Abstract
Background
Chest pain is one of the most common causes of presentation to the emergency room. The diagnosis of non-ST-elevation acute coronary syndrome typically causes uncertainty. Classical considerations for risk stratification are History, ECG, Age, Risk factors and Troponin (HEART). Each can be scored with zero, one or two points, depending on the extent of the abnormality. The HEART score is the sum of these five considerations. Methods. Clinical data from 122 patients referred to the emergency room for chest pain were analysed. The predictive value of the HEART score for reaching an endpoint was evaluated in 120/122 patients.
Results
Twenty-nine patients reached one or more endpoints: an acute myocardial infarction was diagnosed in 16 patients, 20 underwent revascularisation and two died. The HEART score in the patients with and without an endpoint was 6.51±1.84 and 3.71±1.83 (p<0.0001) respectively. A HEART score of 0-3 points holds a risk of 2.5% for an endpoint and supports an immediate discharge. With a risk of 20.3%, a HEART score of 4-6 points implies admission for clinical observation. A HEART score ≥7points, with a risk of 72.7%, supports early invasive strategies.
Conclusion
The HEART score facilitates accurate diagnostic and therapeutic choices. The HEART score is an easy, quick and reliable predictor of outcome in chest pain patients. (Neth Heart J 2008;16:191-6.)
Keywords: chest pain, acute coronary syndrome, emergency room
Chest pain is one of the most common reasons for admitting patients to the emergency room. An acute coronary syndrome (ACS) needs to be distinguished from a variety of other cardiac and noncardiac diseases that cause chest pain. In certain cases, a diagnosis can be made quickly, in particular in the case of an acute transmural myocardial infarction.
Non-ST-elevation ACS (nSTE-ACS), previously called ‘unstable angina’ or ‘pending infarction’, typically causes uncertainty.1 This diagnosis can be made quickly in case of concurrent typical changes in the electrocardiogram (ECG) and/or increased levels of myocardial markers in plasma. Absence of such abnormalities, however, does not always exclude an nSTE-ACS. Therefore, excluding the diagnosis of nSTE-ACS is felt to be hard in the early stages of the diagnostic process. It is important to make a quick diagnosis as patients benefit significantly from early treatment.2 In addition, a ‘missed diagnosis’ may result in a wrongful discharge and ultimately in out-ofhospital sudden death when unstable angina becomes a myocardial infarction.
Typically, patients are checked by a resident on duty in the emergency room and subsequently discussed with a supervisor. Based on a general impression, patient history, risk factors, ECG and levels of myocardial infarction markers it is decided whether or not to admit the patient for clinical observation. Typically, all patients under suspicion of the diagnosis of nSTE-ACS are treated as such, awaiting confirmation or exclusion of the diagnosis.
Most data on the risk stratification of nSTE-ACS have been retrieved from clinical drug trials. In these trials, patients were selected with chest pain plus some objective confirmation of the diagnosis. In order to obtain good trial results, low-risk cases were excluded. Therefore, little is known about the natural course of such doubtful cases.3 How often do we miss the diagnosis of nSTE-ACS in patients with nonspecific chest pain, resulting in a seriously adverse outcome?
As a first step in developing a method for risk stratification, all patients admitted to the emergency room for chest pain during a three-month period were analysed in order to answer two questions: what made doctors decide to admit patients to the coronary care unit or not, and which were the predictors of acute myocardial infarction, need for revascularisation and death.
Methods
This study was performed at a 265-bed community hospital. Inclusion criteria for this study were any patient admitted to the emergency room due to chest pain irrespective of age, prehospital assumptions and previous medical treatments. One very relevant population with chest pain that never arrived at the emergency room needs to be mentioned. Patients with chest pain and significant ST-segment elevation on the ECG during transportation in the ambulance were immediately taken to the coronary intervention room in another hospital nearby. Therefore, patients with ST-elevation acute myocardial infarction (STEMI) were not part of the study.
All admission and follow-up data were retrieved from the hospital charts. If follow-up data were lacking, patients were called at home to check their condition.
