Abstract
The present randomised phase II study was an effort to evaluate single-agent gemcitabine as a first-line systemic treatment of Asian patients with unresectable hepatocellular carcinoma (HCC). Gemcitabine was given via intravenous infusion at 1250 mg m−2 on days 1 and 8 of 3-week cycles. Patients were randomised to receive gemcitabine as a 30-min intravenous infusion (standard schedule) or at a fixed dose rate (FDR) of 10 mg m−2 min−1. A total of 50 patients were enrolled in the study, of whom 48 received study therapy. One patient on standard schedule had a partial response, for an overall response rate of 2.1% (95% CI: 0.05–11.1%). The median time to progression and survival time were 46 and 97 days, respectively. The overall rates of Grade 3 or 4 haematological and nonhaematological toxicities were 39.6 and 64.6%, respectively, with no significant difference between the two treatment arms. There were no drug-related deaths and severe clinical toxicities were rare. Both schedules of gemcitabine were safe and toxicity was well manageable in this patient population. However, gemcitabine seems no more active than other cytotoxic agents when used alone for systemic treatment of advanced HCC.
Keywords: hepatocellular carcinoma, gemcitabine
Hepatocellular carcinoma (HCC) is a major cause of cancer death, in Asia and worldwide (Pisani et al, 1999). Most patients have inoperable disease at the time of diagnosis and need systemic therapy at some point of their disease. No systemic therapy has shown reproducible benefit in controlled clinical trials and treatment outcome has remained poor (Venook, 1994; Simonetti et al, 1997; Fong et al, 2001).
The antimetabolite gemcitabine (GEMZAR®) is a deoxycytidine analogue (2′,2′-difluorodeoxycytidine, dFdC) that inhibits DNA synthesis (Plunkett et al, 1989). Preclinical studies of gemcitabine have shown promising activity in a human HCC model (Graziadei et al, 1998). A phase II study of single-agent gemcitabine in advanced HCC in Taiwan found a response rate of 17.8% and good tolerance (Yang et al, 2000). In that study, gemcitabine was given as an intravenous infusion over 30 min, which is the standard mode of gemcitabine administration. Preclinical and clinical studies have found that the intracellular accumulation of dFdC triphosphate, the active moiety of gemcitabine incorporated into DNA, gets saturated at gemcitabine levels of 15–20 μmol l−1 and can be maximised by the administration of gemcitabine at a fixed dose rate (FDR) of 10 mg m−2 min−1 (Grunewald et al, 1990, 1991; Abbruzzese et al, 1991; Tempero et al, 1999). In two phase I studies, the maximum tolerated dose of gemcitabine at FDR was found to be 1500 mg m−2 (Brand et al, 1997) and 1800 mg m−2 (Touroutoglou et al, 1998). Both studies suggested a phase II starting dose of 1500 mg m−2. The toxicity profile of FDR gemcitabine was similar to that of the standard schedule, with granulocytopaenia and thrombocytopaenia the dose-limiting toxicities (Brand et al, 1997; Touroutoglou et al, 1998). A randomised phase II study in pancreatic cancer has suggested that FDR gemcitabine may produce higher efficacy than standard schedule (Tempero et al, 1999). The present multinational randomised phase II study was an effort to confirm the previously observed activity of standard schedule gemcitabine in Asian patients with unresectable HCC and to evaluate the activity and toxicity of FDR gemcitabine in this patient population.
PATIENTS AND METHODS
Eligible patients had a tissue diagnosis of HCC or serum alpha-fetoprotein of at least 400 ng l−1 plus liver imaging studies that were considered highly suggestive of HCC. Patients had to have distant metastases (stage IV) or locally advanced disease (stage IIIB) not eligible for curative surgery, and bidimensionally measurable disease. Prior systemic chemotherapy was not allowed. Intra-arterial chemotherapy was allowed if given more than 3 months prior to enrolment and not including more than one cytotoxic drug. Other inclusion criteria included: Karnofsky performance status (KPS) of 70 or higher and estimated life expectancy of at least 12 weeks; age of at least 18 years and no higher than 75 years; white blood cell count ⩾3.0 × 109 l−1, absolute neutrophil count (ANC) ⩾2.0 × 109 l−1, platelets ⩾75 × 109 l−1, haemoglobin ⩾9.0 g dl−1; total serum bilirubin ⩽4 × upper limit of normal (ULN), ALT and AST ⩽4 × ULN, and serum albumin ⩾20 g l−1; serum creatinine ⩽1.5 × ULN; Okuda stage I or II (Okuda et al, 1985); and lastly, written informed consent. Exclusion criteria included: central nervous system metastases; any other concomitant tumour therapy; pregnancy or breastfeeding; active infection, active peptic ulcer, active cardiac disease requiring therapy, unstable diabetes mellitus; other documented malignancy except treated nonmelanoma skin cancer, carcinoma in situ of the cervix, or other cancers diagnosed at least 5 years previously and without recurrence. The study was conducted according to ICH Good Clinical Practice Guidelines, including obtaining informed consent from all patients.
