Abstract
Objectives. We sought to assess the impact of several tobacco control policies and televised antismoking advertising on adult smoking prevalence.
Methods. We used a population survey in which smoking prevalence was measured each month from 1995 through 2006. Time-series analysis assessed the effect on smoking prevalence of televised antismoking advertising (with gross audience rating points [GRPs] per month), cigarette costliness, monthly sales of nicotine replacement therapy (NRT) and bupropion, and smoke-free restaurant laws.
Results. Increases in cigarette costliness and exposure to tobacco control media campaigns significantly reduced smoking prevalence. We found a 0.3-percentage-point reduction in smoking prevalence by either exposing the population to televised antismoking ads an average of almost 4 times per month (390 GRPs) or by increasing the costliness of a pack of cigarettes by 0.03% of gross average weekly earnings. Monthly sales of NRT and bupropion, exposure to NRT advertising, and smoke-free restaurant laws had no detectable impact on smoking prevalence.
Conclusions. Increases in the real price of cigarettes and tobacco control mass media campaigns broadcast at sufficient exposure levels and at regular intervals are critical for reducing population smoking prevalence.
Population-wide interventions that can reduce adult smoking prevalence are important for curbing the pandemic of tobacco-related disease.1–3 However, evaluating the effects of tobacco control policies and mass media interventions on populations is difficult.4,5 Generally, there are few comparable control populations to which policy or media interventions are not delivered. Tobacco policies and media campaigns often co-occur, complicating assessment of the relative contribution of each. In addition, most studies in which smoking prevalence is the outcome measure rely on annual population surveys to track change over time, despite policy and media interventions being generally implemented throughout the year, and at differing strengths relative to the time of survey administration. Small or transient impacts on smoking prevalence are difficult to detect and may be underestimated.
Over the past decade, the Australian population has been exposed to changes in several tobacco control policies, including changes in taxes on tobacco products resulting in increases in the real price of cigarettes, increasing availability of pharmaceutical smoking cessation products such as nicotine replacement therapies (NRT) and bupropion, and the introduction of smoke-free restaurant laws. In addition, there has been considerable variation in exposure to public health–sponsored mass media campaigns and pharmaceutical advertising for NRT. We have assessed the independent effect of each tobacco control policy and type of media campaign with a data series in which self-reported smoking prevalence was measured every month over a period of 11 years. This method has the advantage over annual population surveys of more closely matching the timing and extent of policy implementation and media exposure to smoking prevalence, and it has the ability to examine the pattern of change in prevalence, such as the lag time to a measurable impact and the duration of influence.
METHODS
Design
We merged monthly estimates of population exposure to antitobacco television advertising and changes in 3 tobacco control policies to serial cross-sectional monthly surveys of smoking prevalence to examine factors that influenced smoking prevalence.
Population Survey Data
Smoking prevalence from June 1995 to December 2006 was estimated from a Roy Morgan Research (Melbourne, Australia) weekly omnibus survey6 with a consistent methodology of a random sample of Australian residents 14 years or older. Federal electorate districts of approximately equal population served as the strata for sampling. Each electoral area was divided into 4 sampling points of roughly equal population size, which were used in rotation, 1 per week, with starting addresses selected at random from the electoral roll. (In Australia, the voting age is 18 years and enrollment on the electoral roll is compulsory for those who are eligible.) All 148 electorate districts were used in each weekly wave of interviews. One person per household was interviewed; interviewers were instructed to ask to speak to the youngest male 14 years or older and, if unavailable, to then ask to speak to the youngest female 14 years or older. The survey sample was weighted according to Australian Bureau of Statistics quarterly population estimates between June 1995 and June 1998, and for monthly population estimates from July 1998 to December 2006. Refusal rates varied over time, with a trend for higher refusal rates in more recent years.
We used survey data from the 5 largest Australian capital cities (Adelaide, Brisbane, Melbourne, Perth, and Sydney), where 61% of the adult population resides.7 These regions corresponded with the 5 media markets for which data on antitobacco advertising exposure were available. We cumulated weekly data to yield monthly estimates of smoking prevalence for respondents 18 years and older. Overall, there were 343 835 completed interviews and an average of 2474 participants each month in the survey (minimum = 1697, maximum = 3310).
We defined smokers as those who responded “yes” to the question, “Do you now smoke factory-made cigarettes?” or “yes” to the question, “In the last month, have you smoked any roll-your-own cigarettes (of tobacco)?” Smoking prevalence for any given month was the proportion of people who responded affirmatively to either of these questions out of all respondents surveyed in that month. Information was collected on month and year of interview and geographic location of respondent so that survey data could be matched to records of changes in policy and advertising.
Advertising Data
Occurrences of all tobacco-related advertisements appearing on television for the Adelaide, Brisbane, Melbourne, Perth, and Sydney media markets from June 1995 to December 2006 were acquired from OzTAM Pty Ltd (North Sydney, Australia)8 and Nielsen Media Research Australia (Sydney).9 Estimates of advertising exposure were assessed with television-monitoring devices and self-completion viewing diaries.10 Advertising exposure data are based on individual ratings of television programs obtained by monitoring household audiences across media markets. Ratings provide an estimate of the percentage of households with televisions watching a program or advertisement in a media market over a specified period. The advertising exposure measure is based on gross ratings points (GRPs) per month for the population aged 18 years and older. We equated 100 GRPs with an average of 1 potential advertisement exposure per month for all adults within a media market. GRPs represent average potential exposure; actual exposure for any given individual would vary on the basis of the frequency of actual television viewing and attention to the advertisements. GRPs were acquired for the 2 sole sources of tobacco television advertising in Australia: tobacco control advertising from state and national governments or other public health organizations, and direct-to-consumer advertising of NRT by pharmaceutical companies.
