Abstract
INTRODUCTION
Accurate and legible medical records are essential to good quality patient care. Guidelines from The Royal College of Surgeons of England (RCSE) state the content required to form a complete medical record, but do not address legibility. An audit of otolaryngology emergency clinic record keeping was performed using a new scoring system.
PATIENTS AND METHODS
The Adjusted Note Keeping and Legibility (ANKLe) score was developed as an objective and quantitative method to assess both the content and legibility of case notes, incorporating the RCSE guidelines. Twenty consecutive otolaryngology emergency clinic case notes from each of 7 senior house officers were audited against standards for legibility and content using the ANKLe score. A proforma was introduced to improve documentation and handwriting advice was given. A further set of 140 notes (20 notes for each of the 7 doctors) was audited in the same way to provide feedback.
RESULTS
The introduction of a proforma and advice on handwriting significantly increased the quality of case note entries in terms of content, legibility and overall ANKLe score.
CONCLUSIONS
Accurate note keeping can be improved by the use of a proforma. The legibility of handwriting can be improved using simple advice. The ANKLe score is an objective assessment tool of the overall quality of medical note documentation which can be adapted for use in other specialties.
Keywords: Medical audit, Medical records, Handwriting, Quality
Good record keeping is essential for good patient care. Accurate medical records are also important for research, audit and have medicolegal ramifications. Many litigation cases have been successfully won due to incomplete or inaccurate medical records containing insufficient detail to defend the case brought by the applicant.1
The Royal College of Surgeons of England (RCSE)2 produced guidelines on the information required to form a complete medical record. Scoring systems such as the CRABEL (Crawford, Beresford and Lafferty) system have been developed in order to assess the quality of record keeping.3 These allow quantitative comparison of notes.
Both the RCSE guidelines and the CRABEL score focus on the overall quality of the content of medical records, but do not take the legibility of notes into account. We, therefore, developed a new scoring system – the Adjusted Note Keeping and Legibility (ANKLe) score. This provides a universal, objective and quantitative assessment tool of the overall quality of medical notes, taking into account both content and legibility. The authors report on its use in a completed audit loop of medical record keeping in the senior house officer (SHO)-led otolaryngology emergency clinic.
Patients and Methods
ANKLe score development
RCSE guidelines2 were adapted to produce a list of 18 pieces of information that would be expected to be documented in an initial clinic clerking, each of which scored one point. Two additional points were added, which were unique to the otolaryngology clinic (Table 1). A scoring system for legibility was also developed (Table 2). The ANKLe score combines both content (out of 20) and legibility (out of 4) to give an overall score out of 24. A satisfactory score is at least 20 (content score 17/20; legibility score 3/4). This equates to a legible set of notes with most of the required content recorded.
Table 1.
Content scoring system
| Generic content | |
| • | Name |
| • | Date of birth or hospital number |
| • | Consultant on call |
| • | Referral source |
| • | Date seen |
| • | Time seen |
| • | Presenting complaint |
| • | History of presenting complaint |
| • | Past medical history |
| • | Drug and allergy history |
| • | Family history |
| v | Social history |
| • | Examination |
| • | Working diagnosis |
| • | Plan of care |
| • | SHO name |
| • | SHO signature |
| • | SHO bleep |
| ENT specific content | |
| • | Attendance sheet of patient details |
| • | Consultation details inserted in ENT computer database |
Table 2.
Legibility scoring system
| Quality of handwriting | Score |
|---|---|
| Largely illegible | 1 |
| Legible with difficulty | 2 |
| Legible | 3 |
| Legible and neat | 4 |
Audit – first cycle
A prospective audit was undertaken of note keeping in our otolaryngology emergency clinic. The initial clerkings of 20 consecutive sets of notes from each of 7 doctors were evaluated for documentation of information and legibility using the ANKLe scoring system. A total of 140 sets of notes were audited against the standard of a content score of 17, a legibility score of 3 and an overall ANKLe score of 20. All notes were scored jointly by SCD and DH.
Intervention
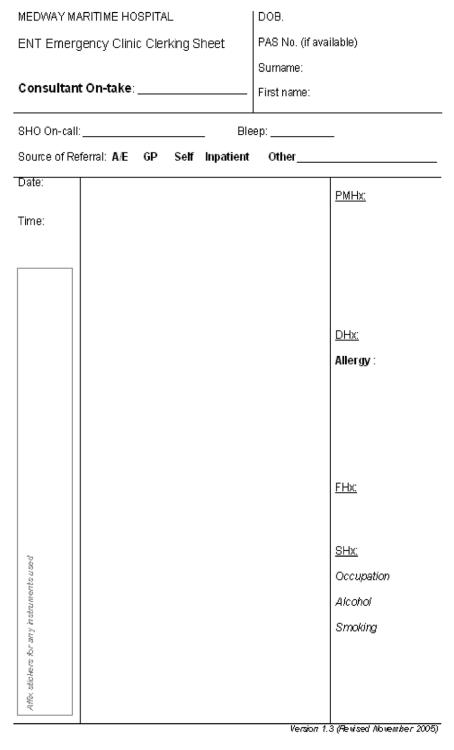
Following the first audit, a clerking proforma was introduced to encourage full documentation of information (Fig. 1). Those doctors with mean legibility scores below 3 were given advice on how to improve their handwriting. This advice included taking time to write slowly and clearly and encouraging the use of capital letters for important pieces of information such as medications.