Expected predictors
Based on clinical experience and current medical literature, we expected specific patient history, ECG abnormalities, higher age, multiple risk factors for coronary artery disease and elevated troponin levels to be predictors of primary endpoints.
Scoring of predictors
History
For the purpose of this study, patient history was classified by two investigators, based on the narrative in the hospital charts written in the emergency room and not allowing for risk factors, ECGs, laboratory results and later developments. In the absence of specific elements in terms of pattern of the chest pain, onset and duration, relation with exercise, stress or cold, localisation, concomitant symptoms and the reaction to sublingual nitrates, the history was classified as ‘nonspecific’ and granted zero points. If the patient history contained both nonspecific and suspicious elements, the history was classified as ‘moderately suspicious’ and granted one point. If the history contained primarily specific elements, the history was classified highly suspicious and granted two points.
ECG
The ECG taken in the emergency room was reviewed and classified. If the ECG was ‘normal’ according to Minnesota criteria,4 zero points were given. In case of repolarisation abnormalities without significant STsegment depression, one point was given. One point was also granted for bundle branch block, typical abnormalities indicative of left ventricular hypertrophy, repolarisation abnormalities probably due to the use of digoxin or in case of unchanged known repolarisation disturbances. For significant ST-segment depressions or elevations in the absence of a bundle branch block, left ventricular hypertrophy or the use of digoxin two points were given.
Age
For age at the time of admission zero points were given if the patient were younger than 45 years, one point if the patient was between 45 and 65 years and two points if the patient was 65 years or older.
Risk factors
The number of risk factors for coronary artery disease present in the individual were counted. The following risk factors were taken into account: currently treated diabetes mellitus, current or recent (<one month) smoker, diagnosed hypertension, diagnosed hypercholesterolaemia, family history of coronary artery disease and obesity. If the patient had no risk factors at all, zero points were given. For one or two risk factors, one point was given. For three or more risk factors, two points were given. Two points were also given for a history of coronary revascularisation, myocardial infarction, stroke or peripheral arterial disease.
Troponin I
Troponin I levels were measured as Access AccuTroponin I assay. If the troponin I level on admission was below the threshold value for positivity (troponin I ≤0.04) zero points were given. If the level was between once and twice the threshold value for positivity, one point was given. If the level was higher than twice the threshold value for positivity, two points were given.
Heart
The total number of points for History, ECG, Age, Risk factors and Troponin was noted as the HEART score. A grid for the score is given in table 1.
Table 1.
Composition of the HEART score for chest pain patients in the emergency room.
| HEART score for chest pain patients | Score | |
|---|---|---|
| History | Highly suspicious | 2 |
| Moderately suspicious | 1 | |
| Slightly suspicious | 0 | |
| ECG | Significant ST depression | 2 |
| Nonspecific repolarisation disturbance | 1 | |
| Normal | 0 | |
| Age | ≤65 year | 2 |
| 45-65 year | 1 | |
| <45 year | 0 | |
| Risk factors | ≥3 risk factors or history of atherosclerotic disease | 2 |
| 1 or 2 risk factors | 1 | |
| No risk factors known | 0 | |
| Troponin | >2x normal limit | 2 |
| 1-2x normal limit | 1 | |
| ≤normal limit | 0 | |
| Total |
Endpoints
Endpoints in this study were acute myocardial infarction (AMI), percutaneous coronary intervention (PCI), coronary artery bypass graft (CABG) and death plus a combined endpoint of AMI, PCI, CABG and death.
Statistics
Statistical analysis was performed according to the SAS system (SAS inc, Cary, NC). Descriptive statistics were given as average ± SD, percentage or Kaplan-Meier cumulative event-free curve. Differences between groups were assessed by means of the Student’s t-test when normally distributed, for count data we used the Fisher’s exact test or in case of ordinal data the Cochran-Armitage trend test. The probability of reaching an endpoint was calculated as the percentage of cases with an endpoint within a category. Statistical significance was defined as p<0.05 two-sided.
