It is reported that 35% to 40% of infertile men have a palpable varicocele (dilated testicular veins), whereas the prevalence of a varicocele in the general male population is about 15%.1,2,3 Although varicoceles have been associated with impaired male fertility potential, it is also clear that a significant proportion of men with a varicocele (about 75%) are fertile.2,4,5 As such, a cause and effect relationship between varicocele and male infertility has not been conclusively established.6 The effect of varicocelectomy on male fertility is also controversial.6–10 Uncontrolled studies have generally shown improved semen quality and pregnancy outcome after surgery.11 On the other hand, the results of randomized controlled studies of varicocelectomy for clinical varicocele (only a few such studies are published) are equivocal.12–15
Despite the absence of clear evidence for a positive effect of varicocelectomy, many clinicians consider the data sufficient to support the practice of this surgery, and varicocele is the most commonly treated condition in men with infertility in North America.8 The benefit of varicocele repair must be balanced by the risk associated with the procedure itself. As such, it is important to select the procedure with the highest success and lowest complication rate. Also, it is important to consider assisted reproductive technologies (ARTs) as an alternative to varicocelectomy in infertile couples.16
Etiology of varicocele
The etiology of varicocele is multifactorial. The anatomic differences between the left and right internal spermatic vein (accounting for the predominance of left-sided varicocele), the incompetence of venous valves resulting in reflux of venous blood and increased hydrostatic pressure are the most popular theories.17,18 Increased intra- abdominal pressure during childhood and early adolescence may be a predisposing factor in the development of a varicocele.19
Mechanisms of varicocele-induced pathology
Scrotal and intratesticular temperatures are elevated in humans and in experimental animal models with varicocele, and varicocelectomy may reduce testicular temperature.20–24 Scrotal hyperthermia likely represents the primary factor by which a varicocele affects endocrine function and spermatogenesis, both sensitive to temperature elevation (testicular proteins exhibit a reduced thermal stability compared with proteins from other organs).25,26,27 The detrimental effect of hyperthermia may also be exerted on the epididymis.28 Experimental elevations in epididymal temperature reduce the storage capacity of this organ, resulting in decreased sperm count and quality in the ejaculate.28
Increased hydrostatic pressure in the internal spermatic vein from renal vein reflux may also be responsible for varicocele-induced pathology.29
Pathophysiology of varicocele
The adverse effect of varicocele on male fertility is most clearly manifested by the testicular atrophy generally associated with this condition.4 Using scrotal ultrasound, we objectively demonstrated that left testicular volume is less than right testicular volume in men with a left varicocele.30
A varicocele is associated with bilateral spermatogenic abnormalities and Leydig cell dysfunction.31–35 The testicular histology in infertile men with varicocele is variable, but most studies report reduced spermatogenesis (hypospermatogenesis). The observed increase in germ cell apoptosis is thought to occur as a result of hyperthermia and low testosterone levels in the testicle.26 Testosterone concentration (testosterone is secreted by Leydig cells) is lower in older (> 30 yr) compared with younger men with varicocele, which is a trend not seen in men without varicocele and suggests a progressive, adverse effect of varicocele on Leydig cell function.4
MacLeod (1965) and other investigators observed that most semen samples from infertile men with varicocele have poorer sperm parameters (lower sperm counts, increased number of spermatozoa with abnormal forms and decreased sperm motility) than fertile men.4,23,36 However, this “stress pattern” is not a specific marker for varicocele and therefore is not diagnostic of this condition.37 Surprisingly, few studies have been conducted over the past 40 years to better define the pathophysiology of varicocele, in particular, the effect of this prevalent condition on human sperm function. This is especially critical in light of the inherent limitations (e.g., high biological variability) and modest predictive value of the standard sperm parameters in terms of reproductive outcomes.38,39
Varicocelectomy approaches
There are several approaches for varicocelectomy. These include retroperitoneal and conventional inguinal open techniques, microsurgical inguinal and subinguinal approaches, laparoscopic repairs and radiographic embolization.40,41,42,43,44 The microsurgical varicocelectomy is considered the “gold standard” because it is associated with the lowest risk of complications (varicocele recurrence, hydrocele formation [fluid collection around the testicle] and testicular atrophy).41,45,46,47