In Australia, tobacco control mass media campaigns have generally been funded through state or federal governments. Before 1997, state level–funded tobacco control programs broadcast most tobacco control advertising. From 1997 to 2001, the bulk of advertising exposure was accounted for by Australia’s National Tobacco Campaign, a collaborative federal and state government initiative, which featured 6 confronting television advertisements aimed at 18- to 40-year-olds with the message “every cigarette is doing you damage” along with an advertisement encouraging smokers to call the national telephone quit line service.11 (These advertisements can be viewed at http://www.quitnow.info.au under “Smokescreen.”)
Since 2002, most advertising has been broadcast by state-level tobacco control programs and mainly included messages for adults depicting the serious health consequences of smoking through graphic images, the use of personal stories, or simulated demonstrations of health effects. (A representative sample of these advertisements is available at http://www.quit.org.au/browse.asp?ContainerID=1640.) Only a small amount of state-level advertising featured the health effects of secondhand smoke or were aimed at youths by suggesting that smoking is not “cool.” Advertising GRPs from pharmaceutical companies for NRT, which commenced in September 1997, were also aggregated. There has been no television advertising for bupropion.
As GRPs are captured at the state level, both tobacco control and NRT advertising GRPs were modified to enable analysis at the national level. We therefore weighted the GRPs according to the percentage of the population living in each state in each year (e.g., 30% of the population lived in Victoria in 1995, so monthly GRPs in Victoria for this year were rescaled by a factor of 0.30).
Tobacco Control Policies
Tobacco prices.
Cigarette costliness was measured with the ratio of the average recommended retail price per cigarette pack to the average weekly earnings in the same quarter. Costliness is the percentage of weekly income that a typical packet of cigarettes costs. Cigarette price data were acquired from the bimonthly retail trade magazine Australian Retail Tobacconist (volumes 55–66), which gave the recommended retail price for packs of all brands in each state and territory. A comprehensive study of prices in Australia between 1997 and 200112,13 indicated that actual prices of cigarettes sold were close to recommended prices in convenience stores and petrol stations, but significantly lower than recommended prices in tobacco shops and supermarkets. Over the 4-year period during which prices were monitored, the average actual price of cigarettes sold across all outlets was significantly lower than the recommended prices, but the extent to which it was lower remained constant over the course of the study. We averaged the price of the 2 top-selling Australian brands (Peter Jackson 30s and Winfield 25s) for each state over the period. Sales of these 2 brands combined composed around 32% of total sales in 1994, increasing to more than 38% in 2003.14 We obtained quarterly estimates of employee gross average weekly earnings in each state, projected to the total population.15 Both price and income data were matched at the state level and then averaged to produce national estimates.
Population use of pharmaceutical smoking cessation products.
Throughout the study period, NRT was available, changing from prescription-only to over-the-counter status in September 1997. Generic patches were available starting in June 2001, and generic gum in September 2001. Supermarkets and convenience stores have sold NRT since June 2006, but pharmaceutical companies cannot advertise this availability. Bupropion was first made available by prescription in November 2000, with the government subsidizing the consumer starting in February 2001. Subsidized bupropion is restricted to 1 prescription of 90 tablets per year per adult. Because bupropion is a prescription-only drug, direct-to-consumer advertising for the drug is not permitted, but there was considerable unpaid news media coverage about its cost subsidization and later its association with sudden death that led to rapid uptake and then decline of the product in 2001.16,17 Generic versions of bupropion have been available since March 2006. We obtained monthly data on Australia-wide sales of NRT and bupropion from June 1995 to December 2006 from IMS Health Australia Pty Ltd (Crows Nest, Australia), a pharmaceutical sales tracking company.18 Monthly sales are expressed as 2 separate series, Australian dollar sales (consumer price index adjusted to 2006 dollars) and number of units sold. These data represent sales into pharmacies through wholesale channels, estimated to represent coverage of more than 98% of the market. The remaining 2% of sales were estimated with records of direct sales from a representative sample of pharmacies.
Smoke-free restaurant laws.
Smoke-free restaurant laws were implemented in January 1999 in Adelaide, June 2002 in Brisbane, July 2001 in Melbourne, April 1999 in Perth, and September 2000 in Sydney. To analyze state-level information at the national level, population exposure to smoke-free laws was expressed as the percentage of the total sample that was subject to such laws.
Statistical Analysis
We used time-series autoregressive integrated moving average analysis19,20 in SAS version 9.1 (SAS Institute Inc, Cary, NC) to estimate the effect of antitobacco advertising and tobacco policies on monthly smoking prevalence. Monthly smoking prevalence exhibited a downward trend. Because time-series modeling techniques require the removal of the effects of trend from the data, we used first-order differencing to transform the variable into a stationary series. As a first step in time-series analyses, it is necessary to establish that the outcome variable does not predict the explanatory variables of interest (i.e., feedback).20 We found no evidence that smoking prevalence predicted the occurrence of advertising or tobacco control policies. As a second step, it is necessary to identify the transfer function to establish the temporal nature of the relationships between the predictors and the outcome variable. To do this, preliminary modeling with the free-form distributed lag model with a single moving average term provided tentative specifications of the transfer functions. We then used autoregressive integrated moving average modeling to confirm these specifications at the bivariate level. Where this modeling did not identify transfer functions, we used results from similar variables to test a range of potential transfer functions to identify the best-fitting transfer function for each advertising and policy variable. Finally, we used autoregressive integrated moving average modeling to jointly examine the impact on smoking prevalence of the explanatory variables. Those variables that were least significant in the multivariate analysis were removed one at a time until a model remained with only significant explanatory variables, which satisfied the necessary assumptions for time-series analyses of stationarity, invertibility (i.e., error estimates were less than 1), and residuals resembling white noise, as evidenced by a nonsignificant Box-Ljung Q-test over 24 months and by nonsignificant correlations on the residual autocorrelation function.