A minimisation randomisation process (Pocock, 1983) was used in which patients were stratified on stage of disease (Okuda I or II), KPS (70–80 or 90–100) and whether they had prior intra-arterial chemotherapy (yes or no). A block size of 4 was used when there was balance between the prognostic factors and a ratio of 3 : 2 with a block size of 5 was used if there was imbalance. In both arms, gemcitabine was given at 1250 mg m−2 as an intravenous infusion on days 1 and 8 of 3-weekly cycles. In the standard schedule arm, gemcitabine was administered over 30 min, in the FDR arm at 10 mg m−2 min−1 (eg, over 125 min for a dose of 1250 mg m−2). An infusion pump was used to ensure exact infusion time. Antiemetics were used according to the standard local practice.
To start a next cycle, ANC had to be ⩾1.0 × 109 l−1, platelets ⩾75 × 109 l−1, AST, ALT and serum bilirubin ⩽4 × ULN, and patients had to have no other toxicity of common toxicity criteria (CTC) Grade 3 or 4 with the exception of nausea, vomiting and anaemia. The dose of gemcitabine was reduced by 20% in a subsequent cycle in the case of ANC <0.5 × 109 l−1 associated with fever (defined as a single episode of ⩾38.5°C or three episodes of ⩾38.5°C during a 24-h period or lasting more than 7 days), platelet count <25 × 109 l−1 or <50 × 109 l−1 associated with bleeding, or AST, ALT or serum bilirubin >4 × ULN at any time during the preceding cycle. If any other toxicity of CTC Grade 3 or 4 occurred during the preceding cycle, with the exception of nausea, vomiting and anaemia, the dose of gemcitabine could be reduced by 20% at the discretion of the investigator. The day 8 dose of gemcitabine was omitted in case of ANC <0.5 × 109 l−1, platelets <50 × 109 l−1, AST, ALT or serum bilirubin >4 × ULN, or any other toxicity of CTC Grade 3 or 4 with the exception of nausea, vomiting and anaemia. Prophylactic use of granulocyte colony-stimulating factor (G-CSF) or granulocyte–macrophage colony-stimulating factor (GM-CSF) was not allowed in this study. Therapeutic CSF was permitted in case of febrile neutropaenia.
Before study enrolment, patients were required to have a physical examination, chest X-ray, abdominal and chest computed tomography, complete blood work-up and ECG. Abdominal ultrasound and bone X-ray and/or scan were optional as clinically indicated. Before the start of each cycle and day 8 dosing of gemcitabine, a physical examination, full blood count and blood work-up were performed. A full blood count was obtained around day 15. Upon discontinuation of study therapy, survival status was assessed until 12 months past randomisation or death, whichever occurred first. If patients had an objective remission or stable disease at the time of discontinuation of study therapy, response status was evaluated every 2 months.
Tumour response status was evaluated every two cycles. Confirmation of response was required at no earlier than 4 weeks. Complete response was defined as complete disappearance of all known disease; partial response as at least 50% reduction in the size of measurable lesions; no change as less than 50% reduction and 25% increase in the size of measurable lesions; and progressive disease as equal to or more than 25% increase in the size of at least one measurable lesion or any appearance of a new lesion. Duration of response and stable disease, and time to progression were measured from the date of randomisation to documented disease progression. Survival time was calculated from the date of randomisation to the date of death or last follow-up. Toxicity was graded according to the National Cancer Institute Common Toxicity Criteria, version 2.0 (National Cancer Institute, 1999).
