Abstract
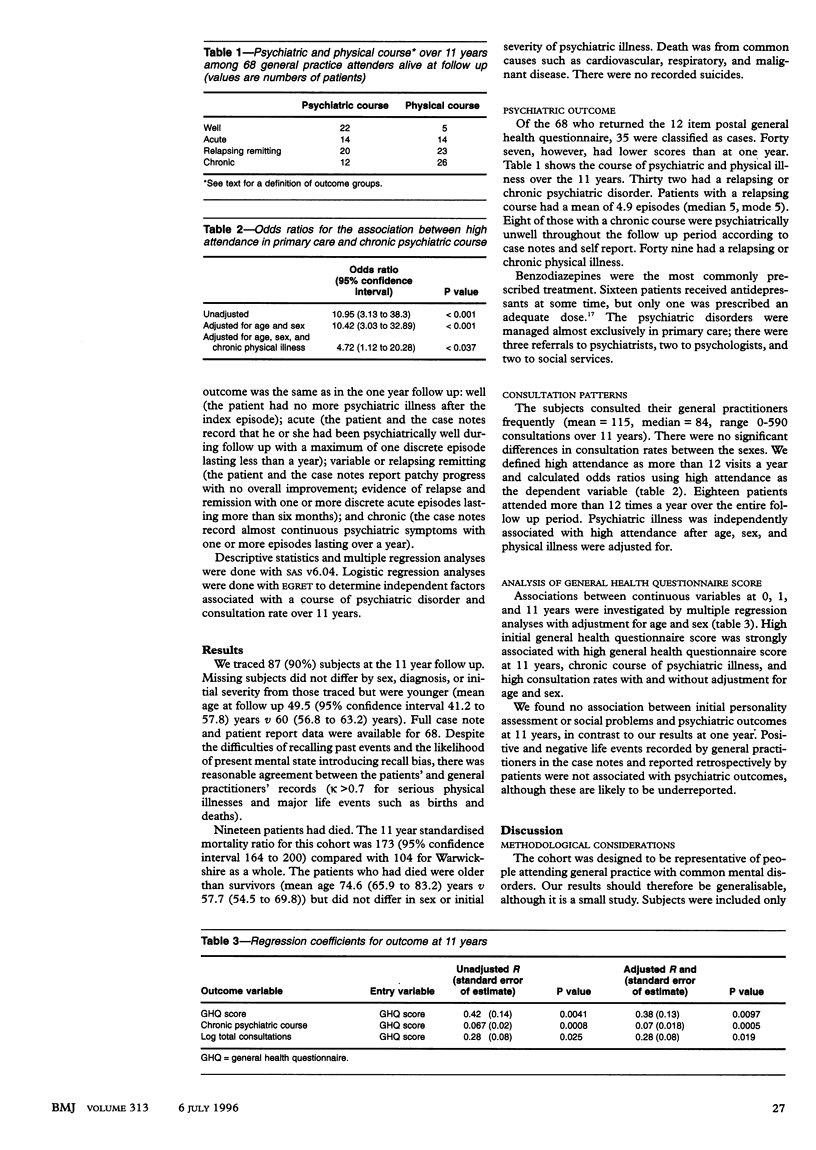
OBJECTIVE--To determine the 11 year outcome of neurotic disorder in general practice. DESIGN--Cohort study over 11 years. SETTING--Two general practices in Warwickshire England. SUBJECTS--100 patients selected to be representative of those identified nationally by general practitioners as having neurotic disorders. MAIN OUTCOME MEASURES--Mortality, morbidity, and use of health services. RESULTS--At 11 years 87 subjects were traced. The 11 year standardised mortality ratio was 173 (95% confidence interval 164 to 200). 47 were cases on the general health questionnaire, 32 had a relapsing or chronic psychiatric course, and 49 a relapsing or chronic physical course. Treatment for psychiatric illness was mainly drugs. The mean number of consultations per year was 10.8 (median 8.7). A persistent psychiatric diagnosis at one year follow up was associated with high attendance ( > 12 visits a year for 11 years) at follow up after age, sex, and physical illness were adjusted for. Severity of psychiatric illness (general health questionnaire score) at outset predicted general health questionnaire score at 11 year follow up, course of psychiatric illness, and high consultation rate. CONCLUSION--These data support the view that a neurotic illness can become chronic and is associated with raised mortality from all causes and high use of services. Such patients need effective intervention, particularly those with a more severe illness who do not recover within one year.