RESULTS
Sample Characteristics
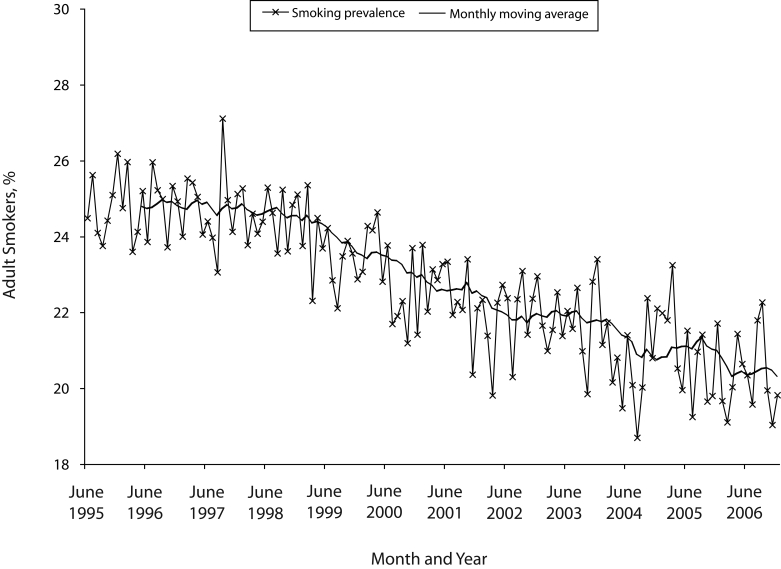
Monthly Australian smoking prevalence from June 1995 to December 2006 was characterized by an overall decline (Figure 1 ▶). The mean smoking prevalence during the period was 22.9% (SD= 1.9%), with a minimum of 18.7% (August 2004) and a maximum of 27.1% (September 1997).
FIGURE 1—
Monthly adult smoking prevalence: Australia, June 1995 to December 2006.
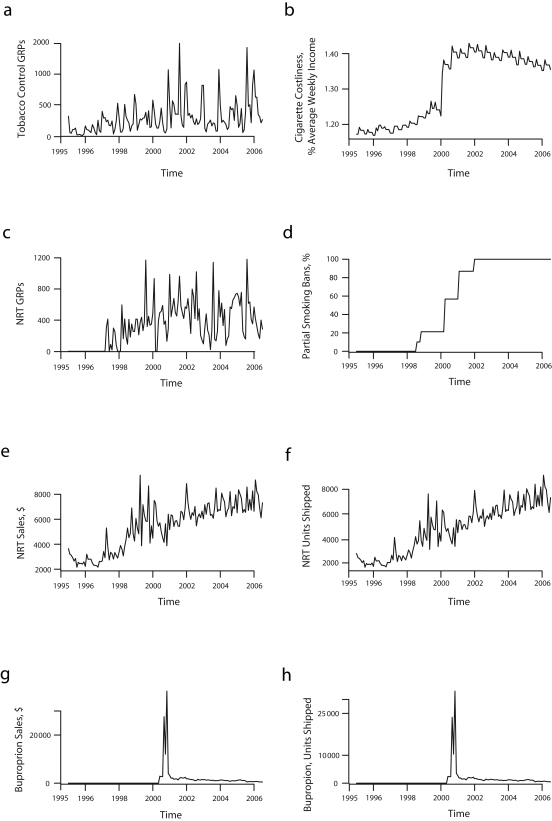
Table 1 ▶ and Figure 2 ▶ show that tobacco control advertising had an average monthly exposure of 288.51 GRPs per month, and NRT advertising averaged 331.85 GRPs per month, although both showed wide variability. Over the study period, cigarettes became more costly. In June 1995, a pack of cigarettes cost 1.17% of gross average weekly earnings. This increased steadily until July 2000, when the method of taxing tobacco changed and a goods and services tax was implemented,13 leading to a pack costing 1.34% of weekly earnings. Cigarette costliness reached a peak of 1.42% of weekly earnings in February 2002 and then declined, with a pack costing 1.36% of gross average weekly earnings in December 2006. As smoke-free restaurant laws rolled out across the nation, 10.1% of the sample was subject to them as of January 1999 (Adelaide), 100% as of June 2002 (Brisbane), 87.0% as of July 2001 (Melbourne), 21.3% as of April 1999 (Perth), and 56.8% as of September 2000 (Sydney). Mean monthly sales of NRT were 203420 units, representing a wholesale cost of AU$5429920. For bupropion, mean monthly sales were 6770 units, generating mean monthly sales of AU$1264770, although there was a sharp peak following its release in 2001.