We have favoured the microsurgical subinguinal approach because it is associated with a higher success rate (disappearance of varicocele) and a lower complication rate (recurrence rate and hydrocele formation), compared with non- microsurgical techniques.46,48 The subinguinal approach is also associated with less operative and postoperative pain than inguinal approaches.49,50 However, the subinguinal approach is more challenging owing to the greater number of vessels (arteries and veins) encountered at this level, compared with the inguinal canal.51
Microsurgical sub-inguinal varicocelectomy
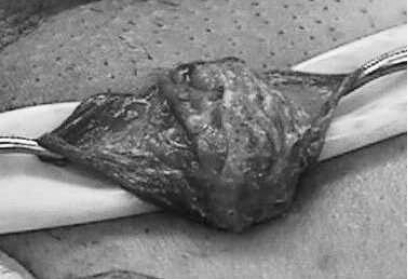
We start with a 2–3-cm oblique skin incision centred over the external inguinal ring, as previously described.52 The incision is deepened through Camper's and Scarpa's fascias and the spermatic cord is then grasped with a Babcock clamp, delivered and placed over a large (1-inch) Penrose drain. The testicle is then delivered and the gubernacular veins and external spermatic perforators are isolated and divided (Fig. 1). The testicle is returned to the scrotum and the spermatic cord is elevated on a large Penrose drain. The microscope is then brought into the operating field and the cord examined under 8–15 power magnification. The internal and external spermatic fascias are incised and the cord structures are again examined (Fig. 2).
Figure 1.
Testicle delivered through the subinguinal incision depicting the spermatic cord (held by Penrose drain; bottom left) and the gubernaculum (held by Penrose drain; right).
Figure 2.
Spermatic cord with Penrose drain beneth it (the internal and external spermatic fascias have been opened).
To simplify the procedure and protect the vas deferens and its vessels from potential injury during subsequent cord dissection, we first create a window between the internal spermatic vessels and the external spermatic fascia so that the internal spermatic vessels are separate from the external spermatic fascia and its associated structures (cremasteric fibres, external spermatic vessels, vas deferens and its vessels).52 A second Penrose drain is then introduced between the internal spermatic vessels and the external spermatic fascia and its associated structures.
We first dissect the contents of the internal spermatic fascia (lying on top of the most superficial Penrose drain). Subtle pulsations will usually reveal the location of the underlying internal spermatic artery (or arteries). Once identified, the artery is dissected free of all surrounding veins and encircled with a 2-0 silk ligature for identification. Care is taken to identify a number of lymphatics (usually 2–5 channels) and these are also encircled with a 2-0 silk ligature. All internal spermatic veins are clipped or ligated (with 4-0 silk) and divided. At the end of the first dissection, the cord is skeletonized so that only the identified artery (or arteries) and lymphatics are preserved.
We then elevate and dissect the contents of the external spermatic fascia (lying between the 2 Penrose drains). The vas deferens and its associated vessels are readily identified and preserved. Any cremasteric artery is also preserved. The remaining cremasteric fibres and veins are ligated and cut thus skeletonizing the cord. At the completion of varicocelectomy, the cord should contain only the testicular artery or arteries, vas deferens, and associated vessels and spermatic cord lymphatics. The wound is irrigated with 1% Neomycin irrigation, and Scarpa's and Camper's fascia are closed with a single 3-0 chromic catgut suture. The incision is infiltrated with 0.5% Marcaine solution with epinephrine, and the skin is closed with a running 4-0 Vicryl subcuticular closure reinforced with Steri-Strips. A dry sterile dressing is applied.
Summary
A variety of approaches have been advocated for management of varicoceles but recent evidence supports the premise that the microsurgical technique is the “gold standard.”46,48 In a number of studies, it has been shown that microsurgical varicocelectomy (inguinal or subinguinal) is superior to non-microsurgical procedures with respect to the development of postoperative complications such as hydrocele or recurrence.41,46,47 Hydrocele formation is believed to be due to ligation of lymphatic channels and recurrence generally results from incomplete ligation of collateral venous channels.53,54 Magnification of the spermatic cord with the use of the operating microscope reduces the potential for development of such complications.41,46,47 However, microsurgical varicocelectomy, particularly the subinguinal approach, remains a technically challenging procedure that requires microsurgical expertise.