Results
During the study period, from 1 January to 31 March 2006, a total of 122 chest pain patients were admitted to the emergency room. Patients were 61.2±15.4 years of age. The male/female distribution was 73/49. Race was not routinely noted in the patient charts; in the geographical area of the hospital the vast majority (>95%) of the population were white/Caucasian.
Follow-up
In 120/122 patients (98.3%) long-term follow-up data are available, with a duration of 423±106 days. In two cases follow-up is lacking. These were foreign visitors, one a 42-year-old female from Poland (patient # 47) and one a 30-year-old male from South Africa (patient # 119). Both suffered from nonspecific chest pain and had no abnormalities in their ECG or troponin levels. The HEART scores for these patients were 1 and 0 respectively. Neither were hospitalised. They appear to have returned to their home countries without leaving any traces. Their data are not part of the study’s group comparisons.
Endpoints reached
A total of 29 patients (24.1%) reached one or more endpoints. An AMI was diagnosed in 16 patients (13.3%), 14 patients (11.6%) underwent percutaneous coronary intervention (PCI), six (5.0%) had coronary artery bypass graft (CABG) surgery and two (1.6%) died. All endpoints occurred within a time frame of three months.
Myocardial infarction
An AMI was diagnosed in 16 of the 120 patients (13.3%). Fourteen of these patients (87.5%) already had elevated myocardial markers on admission (apparently these AMIs had started before their arrival to the emergency room.) One AMI occurred two days after admission despite medical treatment in a 64-yearold male (# 89). One AMI occurred ten days afterwards in a discharged patient (# 25). This patient is still alive.
Revascularisation
Coronary angiography was performed in 27 of the 120 patients (22.5%). Revascularisation was performed in 20 patients (16.6%): 14 PCIs (11.6%) and six CABGs (5.0%). Of the 77 patients who were hospitalised, 12 (15.5%) had a PCI and six (7.7%) a CABG. In the 43 discharged patients revascularisation was performed in two cases (4.6%). Both were successful single-vessle PCIs, without any complications. This concerns # 25 and # 45.
Mortality
Two patients died from the entire study population (1.6%), and death occurred exclusively in the admitted patient group. Both patients were 78-year-old males. One patient died 14 days after admission and the other after 11 days. Both had a HEART score of 8.
Time frame of endpoints
The graph for survival free of acute myocardial infarction and revascularisation is given in figure 1. All endpoints occurred within a time frame of three months.
Figure 1.
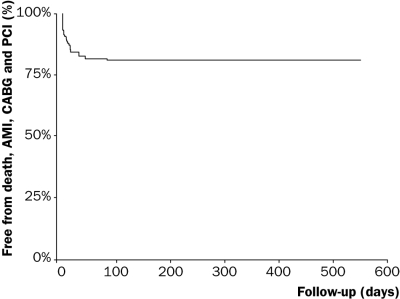
Acute myocardial infarction, PCI and CABG free survival.
Risk factors for reaching an endpoint
A comparison of the risk profile was made between the patient groups with and without an endpoint. Results are presented in table 2. Of these variables, a history of hypertension, positive family history and history of peripheral arterial disease were independent predictors of the combined endpoint.
Table 2.
Risk profile of patients with and without the combined endpoint of AMI, revascularisation or death.