Figure 1.
Clerking proforma.
Audit – Second Cycle
A re-audit was performed using the same method with a further 20 consecutive sets of notes from each of 7 doctors.
Statistical analysis
Mean scores achieved by notes and the levels of documentation of information were compared by the Wilcoxon signed rank test.
Results
First cycle
In the first cycle, 36% of notes achieved the standard for content, 68% for legibility and 36% for overall ANKLe score. Mean overall scores for content, legibility and ANKLe were 16.0, 2.96 and 18.95, respectively. Information that was poorly documented included patient date of birth (65% of notes), responsible consultant (22%), and time seen (66%).
Second cycle
Following the introduction of a clerking proforma and handwriting advice, all scores improved. Overall, 75% of notes achieved standards in legibility, 66% in content and 68% in overall ANKLe score. Mean overall scores for content, legibility and ANKLe score all showed significant improvement (Table 3).
Table 3.
Improvement in overall scores
| Standard achieved | Mean score First cycle | Mean score Second cycle | P-value |
|---|---|---|---|
| Contents | 16.0 | 17.2 | < 0.0001 |
| Legibility | 2.96 | 3.02 | < 0.05 |
| ANKLe | 18.95 | 20.24 | < 0.0001 |
The documentation of most information significantly improved in the second audit cycle (Table 4). All the areas where a significant improvement was found were those specifically required by the proforma. Those areas with no change or a significant worsening in documentation were those not specifically required by the proforma.
Table 4.
Documentation of information in first and second audit cycles
| Information | Number documented First cycle (/140) | Number documented Second cycle (/140) | Improvement | P-value |
|---|---|---|---|---|
| Consultant on call | 31 | 104 | +73 | < 0.0001 |
| Referral source | 95 | 133 | +38 | < 0.0001 |
| Social history | 55 | 88 | +33 | < 0.0001 |
| Time seen | 92 | 122 | +30 | < 0.0001 |
| Date of birth or hospital number | 91 | 120 | +29 | < 0.0001 |
| Family history | 8 | 37 | +29 | < 0.0001 |
| Drug and allergy history | 109 | 124 | +15 | < 0.0001 |
| Past medical history | 115 | 129 | +14 | < 0.0001 |
| Name | 137 | 138 | +1 | 0.32 |
| Date seen | 138 | 138 | 0 | – |
| Examination | 140 | 140 | 0 | – |
| Plan of care | 140 | 139 | −1 | 0.32 |
| History of presenting complaint | 140 | 138 | −2 | 0.16 |
| Presenting complaint | 140 | 138 | −2 | 0.16 |
| SHO signature | 140 | 138 | −2 | 0.16 |
| SHO name | 139 | 133 | −6 | 0.014 |
| Working diagnosis | 133 | 127 | −7 | 0.008 |
| Attendance sheet | 128 | 116 | −12 | 0.0005 |
| SHO bleep | 139 | 123 | −16 | 0.0001 |
| ENT database | 129 | 105 | −24 | < 0.0001 |
Discussion
The Medical Protection Society estimates that 12% of cases against general practitioners in the UK relate to inadequate note keeping.1 These cases can result in hundreds of thousands of pounds in compensation awards. The General Medical Council (GMC) states that it is every doctor's duty to ‘keep clear accurate, legible and contemporaneous patient records which report the relevant clinical findings’.4 Quality of records depends on their content but also on whether the information can be read. As an example, a case of poor handwriting in the US resulted in the dispensing of incorrect medication which led to the death of the patient. The doctor was ordered to pay $225,000 compensation.5
Initial audit of record keeping in the otolaryngology emergency clinic showed poor legibility and poor documentation in many areas. The authors introduced a proforma for the initial clinic clerking and gave advice on handwriting to doctors with poor legibility. The ANKLe scoring system was developed in order to provide an objective assessment tool of note quality.
Several studies in different areas of healthcare have found the introduction of proformas to be successful in aiding communication.6–9 Proformas often reduce the amount of handwriting needed to convey information through simplification and the use of tick-boxes and checklists. This aids thorough documentation and can reduce misinterpretation of information through illegible handwriting.
The proforma used in this study significantly improved the documentation of information in many areas, ensuring that a thorough clerking was taken. These findings were in agreement with previous studies. The proforma was widely accepted by both the doctors and nursing staff as useful and easy to use. It has continued to be used within the department, and has been promoted within the hospital as a means to improve documentation.