TABLE 1—
Tobacco Control Policies and Mass Media Campaign Exposure Each Month: Australia, June 1995 to December 2006
| Mean (SD) | Minimum (Month and Year) | Maximum (Month and Year) | |
| Tobacco control GRPs per month | 288.51 (267.18) | 0 (April 1996) | 1502.91 (January 2002) |
| NRT GRPs per month | 331.85 (286.98) | 0 (before September 1997) | 1181.59 (January 2006) |
| Cigarette costlinessa | 1.31 (0.10) | 1.17 (June–July 1996) | 1.42 (February 2002) |
| Population with smoke-free restaurant laws, % | 49.8 (44.99) | 0 (before January 1999) | 100 (since June 2002) |
| Number of NRT units sold per month | 203 420 (72 310) | 75 600 (December 1995) | 353 700 (July 2006) |
| NRT sales per monthb | 5 429 920 (1 930 380) | 2 157 570 (December 1995) | 9 530 000 (September 1999) |
| Number of bupropion units sold per month | 6770 (20 240) | 0 (before November 2000) | 181 800 (April 2001) |
| Bupropion sales per monthb | 1 264 770 (4097.17) | 0 (before November 2000) | 38 247 520 (April 2001) |
Note. GRPs = gross television audience rating points for the population aged 18 years and older representing average potential exposure to ads; NRT = nicotine replacement therapy.
aCost of 1 cigarette pack, expressed as a percentage of average weekly earnings.
bIn 2007 Australian dollars.
FIGURE 2—
Time-series analysis of tobacco control GRPs (a), cigarette costliness (b), NRT GRPs (c), partial smoking bans (d), NRT sales (e), NRT units sold to pharmacies (f), bupropion sales (g), and bupropion units sold to pharmacies (h): Australia, 1996–2006.
Note. GRPs = gross television audience rating points for the population aged 18 years and older representing average potential exposure to ads; NRT = nicotine replacement therapy.
Relation Between Policies and Smoking Prevalence
Exploratory bivariate analysis for the variables NRT units sold to pharmacies, bupropion units sold to pharmacies, and bupropion sales found no immediate or lagged relationship with monthly smoking prevalence, and these variables were excluded from subsequent analysis. We tested for and found no multi-collinearity between the explanatory variables. Transfer functions for all other variables were tested, and the best-fitting transfer functions were selected for multivariate autoregressive integrated moving average modeling (Table 2 ▶), which was then used to jointly examine the impact on smoking prevalence of these explanatory variables. During this analytic process, we removed NRT dollar sales, smoking bans in restaurants, and nicotine replacement therapy GRPs, because they remained not significant (P>.05; models 1, 2, and 3).
TABLE 2—
Parameter Estimates From Conditional Least Squares Autoregressive Integrated Moving Average Model of Monthly Adult Smoking Prevalence: Australia, June 1995 to December 2006
| Model 1 | Model 2 | Model 3 | Model 4 | |||||
| b (SE) | P | b (SE) | P | b (SE) | P | b (SE) | P | |
| Tobacco control GRPs (2 months’ laga) | −0.00060 (0.00036) | .103 | −0.00064 (0.00040) | .080 | −0.00065 (0.00036) | .074 | −0.00077b (0.00034) | .025 |
| Cigarette costliness (immediate effect) | −5.227 (3.691) | .159 | −5.813 (3.800) | .129 | −8.425 (2.917) | .005 | −8.802c (2.891) | .003 |
| NRT GRPs (2 months’ lag) | −0.00030 (0.00042) | .476 | −0.00043 (0.00040) | .290 | −0.00043 (0.00040) | .283 | ||
| Smoke-free restaurant laws (immediate effect) | −0.0104 (0.0098) | .293 | −0.0104 (0.0103) | .317 | ||||
| NRT sales (immediate effect) | −0.00011 (0.00009) | .232 | ||||||
| Moving average, 1-month lag (θ1d) | 0.905 (0.040) | <.001 | 0.890 (0.041) | <.001 | 0.878 (0.043) | <.001 | 0.879 (0.043) | <.001 |
| Residual auto-correlation at 6-month lag e | 2.65 | .753 | 2.51 | .774 | 2.76 | .736 | 2.23 | .816 |
| Residual auto-correlation at 12-month lag e | 4.65 | .947 | 4.33 | .959 | 4.64 | .948 | 3.80 | .975 |
| Residual auto-correlation at 18-month lag e | 15.32 | .572 | 13.16 | .725 | 14.74 | .614 | 15.00 | .595 |
| Residual auto-correlation at 24-month lag e | 25.65 | .318 | 23.17 | .451 | 24.56 | .373 | 24.39 | .382 |
Note. GRPs = gross television audience rating points for the population 18 years and older representing average potential exposure to ads; NRT = nicotine replacement therapy.
aTransfer function.
bAn increase of 1 GRP per month is associated with a decline in prevalence of 0.00077 percentage points; to estimate a reduction in smoking prevalence of 0.30 percentage points, we divided the desired prevalence percentage point change required (−0.30) by the unstandardized parameter estimate for tobacco control GRPs (−0.00077), giving 390 GRPs.
cAn increase of 1% in cigarette costliness is associated with a decline in prevalence of 8.802 percentage points; to estimate a reduction in smoking prevalence of 0.30 percentage points, we divided the desired prevalence percentage point change required (−0.30) by the coefficient for cigarette costliness (−8.802), giving a 0.03-percentage-point increase in cigarette costliness.
dThis parameter estimate accounts for the effects of time.
eThese are diagnostic parameter estimates that must be nonsignificant for the model to be acceptable.
The final model (model 4) showed a significant effect for tobacco control GRPs at 2 months’ lag (i.e., the effect on smoking prevalence was associated with GRPs that were aired 2 months earlier) and an immediate effect for cigarette costliness. This model satisfied the criteria for acceptability and was insensitive to the order in which nonsignificant variables were removed. An increased level of tobacco control GRPs is associated with an acceleration in the rate of decline in prevalence 2 months later. The coefficient for tobacco control GRPs can be interpreted as the impact of an increase of 1 GRP unit on change in smoking prevalence. The magnitude of the effect is such that, to achieve a temporary 0.30-percentage-point decline in smoking prevalence (95% confidence interval = −0.03, −0.56), a 390-point increase in monthly GRPs 2 months earlier (or each person viewing an average of just under 4 ads per month) would be required.
