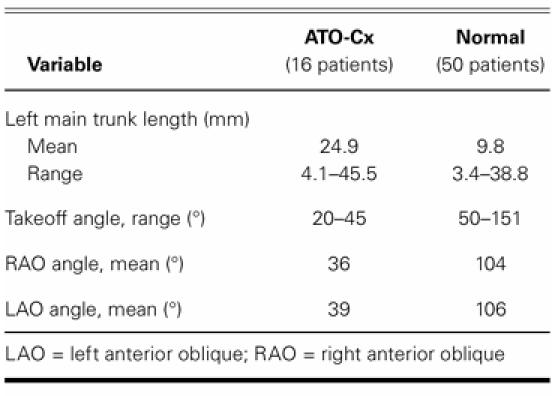
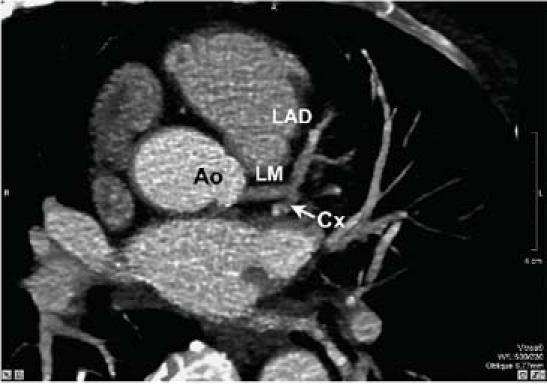
Fig. 4 Computerized axial tomogram of acute takeoff of the circumflex artery (arrow), as shown angiographically in Figure 2.
Ao = aorta; Cx = circumflex artery; LAD = left anterior descending artery; LM = left main trunk
In a series of 5 patients with ATO-Cx who required stent angioplasty, we recognized several procedural dif ficulties (Fig. 5). The ATO-Cx was generally difficult to enter even with a coronary guidewire. Balloons and especially stents had unusual difficulty tracking the guidewire over such an acute angle. These problems adversely affected both the procedural time and the success rate. Because of the small size of this series, however, we were unable to quantify these observations.
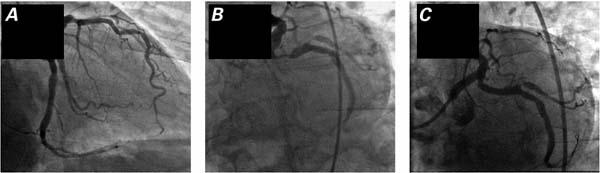
Fig. 5 Preoperative (A, B) and postoperative (C) angiograms of acute takeoff of the circumflex artery involving a severe circumflex atherosclerotic lesion. By using a double guidewire, we were able to straighten the severe proximal angulation and successfully deploy a stent at the target lesion.
Discussion
In our general catheterization-laboratory population of 813 patients, 16 were found to have ATO-Cx, defined as a ≤45° mean angle in the LAO/caudal and/or RAO/caudal projections, for an incidence of 2%. Measurement of the α angle was occasionally hindered by the variability in the amplitude of the circumflex takeoff curve (Figs. 1–5), which could be either abrupt (Figs. 1, 2, 4, and 5), as in typical cases, or wide (Fig. 3). We concluded that an acute, narrow-angled takeoff should be considered the pure form of ATO-Cx, while longer (double or S-shaped) curves of the proximal circumflex artery should probably be considered a less frequent form (Fig. 3), with different technical implications (more benign).
In general, ATO-Cx may be identified by using a single angiographic projection, because the angle is similar in either the LAO or the RAO view; the projection should always be caudally tilted. In the straight RAO or LAO projection, the incidence of ATO-Cx would be spuriously high because of the implied foreshortening effect.
The length of the left main trunk is potentially relevant, because one reason for ATO-Cx could be origination of the circumflex artery at an unusually distal point of an anteriorly tilted left main trunk: the circumflex artery must then assume a backward proximal course in order to join the normally located distal circumflex artery (Fig. 6). In our subgroup of 50 “normal” patients, the left main trunk was significantly shorter than it was in the ATO-Cx group (9.8 vs 24.9 mm; P <0.0001), which appears to indicate a consistent but not constant association between the occurrence of ATO-Cx and the location of the circumflex ostium off the left main trunk. If confirmed in larger studies, this finding would imply that ATO-Cx could be considered merely a synonym for “anomalous origin of the circumflex artery from the left anterior descending artery” (an alternative nomenclature already in use). Alternatively, ATO-Cx could result from posterior origination of the left main artery off the left sinus of Valsalva, with an unusually anterior tilt of the left main trunk.2 Computerized axial tomographic angiography could be useful in this regard, as shown in Figure 4. Figure 6 shows the likely spectrum of 3 possible forms of ATO-Cx: “a primary, abrupt posterior circumflex tilt”; “an anterior tilt of the left main”2; or “a redundant proximal circumflex artery” with an S-shaped course.