| Variable | Endpoint | Endpoint | Total | P value |
|---|---|---|---|---|
| No | Yes | |||
| N | 91 | 29 | 120 | |
| Age | 60.5±15.7 | 64.7±13.2 | 61.2±15.4 | 0.1783 |
| Male gender | 50 (54.9%) | 22 (75.8%) | 72 (60.0%) | 0.0522 |
| Diabetes mellitus | 17 (18.6%) | 5 (17.2%) | 22 (18.3%) | 1.0000 |
| Current smoker | 26 (28.5%) | 10 (34.4%) | 36 (30.0%) | 0.6425 |
| Hypercholesterolaemia | 40 (43.9%) | 12 (41.3%) | 52 (43.3%) | 0.8332 |
| Hypertension | 29 (31.8%) | 18 (62.7%) | 47 (39.1%) | 0.0048 |
| Family history of coronary artery disease | 27 (29.6%) | 15 (51.%) | 42 (35.0%) | 0.0435 |
| Reported obesity | 14 (15.3%) | 5 (17.2%) | 19 (15.8%) | 0.7768 |
| History of myocardial infarction | 13 (14.2%) | 5 (17.2%) | 18 (15.0%) | 0.6979 |
| History of CABG | 3 (3.3%) | 0 (0.0%) | 3 (2.5%) | 1.0000 |
| History of PCI | 9 (9.8%) | 1 (3.4%) | 10 (8.3%) | 0.4479 |
| History of stroke | 7 (7.6%) | 5 (17.2%) | 12 (10.0%) | 0.1592 |
| History of peripheral arterial disease | 1 (1.1%) | 3 (10.3%) | 4 (3.3%) | 0.0434 |
| Use of aspirin | 28 (30.7%) | 10 (34.4%) | 38 (31.6%) | 0.7081 |
| Use of statins | 31 (34.0%) | 10 (34.4%) | 41 (34.1%) | 1.0000 |
The relation between the five predefined elements of the HEART score for chest pain patients and the occurrence of endpoints is given in table 3. Patient history, ECG abnormalities and elevated troponin values were independent predictors of the combined endpoint. The average HEART score in the no endpoint group was 3.71±1.83 and in the patients with at least one endpoint 6.51±1.84 (p<0.0001).
Table 3.
Numbers of patients in each element of the HEART score in groups with or without endpoints.
| No endpoint reached | One or more endpoints reached | P value | |||||
|---|---|---|---|---|---|---|---|
| n=91 | n=29 | ||||||
| Points | 0 | 1 | 2 | 0 | 1 | 2 | |
| History | 44 | 37 | 10 | 5 | 10 | 14 | <0.0001 |
| ECG | 60 | 23 | 8 | 8 | 4 | 17 | <0.0001 |
| Age | 13 | 36 | 42 | 4 | 7 | 18 | 0.2847 |
| Risk factors | 15 | 44 | 32 | 3 | 9 | 17 | 0.0827 |
| Troponin | 82 | 4 | 5 | 15 | 1 | 13 | <0.0001 |
| HEART score (average ± SD) | 3.71±1.83 | 6.51±1.84 | <0.0001 |
Distribution
The distribution of HEART scores in patients with or without the combined endpoint of AMI, revascularisation or death is given in figure 2. The HEART score follows Gaussian distribution in both groups.
Figure 2.
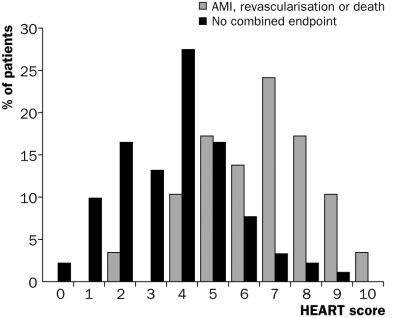
Percentages of patients in each HEART score in groups with and without the combined endpoint of AMI, revascularisation or death.
The HEART score yields all crucial information that can correctly place patients into low-, intermediateand high-risk groups for clinically important irreversible adverse cardiac events: myocardial infarction, revascularisation and cardiac death. One of the 39 patients (2.5%) with a HEART score of 0-3 points had an endpoint. This was a patient who required a CABG 11 days after admission. In the 59 patients with a HEART score of 4-6 points, 12 (20.3%) had an endpoint. In case of a HEART score of 7-10 points, 16 of 22 (72.7%) reached the combined endpoint. In addition, figure 3 illustrates an almost linear relation between the HEART score and the chance of reaching an endpoint (p for trend <0.001).
Figure 3.