Full text
PDF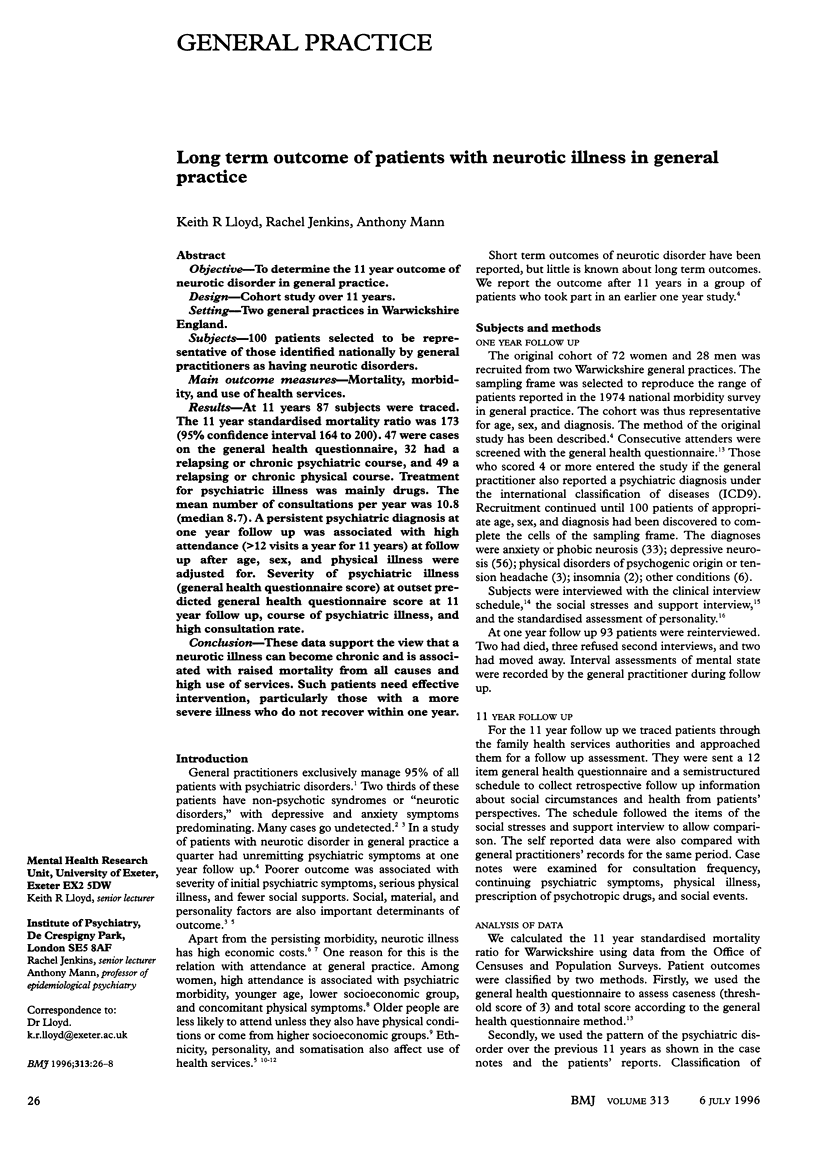
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Corney R., Murray J. The characteristics of high and low attenders at two general practices. Soc Psychiatry Psychiatr Epidemiol. 1988 Jan;23(1):39–48. doi: 10.1007/BF01788441. [DOI] [PubMed] [Google Scholar]
- Dowrick C., Buchan I. Twelve month outcome of depression in general practice: does detection or disclosure make a difference? BMJ. 1995 Nov 11;311(7015):1274–1276. doi: 10.1136/bmj.311.7015.1274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg L. Treating depression and anxiety in primary care. Closing the gap between knowledge and practice. N Engl J Med. 1992 Apr 16;326(16):1080–1084. doi: 10.1056/NEJM199204163261610. [DOI] [PubMed] [Google Scholar]
- Escobar J. I., Burnam M. A., Karno M., Forsythe A., Golding J. M. Somatization in the community. Arch Gen Psychiatry. 1987 Aug;44(8):713–718. doi: 10.1001/archpsyc.1987.01800200039006. [DOI] [PubMed] [Google Scholar]
- Goldberg D. P., Cooper B., Eastwood M. R., Kedward H. B., Shepherd M. A standardized psychiatric interview for use in community surveys. Br J Prev Soc Med. 1970 Feb;24(1):18–23. doi: 10.1136/jech.24.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenkins R., Mann A. H., Belsey E. The background, design and use of a short interview to assess social stress and support in research and clinical settings. Soc Sci Med E. 1981 Aug;15(3):195–203. doi: 10.1016/0271-5384(81)90013-2. [DOI] [PubMed] [Google Scholar]
- Lloyd K. Depression and anxiety among Afro-Caribbean general practice attenders in Britain. Int J Soc Psychiatry. 1993 Spring;39(1):1–9. doi: 10.1177/002076409303900101. [DOI] [PubMed] [Google Scholar]
- Lloyd K., Jenkins R. The economics of depression in primary care. Department of Health initiatives. Br J Psychiatry Suppl. 1995 Apr;(27):60–62. [PubMed] [Google Scholar]
- Mann A. H., Jenkins R., Belsey E. The twelve-month outcome of patients with neurotic illness in general practice. Psychol Med. 1981 Aug;11(3):535–550. doi: 10.1017/s0033291700052855. [DOI] [PubMed] [Google Scholar]
- Paykel E. S., Priest R. G. Recognition and management of depression in general practice: consensus statement. BMJ. 1992 Nov 14;305(6863):1198–1202. doi: 10.1136/bmj.305.6863.1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sims A. Mortality in neurosis. Lancet. 1973 Nov 10;2(7837):1072–1076. doi: 10.1016/s0140-6736(73)92673-1. [DOI] [PubMed] [Google Scholar]
- Sims A., Prior P. The pattern of mortality in severe neuroses. Br J Psychiatry. 1978 Oct;133:299–305. doi: 10.1192/bjp.133.4.299. [DOI] [PubMed] [Google Scholar]