Footnotes
This article has been peer reviewed.
Competing interests None declared.
References
- 1.Clarke BG. Incidence of varicocele in normal men and among men of different ages. JAMA 1966;198:1121-2. [PubMed] [Google Scholar]
- 2.Lipshultz LI, Corriere JN. Progressive testicular atrophy in the varicocele patient. J Urol 1977;117:175. [DOI] [PubMed] [Google Scholar]
- 3.Akbay E, Cayan S, Doruk E, et al. The prevalence of varicocele and varicocele-related testicular atrophy in Turkish children and adolescents. BJU Int 2000;86:490-3. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. The influence of varicocele on parameters of fertility in a large group of men presenting to infertility clinics. Fertil Steril 1992;57:1289-92. [PubMed] [Google Scholar]
- 5.Pinto KJ, Kroovand RL, Jarow JP. Varicocele related testicular atrophy and its predictive effect upon fertility. J Urol 1994;152:788-90. [DOI] [PubMed] [Google Scholar]
- 6.Jarow JP. Effects of varicocele on male fertility. Hum Reprod Update 2001;7:59-64. [DOI] [PubMed] [Google Scholar]
- 7.Kamischke A, Nieschlag E. Varicocele treatment in the light of evidence-based andrology. Hum Reprod Update 2001;7:65-9. [DOI] [PubMed] [Google Scholar]
- 8.Sharlip ID, Jarow JP, Belker AM, et al. Best practice policies for male infertility. Fertil Steril 2002;77:873-82. [DOI] [PubMed] [Google Scholar]
- 9.Evers JL, Collins JA. Assessment of efficacy of varicocele repair for male subfertility a systematic review. Lancet 2003;361:1849-52. [DOI] [PubMed] [Google Scholar]
- 10.Ficarra V, Cerruto MA, Liguori G, et al. Treatment of varicocele in subfertile men The Cochrane Review–a contrary opinion. Eur Urol 2006;49:258-63. [DOI] [PubMed] [Google Scholar]
- 11.Schlesinger MH, Wilets IF, Nagler HM. Treatment outcome after varicocelectomy A critical analysis. Urol Clin North Am 1994;21:517-29. [PubMed] [Google Scholar]
- 12.Nilsson S, Edvinsson A, Nilsson B. Improvement of semen and pregnancy rate after ligation and division of internal spermatic vein fact or fiction? Br J Urol 1979;51:591-6. [DOI] [PubMed] [Google Scholar]
- 13.Madgar I, Weissenberg R, Lunenfeld B, et al. Controlled trial of high spermatic vein ligation for varicocele in infertile men. Fertil Steril 1995;63:120-4. [DOI] [PubMed] [Google Scholar]
- 14.Nieschlag E, Hertle L, Fischedick A, et al. Update on treatment of varicocele counselling as effective as occlusion of the vena spermatica. Hum Reprod 1998;13:2147-50. [DOI] [PubMed] [Google Scholar]
- 15.Krause W, Muller HH, Schafer H, et al. Does treatment of varicocele improve male fertility? Results of the ‘Deutsche Varikozelenstudie', a multicentre study of 14 collaborating centres. Andrologia 2002;34:164-71. [DOI] [PubMed] [Google Scholar]
- 16.Kamal KM, Jarvi K, Zini A. Microsurgical varicocelectomy in the era of assisted reproductive technology influence of initial semen quality on pregnancy rates. Fertil Steril 2001;75:1013-6. [DOI] [PubMed] [Google Scholar]
- 17.Buschi AJ, Harrison RB, Brenbridge AN, et al. Distended left renal vein CT/sonographic normal variant. Am J Radiol 1980;135:339-42. [DOI] [PubMed] [Google Scholar]
- 18.Braedel HU, Steffens J, Ziegler M, et al. A possible ontogenic etiology for idiopathic left varicocele. J Urol 1994;151:62-6. [DOI] [PubMed] [Google Scholar]