Increased cigarette costliness also reduced smoking prevalence. A temporary 0.30-percentage-point decline in prevalence (95% confidence interval = −0.11, −0.49) would be expected from a single pack of cigarettes increasing in price by 0.03% of the average person’s weekly income. In November 2006, this meant an increase from AU$11.60 to AU $11.87 (1.39% to 1.42% of weekly income) for the average pack of Peter Jackson or Winfield cigarettes. Thus, a relatively small price increase could achieve a similar reduction in smoking prevalence to a moderate increase in GRPs. There was no interaction between cigarette costliness and tobacco control GRPs. Using our model to forecast future smoking prevalence from July 1996 on, we estimated that these 2 variables were responsible for a 1.97-percentage-point drop in prevalence, or 47% of the observed decline in smoking prevalence.
Because the findings for NRT sales were unexpected, we conducted post hoc autoregressive integrated moving average modeling to examine whether nicotine replacement therapy GRPs, tobacco control GRPs, and cigarette affordability predicted NRT sales. The best-fitting model showed that tobacco control GRPs (b = 0.74; P = .030) and nicotine replacement therapy GRPs (coefficient=1.04; P=.006) were related to NRT sales. Tobacco control GRPs had an immediate and positive impact on NRT sales, whereas NRT advertising had a positive impact with a 2-month delay. Similar results were obtained for NRT units sold to pharmacies.
DISCUSSION
Our finding that increases in cigarette costliness led to rapid reductions in smoking prevalence is consistent with extensive economic research showing that increases in the real price of tobacco are reliably associated with declines in tobacco consumption, regardless of whether this is measured through self-report, aggregate spending, or tax receipts on the sales of tobacco products.21–24 We found that relatively small percentage changes in the cost of a typical pack of cigarettes, expressed as a percentage of the average weekly income, translated into measurable declines in smoking prevalence. Naturally, at the individual level, the size of this effect needs to be interpreted with due regard to the fact that most smokers smoke many packs of cigarettes per week, so the relative size of the total price increase against one’s average weekly earnings multiplies according to how many packs are actually smoked each week.
Our study was unusual in specifically linking reduced adult population smoking prevalence with increasing exposure to ongoing televised tobacco control campaign activity, as opposed to overall state-level tobacco program efforts25–27 or funding levels.28,29 The study also furnished greater detail about the durability and specificity of effects than is possible in annual population surveys30 or cohort studies of adult quitting in response to media campaign activity.31,32 The long data series of monthly smoking prevalence estimates allowed more-detailed examination of the influence of antitobacco advertising and other tobacco control policies than has previously been possible, thereby allowing us to determine lagged effects and the duration of effects. Our models indicated that the effects of tobacco control advertising on smoking prevalence occurred relatively quickly, but the acceleration in prevalence decline also dissipated rapidly in the absence of continued high levels of GRPs.
Although people may recall advertising long after a media campaign ends, we found that behavioral change was more closely tied to recent media exposure. Few studies have been in a position to document such effects. For example, youth smoking susceptibility in Minnesota decreased during a youth smoking prevention media campaign but increased 6 months after the campaign had ended,33 and cervical screening rates that were elevated during a televised media campaign returned to the baseline level only 4 weeks after the campaign had ended.34 Our results suggest that tobacco control media campaigns need adequate exposure levels over relatively frequent intervals to realize their full potential in reducing population smoking prevalence.
A more perplexing finding was that higher monthly sales of NRT and bupropion did not have a detectable impact on monthly smoking prevalence, even though NRT sales increased in response to NRT advertising (as found by Tauras et al.35) and in response to tobacco control advertising. Although NRT and bupropion improve quit rates in randomized trials,36,37 the impact of over-the-counter NRT on rates of cessation success in population studies has been less clear, with concerns about easier access to NRT potentially leading smokers to rely more heavily on the product than on their own motivation to quit. Although one study of retrospective population survey data has documented immediate increases in cessation measures in the months after over-the-counter availability of NRT,38 others have found limited impact of over-the-counter NRT availability on population smoking cessation in subsequent years.39,40 A more recent population study found that use of bupropion or over-the-counter NRT among moderate to heavy smokers improved quit rates, especially among those who had imposed bans on smoking at home.41 In addition, a recent multinational cohort study of smokers in Canada, France, the United Kingdom, and the United States found NRT use to improve 6-month cessation rates among smokers making self-initiated quit attempts.42 Because NRT and bupropion are designed for and tend to be used by heavier smokers,41,43,44 the population reach of these products is much more limited than tobacco tax or mass media interventions, which can reach and influence the entire population.
An average of 203 420 units of NRT were sold to pharmacies per month (maximum, 353 700). Assuming each unit represents 1 user (thereby erring on the side of overestimate), 4.44% of all smokers in an average month used NRT (maximum, 7.72%) in this population of 20 million, of whom we found 22.9% to be smokers. The comparable usage rate for bupropion was 0.15% of all smokers (maximum = 3.97%). Even though there was considerable variability in monthly sales over time, these low overall levels of reach likely mean that effects on prevalence at the population level could not be detected. Unlike cigarette price and tobacco control media campaigns, which have the potential to influence prevalence by reducing smoking uptake and promoting quitting, pharmaceutical cessation products can only influence the cessation component of changes in overall population smoking prevalence. In addition, increases in cigarette price and media campaign exposure have the capacity to increase the population rate of quit attempts, whereas NRT products focus on improving quit rates among those who try. Others have demonstrated how increasing the rate of quit attempts in a population is a critical ingredient for reducing population smoking prevalence.45,46
We observed no effects of the implementation of smoke-free restaurant laws on smoking prevalence. Levy et al.47 found that the impact of smoke-free laws on prevalence is dependent upon preexisting levels of smoke-free restrictions. In Australia, most work-places, including private worksites, were smoke free for many years before restaurant smoke-free laws were implemented.48 None of the states extended smoke-free laws to bars during the period of study.