The primary objective of this study was to evaluate the response rate of either treatment. One of the secondary objectives was to select the gemcitabine schedule with the higher therapeutic ratio (ie, activity vs toxicity) for further study in advanced HCC. Based on the data from Taiwan (Yang et al, 2000), a minimum response rate of 10% was assumed for either arm. The Simon design for randomised phase II studies was applied to select a treatment regimen for further investigation (Simon et al, 1985). Assuming a mean true response rate of 10%, and the true response rate achieved by one treatment to be 10% higher, a total sample size of 56 patients gave a probability of higher than 0.85 such that the better of the two treatments will have the higher observed response rate. Kaplan–Meier statistics were used to estimate time-to-event measures and log rank test was used for comparisons of treatment groups. Toxicity of the two arms was compared using Fisher's exact test.
RESULTS
In total, 50 patients were entered on trial. Two patients did not receive study therapy because they did not meet the eligibility criteria. In all, 25 and 23 patients received gemcitabine at standard schedule and FDR, respectively. Patient enrolment was stopped early. Two reports of no activity by single-agent gemcitabine in advanced HCC (Kubicka et al, 2001; Ulrich-Pur et al, 2001) prompted an unplanned interim analysis, which found one partial response in 42 patients evaluable for response assessment. This level of activity was considered too low to warrant further patient enrolment.
All data reported here are based on the 48 patients who received study therapy. Of these, 26 patients were enrolled in the People's Republic of China, 15 in Thailand, six in South Korea and one in Hong Kong. The two treatment groups were well balanced for major baseline characteristics (Table 1 ). There were 43 male and five female patients. In all, 12 patients had a tissue diagnosis of HCC, and in 36 patients the diagnosis was based on elevation of serum alpha-fetoprotein of higher than 400 ng ml−1 plus liver imaging studies considered as highly suggestive of HCC.
Table 1. Patient and tumour characteristics.
| Standard schedule (n=25) | FDR (n=23) | |
|---|---|---|
| Age (years) | ||
| Median | 48.7 | 49.0 |
| Range | 35.2–70.3 | 31.8–66.7 |
| KPS | ||
| Median | 80 | 80 |
| Range | 70–100 | 70–90 |
| Stage | ||
| IIIB | 4 | 2 |
| IV | 21 | 21 |
| Two or more organ sites involved | 5 | 12 |
| Okuda stage | ||
| I | 12 | 9 |
| II | 13 | 14 |
| Prior therapy | ||
| None | 22 | 20 |
| Surgery | 1 | 2 |
| IACE | 1 | 1 |
| IAE | 1 | 0 |
| History of chronic benign liver disease | ||
| None | 6 | 9 |
| Chronic hepatitis | 12 | 9 |
| Liver cirrhosis | 7 | 5 |
| Hepatitis B serology | ||
| Positive | 18 | 21 |
| Negative | 3 | 0 |
| Unknown | 4 | 2 |
| Hepatitis C serology | ||
| Positive | 5 | 1 |
| Negative | 7 | 11 |
| Unknown | 13 | 11 |
IACE=intra-arterial chemo-embolisation; IAE=intra-arterial embolisation.
Efficacy
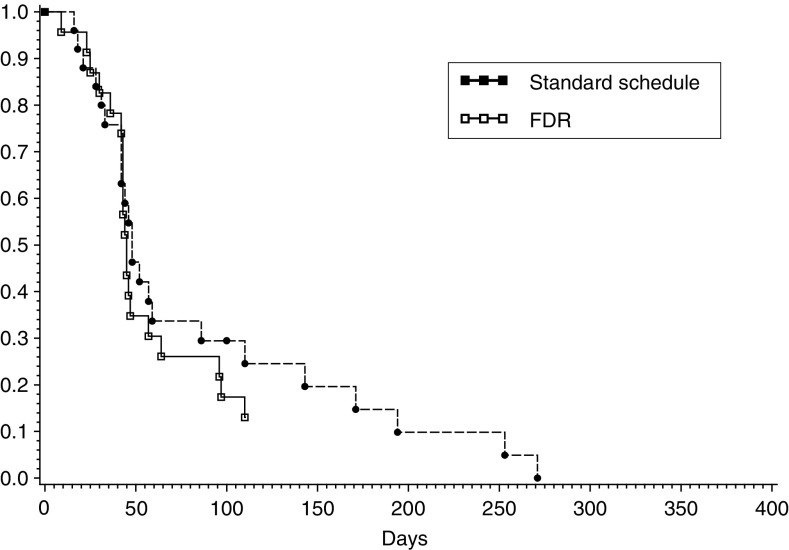
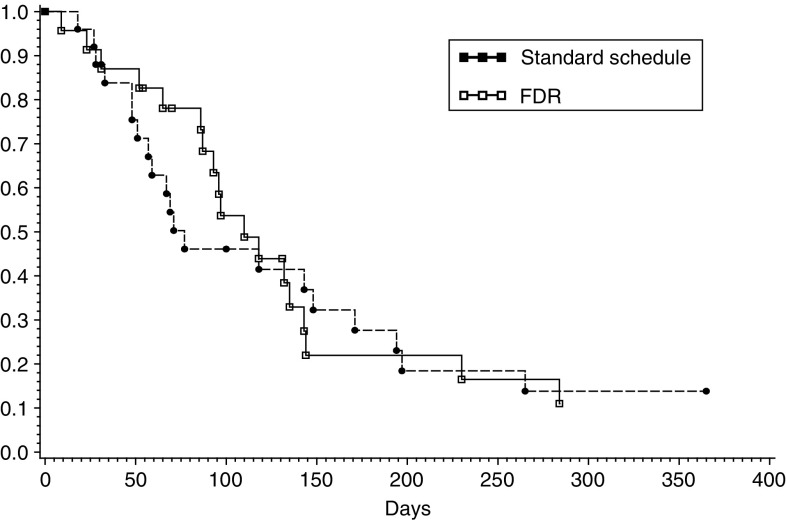