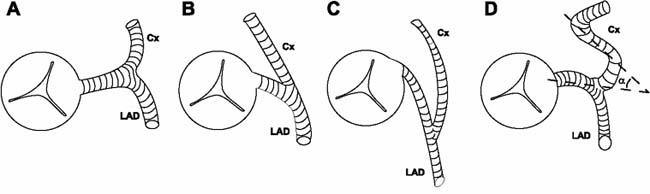
Fig. 6 Schematic representation of normal circumflex anatomy (A) versus 3 different configurations in acute takeoff of the circumflex artery: a typical, normal takeoff (B); posterior origination with acute angulation (C); and a sinuous, S-shaped takeoff, with the method for calculating the α angle superimposed (D). Cx = circumflex artery; LAD = left anterior descending artery
Because ATO-Cx is unrecognized by most cardiologists, it consistently leads to frustration and an increased rate of technical failure during PCI. In such cases, the operator generally encounters unusual difficulties in passing a guidewire into the distal circumflex artery, and even more in tracking a coronary stent over the wire and deploying that stent. These difficulties increase the procedural time, fluoroscopy time, quantity of hardware used, and rate of procedural failure. In an attempt at remedy, we propose that operators adapt standard PCI techniques:
Improve the support afforded by the guiding catheter by increasing the French size and/or choosing the XB or left Amplatz curves;
Initially select a highly steerable, soft-tip coronary guidewire that should feature a gradual transition from a relatively flexible tip to a relatively stiff body—as seen with the Wizard® (Cordis Endovascular, a Johnson & Johnson company; Miami Lakes, Fla), the Hi-Torque Pilot™ 150 (Abbott Vascular; Redwood City, Calif; a division of Abbott Laboratories, Inc.; Abbott Park, III), or the PT Graphix™ (Boston Scientific/SCIMED; Maple Grove, Minn);
Once past the acute angle, exchange (inside the balloon catheter) the initial soft, very steerable guide-wire for an extra-stiff one, 0.014 inches in diameter, such as the Hi-Torque Spartacore® or the Hi-Torque Ironman™ (Abbott Vascular);
Occasionally add a secondary (“buddy”) wire3 to better rectify the anomalous angle and enable passage of the initial balloon catheter and the stent, while stabilizing the support; and
Reduce the length of the stent (by using, if necessary, 2 shorter, overlapping stents).
The probability of successfully rectifying the ATO-Cx angle depends on the original acuteness of the angle, the age of the patient, and the degree of atherosclerotic changes in the vessel.
Conclusions
We propose that the foregoing newly described coronary variant be termed ATO-Cx. Our group1 previously suggested that an anatomic pattern with an incidence of ≥1% in an unselected population should be considered a normal variant, as distinguished from a coronary anomaly (incidence, <1%). The present retrospective study indicates that, because of the technical difficulties presented by ATO-Cx during PCI in the circumflex territory, this is a relevant coronary variant that should be designated by a specific term. To enhance success when performing PCI under these conditions, we recommend the adapted techniques outlined above.
Footnotes
Address for reprints: Paolo Angelini, MD, P.O. Box 20206, Houston, TX 77030 E-mail: PAngelini@leachmancardiology.com
References
- 1.Angelini P, Villason S, Chan AV Jr, Diez JG. Normal and anomalous coronary arteries in humans. In: Angelini P, editor. Coronary artery anomalies: a comprehensive approach. Philadelphia: Lippincott Williams & Wilkins; 1999. p. 27–150.
- 2.Angelini P. Balloon catheter coronary angioplasty. In: Angelini P, Cooley DA, editors. Mount Kisco: Futura Publishing Company, Inc.; 1987. p. 75.
- 3.Selig MB. Lesion protection during fixed-wire balloon angioplasty: use of the “buddy wire” technique and access catheters. Cathet Cardiovasc Diagn 1992;25(4):331–5. [DOI] [PubMed]