Limitations
One limitation of our study was that smoking prevalence is a relatively blunt outcome measure. However, measures of quitting behavior or cigarette consumption were unavailable. On the other hand, we used consistent sampling procedures and questionnaire administration, and because smoking prevalence questions were embedded in an omnibus survey, potential response biases (underreporting) in targeted smoking questionnaires were limited.49 Moreover, in-person household surveys have been found to yield higher and presumably more accurate estimates of substance abuse than telephone surveys.50–52 Although response rates declined over time, Biener et al. demonstrated that, even in Massachusetts and California, where social norms against tobacco are more pronounced than in Australia, declining state survey response rates did not compromise the states’ smoking prevalence rates when compared with estimates from the Current Population Survey, which has relatively stable response rates.53
A second limitation was that GRPs measure advertising exposure at the aggregate population level rather than individual exposure. However, higher GRPs lead to greater self-reported recall of advertising,54–56 and these more objective advertising-monitoring data have advantages over self-reported advertising recall, which is correlated with readiness to change smoking behavior.57 A third limitation was that we did not differentiate GRPs according to whether or not they represented the launch phase of a media campaign. Other things being equal, it might be expected that already well-exposed ads could have less behavioral impact than ads that conveyed new messages. However, we have demonstrated that on average, televised tobacco control advertising can have beneficial effects on smoking prevalence.
Overall, the pattern of findings suggest that antitobacco mass media campaigns and increases in the real price of cigarettes are critical public health strategies for reducing overall population smoking prevalence. Pharmaceutical smoking cessation products assist some segments of the population in quitting, and our results do not challenge the findings of randomized controlled trials demonstrating improved cessation in users of these products. However, results of efficacy randomized controlled trials can provide inflated guides to real-world effectiveness, because research participants are subject to the influence of the research—such as regular contact from researchers, questionnaire completion, biochemical validation, and a sense of duty toward the research project—which can enhance compliance.58 Additionally, the relatively small size of the more nicotine-dependent subgroups who use and benefit from NRT and bupropion,44 especially in light of suggestions that this group is proportionally diminishing,59 means that they can make little contribution to declines in population smoking prevalence overall.
The public health gains from reducing tobacco use are huge and incontrovertible, yet governments rarely scale their responses appropriately or consider expenditure on tobacco control as an ongoing and essential service, as they would with primary health care, intensive care, and ambulance services. Our results give scant support for the notion that sustained population-level change in an addictive health-related behavior will reliably result from sporadic television advertising campaigns and product price increases; rather, much like health care services, ongoing exposure to these mass-reach interventions is necessary to reduce smoking prevalence.
Acknowledgments
This study was supported by the Australian National Health and Medical Research Council (grant 396402). Melanie A. Wakefield was supported by an Australian National Health and Medical Research Council research fellowship.
Human Participant Protection The project was approved by the Human Research Ethics Committee of the Cancer Council Victoria.
Peer Reviewed
Contributors M.A. Wakefield and D. Hill originated the study. S. Durkin led data management. M.J. Spittal led statistical analysis. M. A. Wakefield, S. Durkin, M. J. Spittal, M. Siahpush, M. Scollo, J. A. Simpson, S. Chapman, and V. White contributed to analysis and assisted with interpretation. M.A. Wakefield, S. Durkin, and M.J. Spittal drafted the article. All authors revised and approved the final version.
References
- 1.Reducing Tobacco Use: A Report of the Surgeon General (Executive Summary). Atlanta, GA: Centers for Disease Control and Prevention; 2000.
- 2.Doll R, Peto R, Boreham J, et al. Mortality in relation to smoking: 50 years’ observations on male British doctors. Brit Med J. 2004;328:1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mendez D, Warner KE. Adult cigarette smoking prevalence: declining as expected (not as desired). Am J Public Health. 2004;94:251–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fong GT, Cummings KM, Borland R, et al. The conceptual framework of the International Tobacco Control (ITC) Policy Evaluation Project. Tob Control. 2006;15 (suppl 3):iii3–iii11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hornik RC. Evaluation designs for public health communication programs. In: Hornik RC, ed. Public Health Communication: Evidence for Behavior Change. Mahwah, NJ: L Erlbaum Associates; 2002:385–405.
- 6.Roy Morgan Research. Single source. Available at: http://www.roymorgan.com/products/single-source/single-source_home.cfm. Accessed February 20, 2008.
- 7.2006 Census of Population and Housing: Count of Persons Based on Place of Usual Residence. Canberra: Australian Bureau of Statistics; 2007. Catalogue no. 2068.0.
- 8.MTV Weekly TARP Flighter data for Melbourne, Sydney, Brisbane, Perth and Adelaide, 2001–2006. Prepared for The Cancer Council Victoria. North Sydney, Australia: OzTAM Pty Ltd.
- 9.AdEx data, Metro TV audience data, 1995 to 2000. Prepared for The Cancer Council Victoria. Sydney: Nielsen Media Research Australia.
