Abstract
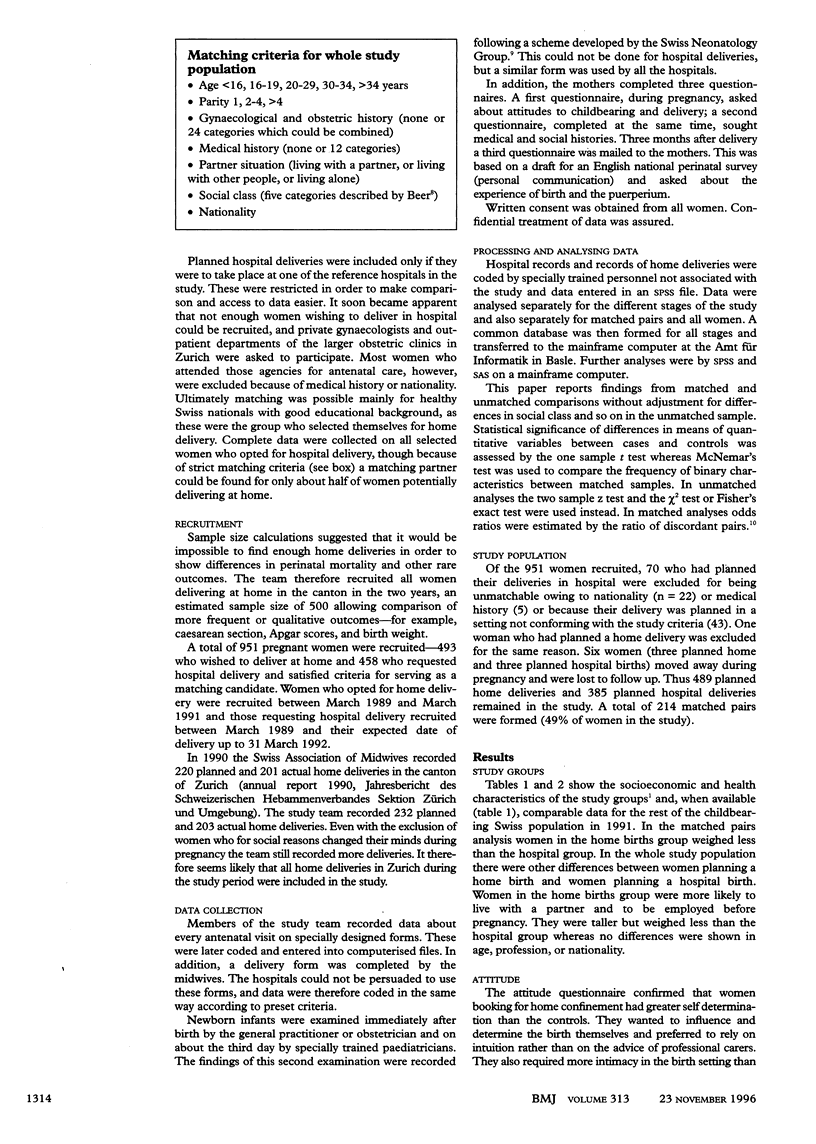
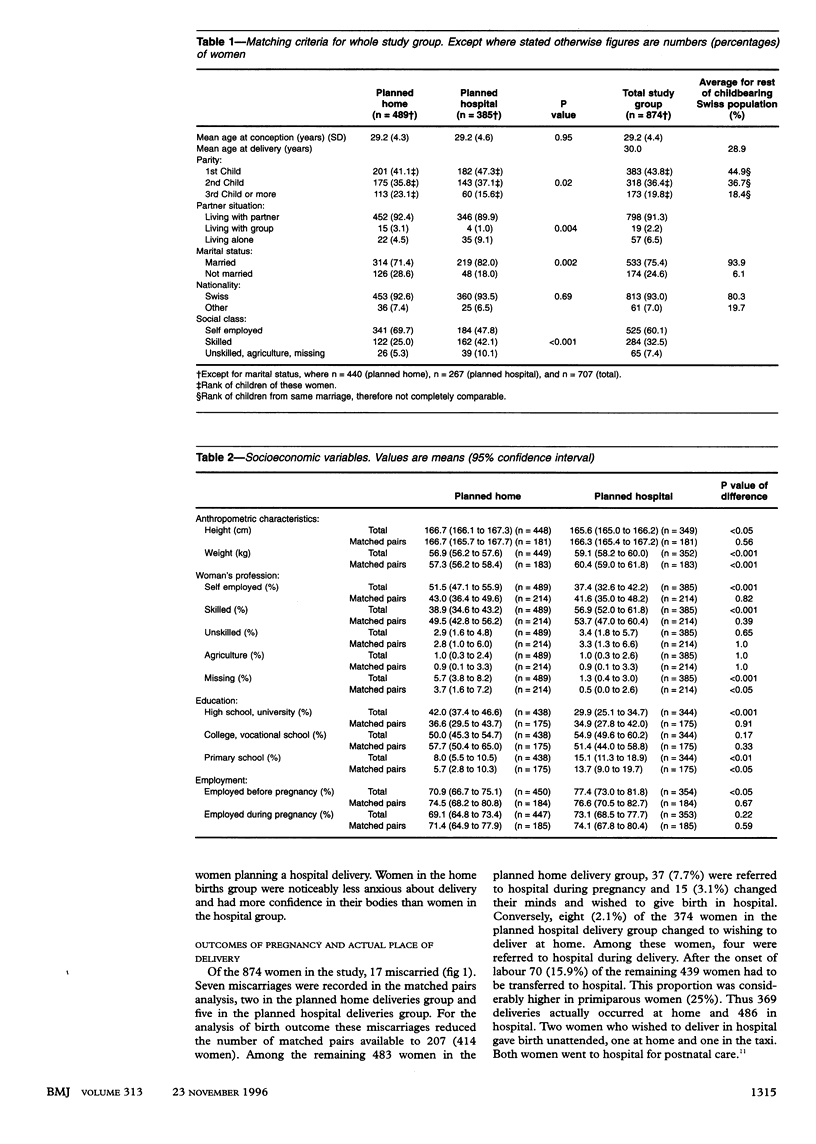
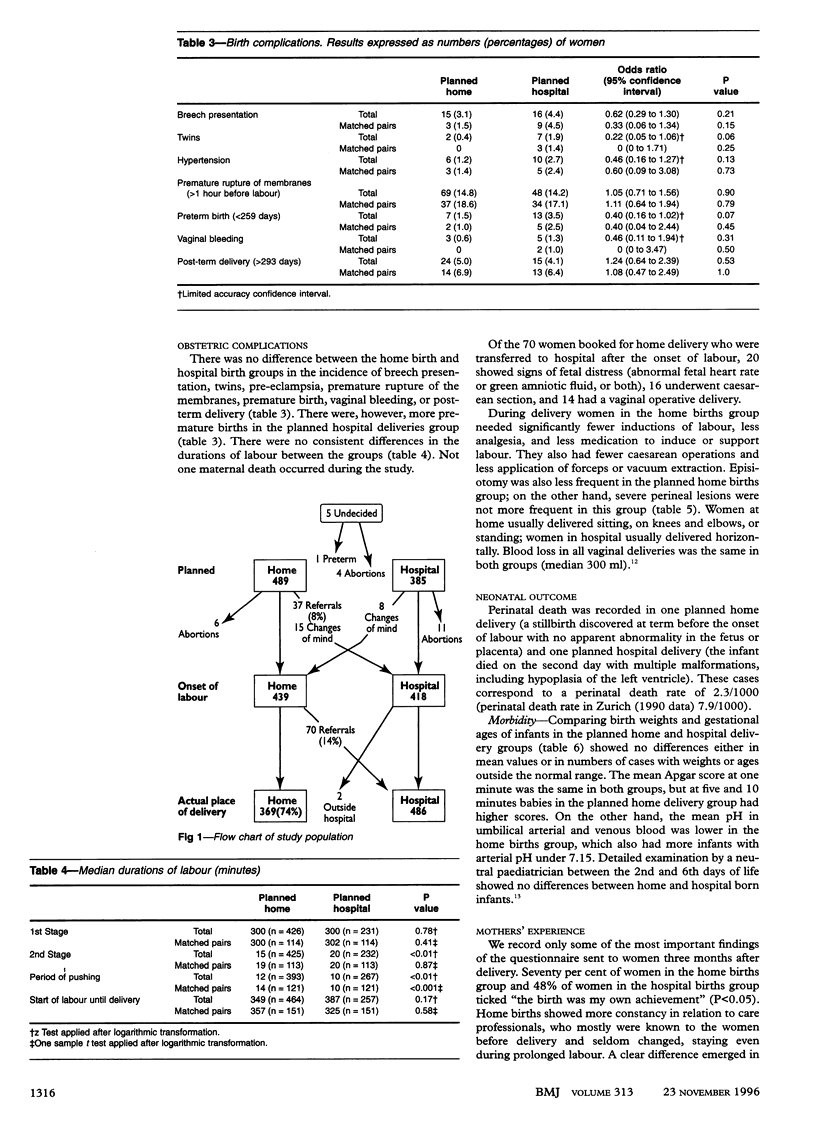
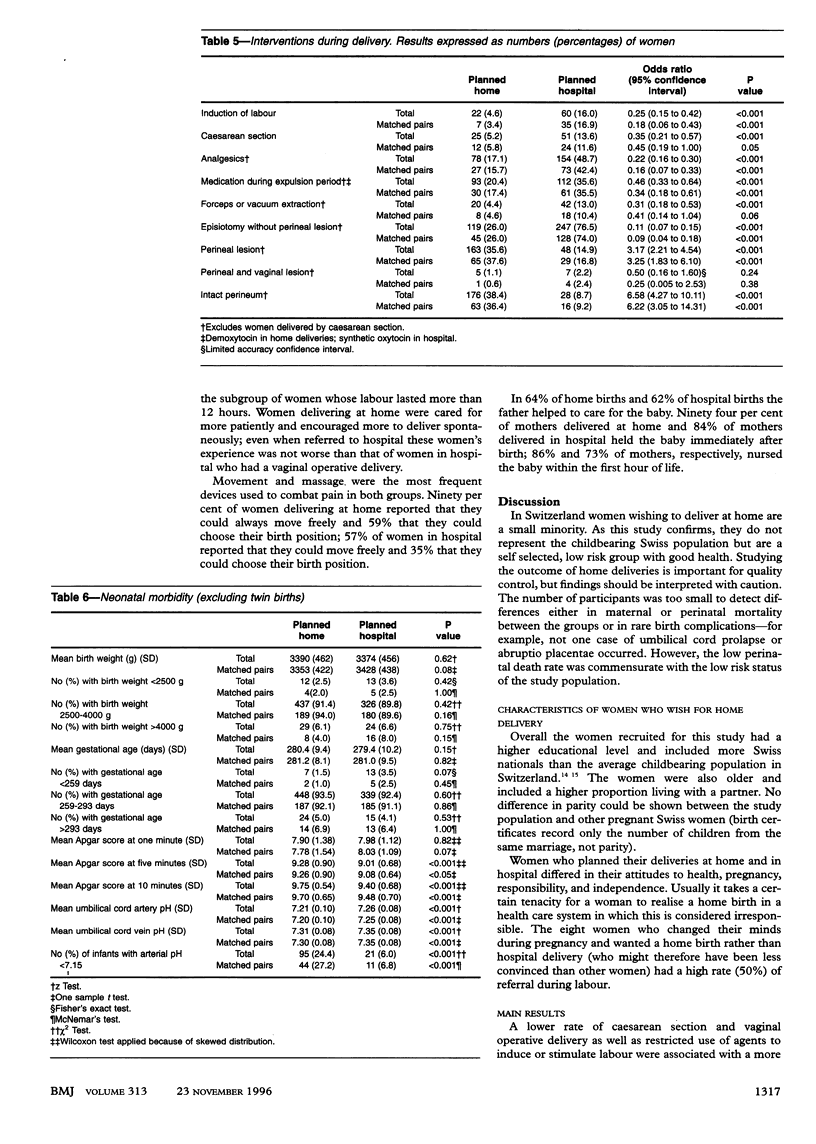
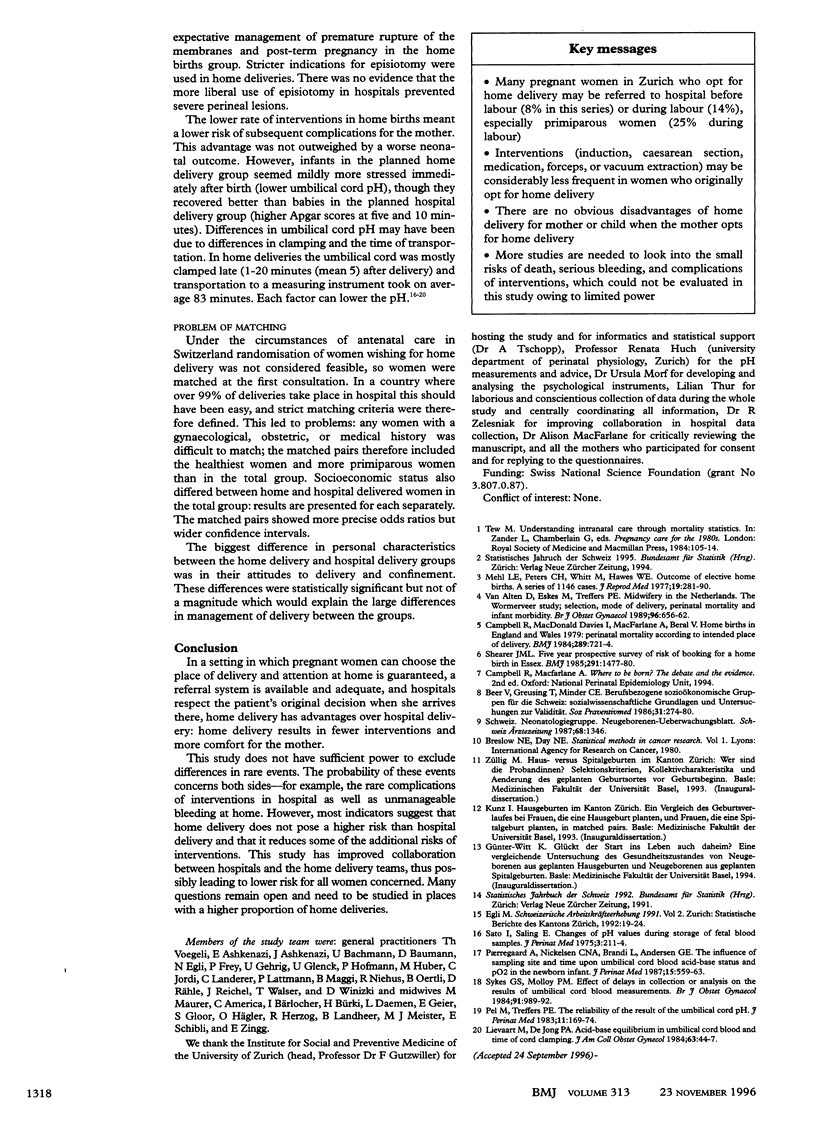
OBJECTIVE: To assess procedures and outcomes in deliveries planned at home versus those planned in hospital among women choosing the place of delivery. DESIGN: Follow up study of matched pairs. SETTING: Antenatal clinics and reference hospitals in Zurich between 1989 and 1992. SUBJECTS: 489 women opting for home delivery and 385 opting for hospital delivery; the women comprised all those attending members of the study team for antenatal care and those attending the reference hospital for antenatal care who could be matched with the women planning home confinement. MAIN OUTCOME MEASURES: Need for medication and incidence of interventions during delivery (caesarean section, forceps, vacuum extraction, episiotomy), duration of