No patient in the FDR arm and one patient in the standard schedule arm had an objective partial response, for an overall response rate of 2.1% (1 out of 48 patients; 95% CI: 0.05–11.1%). The response rates for the standard schedule and FDR arm were 4% (1 out of 25 patients; 95% CI: 0.1–20.4%) and 0% (0 out of 23 patients; 95% CI: 0–14.8%), respectively. The duration of the single partial response was 29.7 weeks. In total, 26 patients (54%) had progressive disease as best response. The time to progression and median survival time were 46 (95% CI: 43–57) and 97 (95% CI: 71–143) days, respectively, with no statistical differences between the two arms (Figures 1 and 2). Five patients (11.6%) were alive at 1 year.
Figure 1.
Time to progression by treatment arm.
Figure 2.
Survival by treatment arm.
Toxicity
In the standard schedule arm, the rates of Grade 3/4 haematological and nonhaematological toxicities were 44.0 and 76.0%, respectively. The corresponding rates in the FDR arm were 34.8 and 52.2%, respectively, with no statistical difference between the two treatment arms. Individual Grade 3/4 toxicities are listed in Table 2 . There were no drug-related deaths. Six patients (12.5%) received G-CSF in 8 out of 113 treatment cycles (7.1%). The number of cycles administered was 73 in the standard schedule and 40 in the FDR arm. The mean number of cycles per patient for the entire study population was 2.35, with a range of 1–6. Five patients completed six cycles of study therapy, all on the standard schedule arm. There were no signs of cumulative toxicity. The most common cause of early discontinuation was disease progression. Dose adjustments in subsequent cycles and on day 8 occurred in four (3.5%) and 36 (32%) cycles, respectively. With a planned dose intensity of 833 mg m−2 week−1 the actual dose intensity achieved was 703.4 mg m−2 week−1, for a relative dose intensity of 0.844. There was no significant difference in dose intensity between the two arms.
Table 2. Grade 3 and 4 toxicities.
|
Standard schedule (n=25) |
FDR (n=23) |
|||
|---|---|---|---|---|
| 3 | 4 | 3 | 4 | |
| Leukopaenia | 2 | 0 | 3 | 0 |
| Neutropaenia | 4 | 1 | 2 | 2 |
| Thrombocytopaenia | 4 | 0 | 1 | 0 |
| Anaemia | 4 | 0 | 3 | 1 |
| Febrile neutropaenia | 0 | 0 | 0 | 0 |
| Infection | 0 | 0 | 1 | 0 |
| Bleeding | 3 | 1 | 0 | 0 |
| AST/ALT | 8 | 0 | 4 | 0 |
| GGT | 7 | 0 | 5 | 0 |
| Bilirubin | 1 | 0 | 2 | 0 |
| Nausea | 0 | 0 | 0 | 0 |
| Vomiting | 0 | 0 | 1 | 0 |
| Skin rash/desquamation | 1 | 0 | 0 | 0 |
| Fatigue | 3 | 0 | 1 | 1 |
DISCUSSION
Hepatocellular carcinoma is known to be highly resistant to chemotherapy (Fong et al, 2001). Doxorubicin is widely considered the most active single-agent, but more recent studies have failed to demonstrate meaningful activity (Lai et al, 1988, 1989; Mok et al, 1999). Newer agents such as raltitrexed, paclitaxel, irinotecan, nolatrexed and eniluracil-5-fluorouracil have shown no activity (Rougier et al, 1997; Chao et al, 1998; Mok et al, 1999; Stuart et al, 1999; Llovet et al, 2001; O'Reilly et al, 2001).