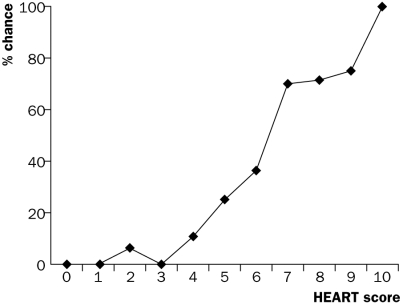
Chances of reaching the combined endpoint in each HEART category.
Discussion
Definition of ACS
Chest pain patients in the emergency ward create uncertainty for all treating physicians, in particular when no diagnosis is made. The diagnosis of nSTE-ACS may be easy to confirm but is often hard to exclude.5 Corroboration of this article may be found in the inclusion criteria for the major treatment trials in ACS, where patients were randomised only when the diagnosis was confirmed by means of typical ECG changes and/or elevated troponin levels. Unconfirmed cases of ACS were ignored in such trials. Although the landmark drug trials have provided a wealth of data on the natural course of high risk nSTE-ACS and have proven the (lack of) efficacy of various treatments, the optimal approach for patients with borderline evidence of an nSTE-ACS is largely unknown. This is also reflected in the current American and European guidelines.6,7
HEART score
Challenged by the lack of exact definitions or criteria for nSTE-ACS, we attempted to define an easy-to-use policy for clinicians. The starting-point question was: which are the decisive factors in practice? They are History, ECG, Age, Risk factors and Troponin. Similar to the Apgar score,8 globally used to assess the need for intensive care in newborns, these five factors can be fused together. Each of the five factors can be appreciated with 0, 1 or 2 points. The sum of all five is called the HEART risk score for chest pain patients. Definitions were based on literature as much as possible. Continuous variables such as age and troponin are exactly defined. Unfortunately, definitions for patient history are lacking in the literature. Therefore, patient history is subject to personal interpretations. Our experience is that the HEART score for individual patients can be calculated without a calculator and even without a sheet of paper.
Literature
In the literature, several risk scores for nSTE-ACS have been published. The most reputed are the TIMI,9 PURSUIT10 and GRACE11,12 risk scores, which were compared by De Araújo Gonçalves.13 Despite the firm scientific basis for all three scoring systems and the recommendations in guidelines, none is widely applied in clinical practice. These classical scoring systems do not show much interest in the differentiation of chest pain patients who are at low to moderate risk for an adverse outcome. The TIMI and PURSUIT scores were designed to identify high-risk patients, who are most likely to benefit from aggressive therapy. The major disadvantage of the GRACE score is that it can only be calculated with the use of the internet. The TIMI score is simple to calculate, but it is quite rough as it allows only binary choices, thus ignoring the fact that many variables have a ‘grey area’. The PURSUIT score is outdated as it was designed before the introduction of troponin assays for clinical use.
Advantages
A major advantage of the HEART score is that it facilitates communication between doctors. A single figure summarises at least ten lines of descriptions and considerations about chest pain patients. For example, when the resident calls the supervisor to discuss the use of limited resources for two chest pain patients, one with eight points and another with two points, choices may appear clear.
Guidelines could be easily and briefly formulated when based on the HEART score. A score of 0-3 points holds a risk of 2.5% of reaching an endpoint and therefore supports a policy of early discharge. With this very low risk percentage in mind, it is doubtful whether additional diagnostic procedures at the outpatient clinic will be useful. With a HEART score of 4-6 points, immediate discharge is not an option as this figure indicates a risk of 20.3% for an adverse outcome. These patients should be admitted for clinical observation, treated as an ACS awaiting final diagnosis and subjected to noninvasive investigations, such as repeated troponin, exercise testing and possibly advanced ischaemia detection. A HEART score ≥7 points, with a risk of 72.7%, implies early aggressive treatment including invasive strategies without preceding noninvasive testing. Clearly, cut-off points may need to be validated in larger multicentre studies.
Limitations
Our study is a careful scientific analysis of a clinical view. Some people believe that only prospective, randomised studies hold true. Our study was set up as a pilot study and was observational and retrospective for the simple reason that this is the optimal design to answer the questions of the study, without the otherwise unavoidable risk of influencing the outcome by the experimental setting. However, we believe that the unexpected significance of the study provides a firm basis for further investigation.