- 19.Scaramuzza A, Tavana R, Marchi A. Varicoceles in young soccer players. Lancet 1996;348:1180-1. [DOI] [PubMed] [Google Scholar]
- 20.Zorgniotti AW, MacLeod J. Studies in temperature, human semen quality, and varicocele. Fertil Steril 1973;24:854-63. [PubMed] [Google Scholar]
- 21.Saypol DC, Howards SS, Turner TT. Influence of surgically induced varicocele on testicular blood flow, temperature, and histology in adult rats and dogs. J Clin Invest 1981;68:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goldstein M, Eid JF. Elevation of intratesticular and scrotal skin surface temperature in men with varicocele. J Urol 1989;142:743-5. [DOI] [PubMed] [Google Scholar]
- 23.Ali JI, Weaver DJ, Weinstein SH, et al. Scrotal temperature and semen quality in men with and without varicocele. Arch Androl 1990;24:215-9. [DOI] [PubMed] [Google Scholar]
- 24.Wright EJ, Young GP, Goldstein M. Reduction in testicular temperature after varicocelectomy in infertile men. Urology 1997;50:257-9. [DOI] [PubMed] [Google Scholar]
- 25.Mieusset R, Bujan L, Plantavid M, et al. Increased levels of serum follicle-stimulating hormone and luteinizing hormone associated with intrinsic testicular hyperthermia in oligospermic infertile men. J Clin Endocrinol Metab 1989;68:419-25. [DOI] [PubMed] [Google Scholar]
- 26.Lue YH, Lasley BL, Laughlin LS, et al. Mild testicular hyperthermia induces profound transitional spermatogenic suppression through increased germ cell apoptosis in adult cynomolgus monkeys (Macaca fascicularis). J Androl 2002;23:799-805. [PubMed] [Google Scholar]
- 27.Sarge KD, Bray AE, Goodson ML. Altered stress response in testis. Nature 1995;374:126. [DOI] [PubMed] [Google Scholar]
- 28.Bedford JM. Effects of elevated temperature on the epididymis and testis experimental studies. Adv Exp Med Biol 1991;286:19-32. [DOI] [PubMed] [Google Scholar]
- 29.Shafik A, Bedeir GA. Venous tension patterns in cord veins in normal and varicocele individuals. J Urol 1980;123:383-5. [DOI] [PubMed] [Google Scholar]
- 30.Zini A, Buckspan M, Berardinucci D, et al. The influence of clinical and subclinical varicocele on testicular volume. Fertil Steril 1997;68:671-4. [DOI] [PubMed] [Google Scholar]
- 31.Dubin L, Hotchkiss RS. Testis biopsy in subfertile men with varicocele. Fertil Steril 1969;20:50-7. [PubMed] [Google Scholar]
- 32.Comhaire F, Vermeulen A. Plasma testosterone in patients with varicocele and sexual inadequacy. J Clin Endocrin Metab 1975;40:824-9. [DOI] [PubMed] [Google Scholar]
- 33.Johnsen SG, Agger P. Quantitative evaluation of testicular biopsies in varicocele. Fertil Steril 1978a;29:52-7. [DOI] [PubMed] [Google Scholar]
- 34.Hudson RW. The endocrinology of varicoceles. Fertil Steril 1988;49:199-208. [DOI] [PubMed] [Google Scholar]
- 35.Su LM, Goldstein M, Schlegel PN. The effect of varicocelectomy on serum testosterone levels in infertile men with varicoceles. J Urol 1995;154:1752-5. [PubMed] [Google Scholar]
- 36.Macleod J. Seminal cytology in the presence of varicocele. Fertil Steril 1965;16:735-57. [DOI] [PubMed] [Google Scholar]
- 37.Ayodeji O, Baker HW. Is there a specific abnormality of sperm morphology in men with varicoceles? Fertil Steril 1986;45:839-42. [DOI] [PubMed] [Google Scholar]
- 38.Guzick DS, Overstreet JW, Factor-Litvak P, et al; National Cooperative Reproductive Medicine Network. Sperm morphology, motility, and concentration in fertile and infertile men. N Engl J Med 2001;345:1388-93. [DOI] [PubMed] [Google Scholar]