- 10.Szczypka G, Emery S, Wakefield M, Chaloupka F. The Adaptation and Use of Nielsen Media Research Commercial Ratings Data to Measure Potential Exposure to Televised Smoking-Related Advertisements. ImpacTeen Research Paper no. 29. Chicago: University of Illinois at Chicago; 2003. Available at: http://www.impacteen.org/ab_RPNo29_2003.htm. Accessed February 20, 2008.
- 11.Hill D, Carroll T. Australia’s National Tobacco Campaign. Tob Control. 2003;12(suppl 11):ii9–ii14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Scollo M, Owen T, Boulter J. Price discounting of cigarettes during the National Tobacco Campaign. In: Hassard K, ed. Australia’s National Tobacco Campaign: Evaluation Report. Vol 2. Canberra, Australia: Commonwealth Department of Health and Aged Care; 2000:155–200. Available at: http://www.quitnow.info.au/internet/quitnow/publishing.nsf/Content/evaluation-reports. Accessed February 20, 2008.
- 13.Scollo M, Younie S, Wakefield M, Freeman J, Icasiano F. Impact of tobacco tax reforms on tobacco prices and tobacco use in Australia. Tob Control. 2003; 12(suppl II):ii59–ii66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Euromonitor International. Tobacco in Australia. London, England: Euromonitor International; 2006. Available at: http://www.euromonitor.com/Tobacco_In_Australia (purchase required). Accessed December 14, 2006.
- 15.Average Weekly Earnings. Canberra: Australian Bureau of Statistics; 2007. Available at: http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/6302.0Feb%202007?OpenDocument. Accessed February 20, 2008.
- 16.Durrant R, Wakefield M, McLeod K, Clegg-Smith K, Chapman S. Tobacco in the news: an analysis of newspaper coverage of tobacco issues in Australia, 2001. Tob Control. 2003;12(suppl II): ii75–ii81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chapman S, Jamrozik K. Is bupropion (Zyban) causing deaths? Med J Aust. 2002;176:134. [DOI] [PubMed] [Google Scholar]
- 18.Smoking Cessation 1995–2006. Report N07B prepared for The Cancer Council Victoria. Crows Nest, Australia: IMS Health Australia Pty Ltd; 2006.
- 19.Box GEP, Jenkins GM, Reinsel GC. Time Series Analysis: Forecasting and Control. 3rd ed. Englewood Cliffs, NJ: Prentice-Hall; 1994.
- 20.Pankratz A. Forecasting With Dynamic Regression Models. New York, NY: Wiley; 1991.
- 21.Curbing the Epidemic: Governments and the Economics of Tobacco Control. Washington, DC: The World Bank; 1999. Available at: http://www1.worldbank.org/tobacco. Accessed February 20, 2008.
- 22.Chaloupka F. Economic approaches. In: Reducing Tobacco Use: A Report of the US Surgeon General. Atlanta, GA: Centers for Disease Control and Prevention; 2000;295–369.
- 23.Chaloupka F, Warner K. The economics of smoking. In: Newhouse J, Cuyler A, ed. The Handbook of Health Economics. New York, NY: Elsevier; 2001; 1539–1627.
- 24.Gallet C, List J. Cigarette demand: a meta-analysis of elasticities. Health Econ. 2003;12: 821–835. Available at: http://www3.interscience.wiley.com/cgi-bin/abstract/101520325. Accessed February 20, 2008. [DOI] [PubMed] [Google Scholar]
- 25.Pierce JP, Gilpin EA, Emery SL, et al. Has the California tobacco control program reduced smoking? JAMA. 1998;280:893–899. [DOI] [PubMed] [Google Scholar]
- 26.Biener L, Harris JE, Hamilton W. Impact of the Massachusetts tobacco control programme: population based trend analysis. Brit Med J. 2000;321:351–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Messer K, Pierce JP, Zhu SH, et al. The California Tobacco Control Program’s effect on adult smokers: (1) Smoking cessation. Tob Control. 2007;16:85–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hill DJ, White VM, Scollo MM. Smoking behaviours of Australian adults in 1995: trends and concerns. Med J Aust. 1998;168:209–213. [DOI] [PubMed] [Google Scholar]
- 29.Farrelly MC, Pechacek TF, Chaloupka FJ. The impact of tobacco control program expenditures on aggregate cigarette sales: 1981–2000 [published correction appears in J Health Econ. 2004;23:419]. J Health Econ. 2003;22:843–849. [DOI] [PubMed] [Google Scholar]
- 30.Ellis JA, Perl SB, Frieden TR, et al. Decline in smoking prevalence, New York City, 2002–2006. MMWR Morb Mortal Wkly Rep. 2007;56:604–608. [PubMed] [Google Scholar]
- 31.McAllister A, Morrison TC, Hu S, et al. Media and community campaign effects on adult tobacco use in Texas. J Health Commun. 2004;9:95–109. [DOI] [PubMed] [Google Scholar]
- 32.Hyland A, Wakefield M, Higbee C, Szczypka G, Cummings KM. Anti-tobacco television advertising and indicators of smoking cessation in adults: a cohort study. Health Educ Res. 2006;21:348–354. [DOI] [PubMed] [Google Scholar]
- 33.Sly D, Arheart K, Dietz N, et al. The outcome consequences of defunding the Minnesota youth tobacco-use prevention program. Prev Med. 2005;41:503–510. [DOI] [PubMed] [Google Scholar]
- 34.Mullins R, Wakefield M, Broun K. Encouraging the right women to attend for cervical cancer screening: results from a targeted television campaign in Victoria, Australia. Health Educ Res. Published online July 5, 2007. doi:10.1093/her/cym021. [DOI] [PubMed]
- 35.Tauras JA, Chaloupka FJ, Emery S. The impact of advertising on nicotine replacement therapy demand. Soc Sci Med. 2005;60:2351–2358. [DOI] [PubMed] [Google Scholar]