It is a commonly held belief that the handwriting of doctors is illegible. This is supported by studies that found doctors' handwriting to be significantly less legible than their fellow health-care professionals10 and often completely illegible.11 Doctors' notes are often written under the pressure of time, which results in poor legibility.12 Methods suggested to improve legibility include writing with a fountain pen13 and the use of self-inking rubber stamps,14 which clearly show the doctor's name and other details such as GMC number.
Doctors with poor handwriting are not routinely reminded about their standards of legibility. The authors could find no specific methods employed to improve handwriting in current practice. A significant improvement in the legibility of notes was demonstrated through the use of simple advice on handwriting to those with low scores. Although handwriting may become less important with the introduction of electronic medical records, it is likely that there will always be some hand-written documentation.
The ANKLe score provides a quantitative assessment of note quality, taking into account both content and legibility. It is scored out of 24, with 20 points allocated to content and 4 to legibility. Eighteen of the points for content are generic to all notes, with 2 that could be changed to make this scoring system adaptable to other specialties. For example, in paediatrics, points for a birth and developmental history could be used.
As the ANKLe score takes both content and legibility into account, it is difficult to achieve an acceptable score of 20 if legibility is poor. The authors believe that the ANKLe score is the first scoring system to take legibility and content into account when assessing note quality. It enables evaluation of both an individual practitioner's ability to keep good records as well as the overall standards of the healthcare team. This study has demonstrated that the ANKLe score can be used to assess and identify individuals whose note keeping is lacking in information content and/or legibility, enabling these individuals to be targeted for improvement. In the first cycle, only 36% of notes met the standard of an ANKLe score of 20/24. By improving note content through the introduction of the proforma and legibility by giving guidance on handwriting, the ANKLe standard was met in 68% of notes in the second cycle.
Conclusions
Good medical records rely both on adequate content and legibility. The ANKLe scoring tool can be used to assess the quality of notes objectively as it takes both the content of notes and legibility into account. This study has demonstrated the use of the ANKLe score in assessing notes and identifying areas of poor documentation and doctors with poor handwriting. The successful introduction of a proforma resulted in a significant improvement in the documentation of information. Handwriting advice to doctors with poor note legibility led to a significant improvement in their performance. The ANKLe score can be adapted and these simple interventions applied to other specialties.
Acknowledgments
The authors thank Mr M Oyarzabal, Consultant Otolaryngologist at Medway Maritime Hospital, for his guidance in this audit.
References
- 1.Medical Protection Society. Casebook: Falling on Deaf Ears. 4. Vol. 12. London: MPS; 2004. p. 24. [Google Scholar]
- 2.The Royal College of Surgeons of England. Guidelines for Clinicians on Medical Records and Notes. London: RCSE; 1990. [PubMed] [Google Scholar]
- 3.Crawford JR, Beresford TP, Lafferty KL. The CRABEL score – a method for auditing medical records. Ann R Coll Surg Engl. 2001;83:65–8. [PMC free article] [PubMed] [Google Scholar]
- 4.General Medical Council. Good Medical Practice. London: GMC; 2001. [Google Scholar]
- 5.Charatan F. Family compensated for death after illegible prescription. BMJ. 1999;319:1456. doi: 10.1136/bmj.319.7223.1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Osborn GD, Pike H, Smith M, Winter R, Vaughan-Williams E. Quality of clinical case note entries: how good are we at achieving set standards? Ann R Coll Surg Engl. 2005;87:458–60. doi: 10.1308/003588405X60632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thompson AG, Jacob K, Fulton J, McGavin CR. Do post-take ward round proformas improve communication and influence quality of patient care? Postgrad Med J. 2004;80:675–6. doi: 10.1136/pgmj.2003.016097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hobson JC, Khemani S, Singh A. Prospective audit of quality of ENT emergency clinic notes before and after introduction of a computerized template. J Laryngol Otol. 2005;119:264–6. doi: 10.1258/0022215054020359. [DOI] [PubMed] [Google Scholar]
- 9.Hussainy HA, Ali F, Jones S, McGregor-Riley JC, Sukumar S. Improving the standard of operation notes in or thopaedic and trauma surgery: the value of a proforma. Injury. 2004;35:1102–6. doi: 10.1016/j.injury.2003.10.016. [DOI] [PubMed] [Google Scholar]
- 10.Lyons R, Payne C, McCabe M, Fielder C. Legibility of doctors' handwriting: quantitative comparative study. BMJ. 1998;317:863–4. doi: 10.1136/bmj.317.7162.863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rodriguez-Vera F, Marin Y, Sanchez A, Borrachero C, Pujol E. Illegible handwriting in medical records. J R Soc Med. 2002;95:545–6. doi: 10.1258/jrsm.95.11.545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Berwick D, Winickoff N. The truth about doctors' handwriting: a prospective study. BMJ. 1996;313:1657–8. doi: 10.1136/bmj.313.7072.1657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dunea G. Beastly handwriting. BMJ. 1999;319:65. doi: 10.1136/bmj.319.7201.65a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Medford ARL, France AJ. Pocket-size self-inking rubber stamps improve legibility of case notes. Qual Primary Care. 2004;12:147–9. [Google Scholar]