The present study did not show promising activity of single-agent gemcitabine. Preliminary data in advanced pancreatic cancer (Tempero et al, 1999) led us to hypothesise that gemcitabine administered at FDR may achieve higher activity in HCC. However, no objective remission was obtained in the FDR arm of this study. A phase II study of single-agent gemcitabine in Taiwan found a response rate of 17.8% in 28 patients with advanced HCC (Yang et al, 2000). More recently, three studies in Europe and the US have shown no activity (Kubicka et al, 2001; Ulrich-Pur et al, 2001; Fuchs et al, 2002). This discrepancy may suggest differing sensitivity of HCC in Asia vs Western countries. However, the present trial was conducted in three Asian countries and was not able to reproduce the activity reported from Taiwan. The eligibility criteria in the current and Taiwan trial were similar, and so were the reported characteristics of the study patients. However, the median survival in the Taiwan study was 18.7 weeks, while it was 13.9 weeks (97 days) in the present study. This suggests more favourable prognostic features of the patients in the Taiwan study, which may also have increased the probability of tumour response. However, the median survival in the US study was 6.9 months and no objective response was observed (Fuchs et al, 2002). The median survival of 97 days in the current trial is similar to the 3.1 months found for HCC patients classified as intermediate-risk by the Chinese University Prognostic Index (CUPI) (Leung et al, 2002). We performed a retrospective risk classification of the study patients according to the CUPI and found 19 (39.6%) and 28 (58.3%) patients falling in the intermediate- and low-risk categories, respectively. The mean CUPI for the overall population was +1.33 (range, −4 to +9), which is close to the lower CUPI cutoff value of +2 for intermediate risk (Leung et al, 2002). Accordingly, the survival outcome in the present study seems to be consistent with the Hong Kong study (Leung et al, 2002).
Gemcitabine was used at full dose, yet toxicity was well manageable, with a low rate of Grade 3 or 4 clinical toxicities, low need for G-CSF, and no drug-related deaths. The relative dose intensity was 0.844. All other studies of gemcitabine in HCC, used as single agent or in combination with cisplatin or doxorubicin, have shown mild to modest toxicity (Babu et al, 2000; Yang et al, 2000, 2002; Kubicka et al, 2001; Ulrich-Pur et al, 2001; Fuchs et al, 2002). We anticipated higher toxicity for FDR gemcitabine, as has been previously observed (Brand et al, 1997; Tempero et al, 1999). Interestingly, this was not the case. As is common in HCC, many patients in this study had underlying benign chronic liver disease. In Asia, this is typically the result of hepatitis B infection, as was the case in the present study. Of note, no hepatitis flare was observed.
In conclusion, both schedules of gemcitabine were found to be safe and toxicity was well manageable in this patient population, but gemcitabine seems no more active than other cytotoxic agents when used alone for systemic treatment of advanced HCC.
Acknowledgments
We thank Wendy Leung and Joanne Renold for project management, Justine Southby for medical writing support, and Drs O-Tur Saeseow (Khon Kaen University, Khon Kaen, Thailand) and Benjamin CY Wong (The University of Hong Kong, Queen Mary Hospital, Hong Kong, SAR China) for study participation.