- 36.Silagy C, Lancaster T, Stead L, Mant D, Fowler G. Nicotine replacement therapy for smoking cessation. Cochrane Database Syst Rev. 2004;3:CD000146. [DOI] [PubMed] [Google Scholar]
- 37.Hughes JR, Stead LF, Lancaster T. Antidepressants for smoking cessation. Cochrane Database Syst Rev. 2004;4:CD000031. [DOI] [PubMed] [Google Scholar]
- 38.Reed MB, Anderson CM, Vaughn JW, Burns DM. The effect of over-the-counter sales of the nicotine patch and nicotine gum on smoking cessation in California. Cancer Epidemiol Biomarkers Prev. 2005;14: 2131–2136. [DOI] [PubMed] [Google Scholar]
- 39.Pierce JP, Gilpin EA. Impact of over-the-counter sales on effectiveness of pharmaceutical aids for smoking cessation. JAMA. 2002;288:1260–1264. [DOI] [PubMed] [Google Scholar]
- 40.Thorndike AN, Biener L, Rigotti NA. Effect on smoking cessation of switching nicotine replacement therapy to over-the-counter status. Am J Public Health. 2002;92:437–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gilpin EA, Messer K, Pierce JP. Population effectiveness of pharmaceutical aids for smoking cessation: what is associated with increased success? Nicotine Tob Res. 2006;8:661–669. [DOI] [PubMed] [Google Scholar]
- 42.West R, Zhou X. Is nicotine replacement therapy for smoking cessation effective in the “real world”? Findings from a prospective multinational cohort study. Thorax. 2007;62:998–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shiffman S, DiMarino ME, Sweeney CT. Characteristics of selectors of nicotine replacement therapy. Tob Control. 2005;14:346–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Biener L, Reimer RL, Wakefield M, Szczypka G, Rigotti NA, Connolly G. Impact of smoking cessation aids and mass media among recent quitters. Am J Prev Med. 2006;30:217–224. [DOI] [PubMed] [Google Scholar]
- 45.Chapman S. Accelerating smoking cessation and prevention in whole communities. In Chapman S. Public Health Advocacy and Tobacco Control: Making Smoking History. Malden, MA: Blackwell Publishing; 2007;127–152.
- 46.Zhu S-H. Increasing cessation in the population: quit attempts versus successful quit attempts. Presented at: 13th World Conference on Tobacco OR Health; July 12–15, 2006; Washington, DC. Available at: http://www.2006conferences.org/WCTOHPresent/breeze/0714/1050-Zhu/index.htm#slide=1. Accessed February 20, 2008.
- 47.Levy DT, Friend K, Polishchuk E. Effect of clean indoor air laws on smokers: the clean air module of the SimSmoke computer simulation model. Tob Control. 2001;10:345–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Germain D. Smoking Bans in Victorian Workplaces: 2005 Update. Melbourne, Australia: Centre for Behavioural Research in Cancer, The Cancer Council Victoria; June 2007. CBRC Research Paper Series no. 24. Available at: http://www.cancervic.org.au/downloads/cbrc_research_papers/smokingbans05_rps24.pdf. Accessed February 20, 2008.
- 49.Cowling DW, Johnson TP, Holbrook BC, Warnecke RB, Tang H. Improving the self-reporting of tobacco use: results of a factorial experiment. Tob Control. 2003;12:178–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Johnson T, Hougland J, Clayton RR. Obtaining reports of sensitive behaviour: a comparison of substance use reports from telephone and face-to-face interviews. Soc Sci Q. 1989;70:174–183. [Google Scholar]
- 51.Aquilino W. Telephone versus face-to-face interviewing for household drug use surveys. Int J Addict. 1992;27:1131–1136. [DOI] [PubMed] [Google Scholar]
- 52.McAuliffe W, Geller S, LaBrie R, Paletz S, Fournier E. Are telephone surveys suitable for studying substance abuse? Cost, administration, coverage and response rate issues. J Drug Issues. 1998;28:455–482. [Google Scholar]
- 53.Biener L, Garrett CA, Gilpin EA, Roman AM, Currivan DB. Consequences of declining survey response rates for smoking prevalence estimates. Am J Prev Med. 2004;27:254–257. [DOI] [PubMed] [Google Scholar]
- 54.Emery S, Wakefield MA, Terry-McElrath Y, et al. Televised state-sponsored antitobacco advertising and youth smoking beliefs and behavior in the United States, 1999–2000. Arch Ped Adol Med. 2005;159: 639–645. [DOI] [PubMed] [Google Scholar]
- 55.Southwell BG, Barmada CH, Hornik RC, Maklan DM. Can we measure encoded exposure? Validation evidence from a national campaign. J Health Commun. 2002;7:445–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Niederdeppe J. Assessing the validity of confirmed ad recall measures for public health communication campaign evaluation. J Health Commun. 2005;10: 635–650. [DOI] [PubMed] [Google Scholar]
- 57.Borland R, Balmford J. Understanding how mass media campaigns impact on smokers. Tob Control. 2003;12 (suppl II):ii45–ii52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Del Boca FK, Darkes J. Enhancing the validity and utility of randomized clinical trials in addictions treatment research: treatment implementation and research design. Addiction. 2007;102:1047–1056. [DOI] [PubMed] [Google Scholar]
- 59.Warner KE, Burns DM. Hardening and the hard-core smoker: concepts, evidence, and implications. Nicotine Tob Res. 2003;5:37–48. [DOI] [PubMed] [Google Scholar]