labour, occurrence of severe perineal lesions, maternal blood loss, and perinatal morbidity and death. RESULTS: All women were followed up from their first antenatal visit till three months after delivery. Referrals during pregnancy (n = 37) and labour (70), changes of mind (15 home to hospital, eight hospital to home), and 17 miscarriages resulted in 369 births occurring at home and 486 in hospital. During delivery the home birth group needed significantly less medication and fewer interventions whereas no differences were found in durations of labour, occurrence of severe perineal lesions, and maternal blood loss. Perinatal death was recorded in one planned hospital delivery and one planned home delivery (overall perinatal mortality 2.3/1000). There was no difference between home and hospital delivered babies in birth weight, gestational age, or clinical condition. Apgar scores were slightly higher and umbilical cord pH lower in home births, but these differences may have been due to differences in clamping and the time of transportation. CONCLUSION: Healthy low risk women who wish to deliver at home have no increased risk either to themselves or to their babies.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Beer V., Greusing T., Minder C. E. Berufsbezogene sozio-ökonomische Gruppen für die Schweiz: sozialwissenschaftliche Grundlagen und Untersuchungen zur Validität. Soz Praventivmed. 1986;31(6):274–280. doi: 10.1007/BF02077499. [DOI] [PubMed] [Google Scholar]
- Campbell R., Davies I. M., Macfarlane A., Beral V. Home births in England and Wales, 1979: perinatal mortality according to intended place of delivery. Br Med J (Clin Res Ed) 1984 Sep 22;289(6447):721–724. doi: 10.1136/bmj.289.6447.721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lievaart M., de Jong P. A. Acid-base equilibrium in umbilical cord blood and time of cord clamping. Obstet Gynecol. 1984 Jan;63(1):44–47. [PubMed] [Google Scholar]
- Mehl L. E., Peterson G. H., Whitt M., Hawes W. E. Outcomes of elective home births: a series of 1,146 cases. J Reprod Med. 1977 Nov;19(5):281–290. [PubMed] [Google Scholar]
- Paerregaard A., Nickelsen C. N., Brandi L., Andersen G. E. The influence of sampling site and time upon umbilical cord blood acid-base status and PO2 in the newborn infant. J Perinat Med. 1987;15(6):559–563. doi: 10.1515/jpme.1987.15.6.559. [DOI] [PubMed] [Google Scholar]
- Pel M., Treffers P. E. The reliability of the result of the umbilical cord pH. J Perinat Med. 1983;11(3):169–174. doi: 10.1515/jpme.1983.11.3.169. [DOI] [PubMed] [Google Scholar]
- van Alten D., Eskes M., Treffers P. E. Midwifery in The Netherlands. The Wormerveer study; selection, mode of delivery, perinatal mortality and infant morbidity. Br J Obstet Gynaecol. 1989 Jun;96(6):656–662. doi: 10.1111/j.1471-0528.1989.tb03279.x. [DOI] [PubMed] [Google Scholar]