References
- Abbruzzese JL, Grunewald R, Weeks EA, Gravel D, Adams T, Nowak B, Mineishi S, Tarassoff P, Satterlee W, Raber MN (1991) A phase I clinical, plasma, and cellular pharmacology study of gemcitabine. J Clin Oncol 9: 491–498 [DOI] [PubMed] [Google Scholar]
- Babu G, Parikh P, Fuloria J, Doval D, Prabhakaran P, Pai VR, Vaid A, Nguyen B, Kapil S (2000) A multicenter phase II trial of gemcitabine and cisplatin in unresectable hepatocellular carcinoma. Ann Oncol 11(Suppl 4): 269P (abstract) [Google Scholar]
- Brand R, Capadano M, Tempero M (1997) A phase I trial of weekly gemcitabine administered as a prolonged infusion in patients with pancreatic cancer and other solid tumors. Invest N Drugs 15: 331–341 [DOI] [PubMed] [Google Scholar]
- Chao Y, Chan WK, Birkhofer MJ, Hu OY, Wang SS, Huang YS, Liu M, Whang-Peng J, Chi KH, Lui WY, Lee SD (1998) Phase II and pharmacokinetic study of paclitaxel therapy for unresectable hepatocellular carcinoma patients. Br J Cancer 78: 34–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fong Y, Kemeny N, Lawrence T (2001) Cancer of the liver and biliary tree. In Cancer: Principles and Practice of Oncology, DeVita V, Hellman S, Rosenberg S (eds) pp 1162–1203. Philadelphia, PA: JB Lippincott [Google Scholar]
- Fuchs CS, Clark JW, Ryan DP, Kulke MH, Kim H, Earle CC, Vincitore M, Mayer RJ, Stuart KE (2002) A phase II trial of gemcitabine in patients with advanced hepatocellular carcinoma. Cancer 94: 3186–3191 [DOI] [PubMed] [Google Scholar]
- Graziadei I, Kelly T, Schirmer M, Geisen FH, Vogel W, Kowalinka G (1998) Antitumor effect of the nucleoside analogs 2-chlordeoxyadenosine and 2′,2′-difluorodeoxycytidine on human hepatoma HepG2 cells. J Hepatol 28: 504–509 [DOI] [PubMed] [Google Scholar]
- Grunewald R, Abbruzzese JL, Tarassoff P, Plunkett W (1991) Saturation of 2′,2′-difluorodeoxycytidine 5′-triphosphate accumulation by mononuclear cells during a phase I trial of gemcitabine. Cancer Chemother Pharmacol 27: 258–262 [DOI] [PubMed] [Google Scholar]
- Grunewald R, Kantarjian H, Keating MJ, Abbruzzese J, Tarassoff P, Plunkett W (1990) Pharmacologically directed design of the dose rate and schedule of 2′,2′-difluorodeoxycytidine (gemcitabine) administration in leukemia. Cancer Res 50: 6823–6826 [PubMed] [Google Scholar]
- Kubicka S, Rudolph KL, Tietze MK, Lorenz M, Manns M (2001) Phase II study of systemic gemcitabine chemotherapy for advanced unresectable hepatobiliary carcinomas. Hepatogastroenterology 48: 783–789 [PubMed] [Google Scholar]
- Lai CL, Wu PC, Chan GC, Lok AS, Lin HJ (1988) Doxorubicin versus no antitumor therapy in inoperable hepatocellular carcinoma. A prospective randomized trial. Cancer 62: 479–483 [DOI] [PubMed] [Google Scholar]
- Lai CL, Wu PC, Lok AS, Lin HJ, Ngan H, Lau JY, Chung HT, Ng MM, Yeoh EK, Arnold M (1989) Recombinant alpha 2 interferon is superior to doxorubicin for inoperable hepatocellular carcinoma: a prospective randomised trial. Br J Cancer 60: 928–933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung TWT, Tang AMY, Zee B, Yu SCH, Lai PBS, Lau WY, Johnson PJ (2002) Factors predicting response and survival in 149 patients with unresectable hepatocellular carcinoma treated by combination cisplatin, interferon-alpha, doxorubicin and 5-fluorouracil chemotherapy. Cancer 94: 421–427 [DOI] [PubMed] [Google Scholar]
- Llovet JM, Ruff P, Tassopoulos N, Castells L, Bruix J, El-Hariry I, Peachey M (2001) A phase II trial of oral eniluracil/5-fluorouracil in patients with inoperable hepatocellular carcinoma. Eur J Cancer 37: 1352–1358 [DOI] [PubMed] [Google Scholar]