Conclusions
The HEART score helps the cardiologist in making accurate diagnostic and therapeutic choices in a setting that is currently denoted by uncertainty and a lack of guidance by the medical literature. The HEART score is an easy, quick and reliable predictor of outcome in chest pain patients and can therefore be used for triage.
References
- 1.Cannon CP, Braunwald E. Unstable angina and non-ST elevation myocardial infarction. In Zipes, Libby, Bonow and Braunwald (eds.): Braunwald’s Heart Disease. A textbook of cardiovascular medicine. Elsevier Saunders 2005. pp 1243-79. [Google Scholar]
- 2.Hirsch A, Windhausen F, Thijssen JGP, Verheugt FWA, Cornel JH, De Winter RJ. Long-term outcome after an early invasive versus selective invasive treatment strategy in patients with non-ST-elevation acute coronary syndrome and elevated cardiac troponin T (the ICTUS trial): a follow-up study. Lancet 2007;369:827-35. [DOI] [PubMed] [Google Scholar]
- 3.Miller CD, Lindsell CJ, Khandelwal S, et al. Is the initial diagnostic impression of “Noncardiac Chest Pain” adequate to exclude cardiac disease? Ann Emerg Med 2004;44:565-74. [DOI] [PubMed] [Google Scholar]
- 4.Blackburn H, Keys A, Simonson E, et. The electrocardiogram in population studies: a classification system. Circulation 1960;21:1160-75. [DOI] [PubMed] [Google Scholar]
- 5.Hollander JE. Acute coronary syndrome in the emergency department: Diagnosis, risk stratification, and management. In: P Théroux (Ed.): Acute coronary syndromes. A companion to Braunwald’s heart disease. Saunders/Elsevier, 2003. [Google Scholar]
- 6.ACC/AHA 2007 Guidelines for the Management of Patients With Unstable Angina/Non–ST-Elevation Myocardial Infarction. J Am Coll Cardiol 2007;50:e1-157. [DOI] [PubMed] [Google Scholar]
- 7.Bassand JP, Hamm CW, Ardessino D, et al. Guidelines for the diagnosis and treatment of non ST-segment elevation Acute Coronary Syndromes. Eur Heart J 2007;28:1598-660. [DOI] [PubMed] [Google Scholar]
- 8.Apgar V. A Proposal for a New Method of Evaluation of the Newborn Infant. Current Researches in Anesthesia and Analgesia, July-August, 1953, page 260. [PubMed] [Google Scholar]
- 9.Antman EM, Cohen Mk Bernink PJLM, et al. The TIMI risk score for unstable angina/ non-ST elevation MI. JAMA 2000; 284:835-42. [DOI] [PubMed] [Google Scholar]
- 10.Boersma E, Pieper KS, Steyerberg EW, et al. for the PURSUIT investigators. Predictors of outcome in patients with acute coronary syndromes without persistent ST-segment elevation. Results from an international trial of 9461 patients. Circulation 2000;101:2557-67. [DOI] [PubMed] [Google Scholar]
- 11.Granger CB, Goldberg RJ, Dabbous OH, et al. for the Global Registry of Acute Coronary Events Investigators. Predictors of hospital mortality in the global registry of acute coronary events. Arch Intern Med 2003;163:2345-53. [DOI] [PubMed] [Google Scholar]
- 12.Fox KA, Dabbous OH, Goldberg RJ, et al. Prediction of risk of death and myocardial infarction in the six months after presentation with acute coronary syndrome: prospective multinational observational study (GRACE). BMJ 2006;333:1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.De Araújo Gonçalves P, Ferreira J, Aguiar C, Seabra-Gomes R. TIMI, PURSUIT, and GRACE risk scores: sustained prognostic value and interaction with revascularization in NSTE-ACS. Eur Heart J 2005;26:865-72. [DOI] [PubMed] [Google Scholar]


