Fig. 4.
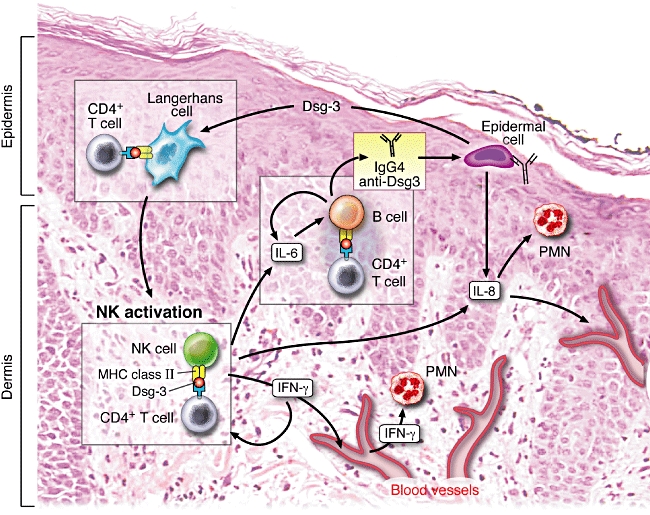
Representation of the possible role of natural killer (NK) cells in pemphigus vulgaris (PV) − a hypothetical model for pathogenesis of clinical disease. NK cells acting as antigen-presenting cells present desmoglein 3 (Dsg3) peptides to CD4+ T cells, both of which hone into the perilesional skin and oral mucosa, from the peripheral blood. The proliferating T cells secrete interleukin (IL)-6, which stimulates resident B cells to produce anti-Dsg3 antibodies. NK cells produce interferon (IFN)-γ, which then further up-regulates major histocompatibility complex (MHC) class II expression and simultaneously attracts other NK cells to the site of pathology. IL-8 secreted by activated NK cells will stimulate resident polymorphonuclear cell (PMN) and monocytes. These NK cells, IL-8, IL-6, IFN-γ and other cytokines, chemokines and inflammatory mediators are absorbed into the blood vessels of the skin and mucosal tissues and carried to lymph nodes, spleen and bone marrow. Here the inflammatory response and the levels of autoantibody production may be amplified significantly. Once substantial levels of the autoantibody and inflammatory chemokines and cytokines reach the target tissue, the adhesions between the epithelial cells in the stratum malphigii are lost and clinical disease is observed. The simultaneous critical role of the central immune system, perhaps in the bone marrow, spleen or lymph nodes, and the essential role of the microenvironment of the skin and mucosal tissues are emphasized in this model.