- Mok TSK, Leung TWT, Lee S-D, Chao Y, Chan ATC, Huang A, Lui M-C, Yeo W, Chak K, Johnston A, Johnson P (1999) A multi-centre randomized phase II study of nolatrexed versus doxorubicin in treatment of Chinese patients with advanced hepatocellular carcinoma. Cancer Chemother Pharmacol 44: 307–311 [DOI] [PubMed] [Google Scholar]
- National Cancer Institute (1999), National Cancer Institute Common Toxicity Criteria (version 2), Bethesda, MD: Division of Cancer Treatment and Diagnosis, National Cancer Institute http://ctep.info.nih.gov/ctc3/ctc.htm
- Okuda K, Ohtsuki T, Obata H, Tomimatsu M, Okazaki N, Hasegawa H, Nakajima Y, Ohnishi K (1985) Natural history of hepatocellular carcinoma and prognosis in relation to treatment. Study of 850 patients. Cancer 56: 918–928 [DOI] [PubMed] [Google Scholar]
- O'Reilly EM, Stuart KE, Sanz-Altamira PM, Schwartz GK, Steger CM, Raeburn L, Kemeny NE, Kelsen DP, Saltz LB (2001) A phase II study of irinotecan in patients with advanced hepatocellular carcinoma. Cancer 91: 101–105 [DOI] [PubMed] [Google Scholar]
- Pisani P, Parkin DM, Bray FI, Ferlay J (1999) Estimates of the world-wide mortality from twenty-five major cancers in 1990. Int J Cancer 83: 18–2910449602 [Google Scholar]
- Plunkett W, Gandhi V, Chubb S, Novak B, Heinemann V, Mineishi S, Sen A, Herter L, Grindey GB (1989) 2′,2′-Difluorodeoxycytidine metabolism and mechanism of action in human leukemia cells. Nucleosides Nucleotides 8: 775–785 [Google Scholar]
- Pocock SJ (1983) Clinical Trials: A Practical Approach. Chichester: John Wiley & Sons [Google Scholar]
- Rougier P, Ducreux M, Kerr D, Carr BI, Francois E, Adenis A, Seymour L (1997) A phase II study of raltitrexed (‘Tomudex’) in patients with hepatocellular carcinoma. Ann Oncol 8: 500–502 [DOI] [PubMed] [Google Scholar]
- Simon R, Wittes RE, Ellenberg SS (1985) Randomized phase II clinical trials. Cancer Treat Rep 69: 1375–1381 [PubMed] [Google Scholar]
- Simonetti RG, Liberati A, Angiolini C, Pagliaro L (1997) Treatment of hepatocellular carcinoma: a systematic review of randomized controlled trials. Ann Oncol 8: 117–136 [DOI] [PubMed] [Google Scholar]
- Stuart K, Tessitore J, Rudy J, Clendennin N, Johnston A (1999) A phase II trial of nolatrexed dihydrochloride in patients with advanced hepatocellular carcinoma. Cancer 86: 410–414 [PubMed] [Google Scholar]
- Tempero M, Plunkett W, Ruiz van Haperen V, Hainsworth J, Hochster H, Lenzi R, Abbruzzese J (1999) Randomized phase II trial of dose intense gemcitabine by standard infusion vs fixed dose rate in metastatic pancreatic adenocarcinoma. Proc Am Soc Clin Oncol 18: 1048 (abstract) [DOI] [PubMed] [Google Scholar]
- Touroutoglou N, Gravel D, Raber MN, Plunkett W, Abbruzzese JL (1998) Clinical results of a pharmacodynamically based strategy for higher dosing of gemcitabine in patients with solid tumors. Ann Oncol 9: 1003–1008 [DOI] [PubMed] [Google Scholar]
- Ulrich-Pur H, Kornek GV, Fiebiger W, Schull B Raderer M, Scheithauer W (2001) Treatment of advanced hepatocellular carcinoma with biweekly high-dose gemcitabine. Oncology 60: 313–315 [DOI] [PubMed] [Google Scholar]
- Venook AP (1994) Treatment of hepatocellular carcinoma: too many options? J Clin Oncol 12: 1323–1334 [DOI] [PubMed] [Google Scholar]
- Yang T-S, Lin Y-C, Chen J-S, Wang H-M, Wang C-H (2000) Phase II study of gemcitabine in patients with advanced hepatocellular carcinoma. Cancer 89: 750–756 [DOI] [PubMed] [Google Scholar]
- Yang TS, Wang CH, Hsieh RK, Chen JS, Fung MC (2002) Gemcitabine and doxorubicin for the treatment of patients with advanced hepatocellular carcinoma: a phase I–II trial. Ann Oncol 13: 1771–1778 [DOI] [PubMed] [Google Scholar]