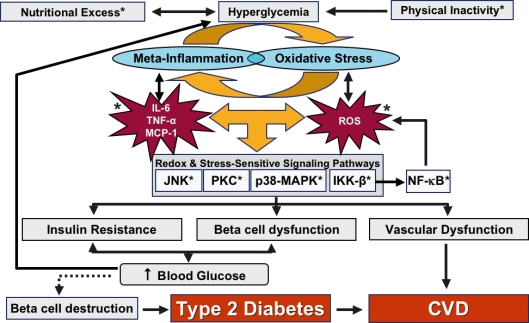
Figure 2.
Chronic hyperglycaemia, driven by nutritional excess and physical inactivity, greatly influences the positive feedback loop that drives mediators of meta-inflammation and oxidative stress, such as TNF-α, MCP-1, IL-6, and reactive oxygen species (ROS). These activate stress-sensitive signalling pathways, which include JNK, PKC, p38-MAPK and IKK-β. Activation of these pathways leads to insulin resistance and dysfunction of the β-cell dysfunction and vasculature. Insulin resistance and β-cell dysfunction cause an increase in blood glucose levels, which can create a vicious cycle leading to pathophysiology of target organs. If left unchecked, chronic hyperglycaemia eventually causes β-cell destruction (designated by the dotted line), leading to the development of type 2 diabetes and cardiovascular disease (CVD). Potential areas for therapeutic intervention (designated by *) may modulate the mediators of the oxidation-inflammation cascade to improve glucose tolerance, β-cell dysfunction and vascular function, thereby slowing the development of type 2 diabetes. TNF-α, tissue necrosis factor-α; IL-6, interleukin-6; MCP-1, monocyte chemoattractant factor-1; JNK, c-Jun N-terminal kinase; PKC, protein kinase C; MAPK, mitogen-activated protein kinase; IKK-β, inhibitor of kappa β kinase