- 39.Menkveld R, Wong WY, Lombard CJ, et al. Semen parameters, including WHO and strict criteria morphology, in a fertile and subfertile population an effort towards standardization of in-vivo thresholds. Hum Reprod 2001;16:1165-71. [DOI] [PubMed] [Google Scholar]
- 40.Walsh PC, White RI. Balloon occlusion of the internal spermatic vein for the treatment of varicoceles. JAMA 1981;246:1701. [PubMed] [Google Scholar]
- 41.Goldstein M, Gilbert BR, Dicker AP, et al. Microsurgical inguinal varicocelectomy with delivery of the testis An artery and lymphatic sparing technique. J Urol 1992;148:1808-11. [DOI] [PubMed] [Google Scholar]
- 42.Donovan JF, Winfield HN. Laparoscopic varix ligation. J Urol 1992;147:77. [DOI] [PubMed] [Google Scholar]
- 43.Jarow JP, Assimos DJ, Pittaway DE. Effectiveness of laparoscopic varicocelectomy. Urology 1993;42:544-7. [DOI] [PubMed] [Google Scholar]
- 44.Enquist E, Stein BS, Sigman M. Laparoscopic versus subinguinal varicocelectomy a comparative study. Fertil Steril 1994;61:1092-6. [DOI] [PubMed] [Google Scholar]
- 45.Murray RR, Mitchell SE, Kadir S, et al. Comparison of recurrent varicocele anatomy following surgery and percutaneous balloon occlusion. J Urol 1986;135:286-9. [DOI] [PubMed] [Google Scholar]
- 46.Cayan S, Kadioglu TC, Tefekli A, et al. Comparison of results and complications of high ligation surgery and microsurgical high inguinal varicocelectomy in the treatment of varicocele. Urology 2000;55:750-4. [DOI] [PubMed] [Google Scholar]
- 47.Grober ED. O'brien J, Jarvi KA, Zini A. Preservation of testicular arteries during subinguinal microsurgical varicocelectomy clinical considerations. J Androl 2004;25:740-3. [DOI] [PubMed] [Google Scholar]
- 48.Ghanem H, Anis T, El-Nashar A, et al. Subinguinal microvaricocelectomy versus retroperitoneal varicocelectomy comparative study of complications and surgical outcome. Urology 2004;64:1005-9. [DOI] [PubMed] [Google Scholar]
- 49.Gontero P, Pretti G, Fontana F, et al. Inguinal versus subinguinal varicocele vein ligation using magnifying loupe under local anesthesia which technique is preferable in clinical practice? Urology 2005;66:1075-9. [DOI] [PubMed] [Google Scholar]
- 50.Al-Kandari AM, Shabaan H, Ibrahim HM, et al. Comparison of outcomes of different varicocelectomy techniques open inguinal, laparoscopic, and subinguinal microscopic varicocelectomy a randomized clinical trial. Urology 2007;69:417-20. [DOI] [PubMed] [Google Scholar]
- 51.Hopps CV, Lemer ML, Schlegel PN, et al. Intraoperative varicocele anatomy a microscopic study of the inguinal versus subinguinal approach. J Urol 2003;170:2366-70. [DOI] [PubMed] [Google Scholar]
- 52.Zini A, Fischer MA, Bellack D, et al. Technical modification of microsurgical varicocelectomy can reduce operating time. Urology 2006;67:803-6. [DOI] [PubMed] [Google Scholar]
- 53.Kaufman SL, Kadir S, Barth KH, et al. Mechanisms of recurrent varicocele after balloon occlusion or surgical ligation of the internal spermatic vein. Radiology 1983;147:435-40. [DOI] [PubMed] [Google Scholar]
- 54.Szabo R, Kessler R. Hydrocele following internal spermatic vein ligation A retrospective study and review of the literature. J Urol 1984;132:924-5. [DOI] [PubMed] [Google Scholar]