Abstract
A 77 year old aboriginal woman in an isolated village became drowsy and shocked. Poor weather conditions delayed the arrival of the medical and support team—the roads had been seriously destroyed by torrential rains and helicopter was the only means for delivering critical medical care and support. While waiting for the arrival of the helicopter, and in the absence of the necessary emergency medical equipment, the patient's condition deteriorated. Administration of persistent emergency acupuncture stimulation for 80 minutes helped maintain the patient's vital signs until successful transfer of the patient to hospital. She recovered without any complications of shock and was discharged six days later.
Keywords: acupuncture, septic shock, shock resuscitation
On 25 August 2004, Typhoon Aere battered northern Taiwan. Torrential rains soaked the island throughout the night, washing away the roads of the mountainous Hsinchu County. With land transportation in jeopardy, helicopter became the only means for delivering critical medical care and support. Four days after the disaster, the National Disaster Relief Center received a request for emergency medical care for a 77 year old aboriginal woman from an isolated mountain tribe. She had been drowsy for more than 24 hours. After a 30 minute flight, the helicopter landed on a piece of dry land in the wilderness, the only suitable place for landing within 2 km of the patient's location. We walked for an hour before we reached her home.
On arrival, we found her lying on her bed, feeling weak. Physical examination revealed that her blood pressure was 80/50 mm Hg and body temperature 36.2 °C. She was drowsy and her lips and extremities were cyanosed. On chest auscultation there were crackles. Her family reported that she had developed mild fever and had had frequent bouts of watery diarrhoea after eating stale food from the refrigerator (there had been a power cut for three days). Several episodes of cold sweating and high fever were noted subsequently. Then she became drowsy and passed bloody and mucus‐rich stool.
Initial assessment revealed that she was shocked and needed emergency resuscitation, but the only resuscitation equipment available was a 500 ml bottle of normal saline. After administering this, her blood pressure was 85/50 mm Hg and body temperature 36.0 °C. At the same time, we requested for emergency helicopter transport from the National Disaster Relief Center.
The family quickly assembled a stretcher with some bamboo cuttings to carry the patient. We alternately walked and ran in the rain drenched paths, racing against time. The helicopter had been trying to land but was unable to due to poor weather conditions. After 40 minutes we finally arrived at the landing place. The patient seemed to be deteriorating and we could not feel her carotid or femoral artery pulse or detect her blood pressure. Her body was cold and her face and extremities cyanosed. Her breathing was shallow and rapid at first but gradually almost came to a halt.
Critical medical equipment was not available. We had no endotracheal tube, intravenous fluids, oxygen, adrenaline, or electrocardiography monitor. There was little sign of breathing. Left with no choice, we tried emergency acupuncture to resuscitate her. We chose seven acupuncture points including Renzhong (DU‐26) on the face (see fig 1), bilateral Heku (LI‐4), Neiguan (P6) and Shixuan (Extra) on both hands, bilateral Zusanli (ST‐36) on both lower legs, and Tiantu (REN‐22) on the suprasternal notch area. Ten minutes later, we could feel the pulsation in her carotid and femoral arteries. She began to take deep breaths and the cyanosis also disappeared. At that time, her blood pressure was 70/50 mmHg. We continued acupuncture stimulation, particularly on Renzhong (DU‐26). Every time the acupuncture points were stimulated, she responded with body movement or loud cries.
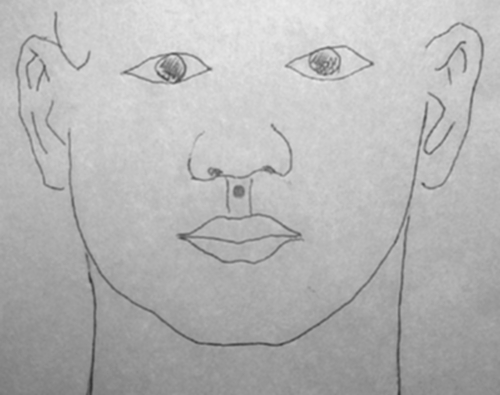
Figure 1 The main acupuncture point—Renzhong (DU‐26)—in critical condition according to traditional Chinese medicine.
The weather began clearing up and the dark clouds disappeared 40 minutes later. The helicopter landed successfully and the patient was rushed to the hospital. During the 30 minute flight, we continued stimulating the acupuncture points. On arrival at the emergency department of the regional hospital, the physical examination revealed no palpable carotid pulse, undetectable blood pressure, and Glasgow Coma Scale score was E1V1M5. The monitor showed heart rate of 116 beats/min (fig 2), respiratory rate 10 breaths/min, and oxygen saturation 85% under 8 l/min oxygen flow mask. Laboratory findings were as follows: one touch glucose 133 mg/dl; leucocytosis with white blood count 24 120/μl and left shift (band 5%); pyuria and bacteria on urinalysis; and impaired renal function (BUN 40.6 mg/dl and creatinine 4.6 mg/dl). She was given hydration and antibiotics, and admitted to the intensive care unit. The next day, a urine culture showed Gram positive cocci which were sensitive to the antibiotics. She was discharged six days later without any complications due to the shock.
Figure 2 Upper panel: initial monitor reading at the hospital; blood pressure was undetectable and Glasgow Coma Scale score was E1V1M5. Lower panel: eight minutes after fluid administration, the patient's blood pressure rose to 59/38 mmHg and Glasgow Coma Scale was E2V2M5.
Discussion
Acupuncture is used to treat a variety of health problems, mostly in relation to chronic diseases, physiotherapy, and pain control.1 It is seldom used in critical conditions, especially for shock resuscitation, an emergent and critical procedure. Many advanced approaches to shock resuscitation and critical medical care have been proposed,2 but no one has suggested acupuncture. Some related studies have been reported,3,4 but how emergency acupuncture stimulation benefits shock resuscitation remains unclear. Although the findings of our case report need to be verified in a larger sample, the initial results of the intervention in our patient did show the beneficial effects of emergency acupuncture stimulation for shock resuscitation. The definitive benefits need to be further determined.
Acknowledgements
We thank all the volunteers and staff of the emergency medical care team who care for the remote mountain tribes in Taiwan.
Footnotes
Competing interests: none declared
References
- 1.Andrew V, Catherine Z. ABC of complementary medicine: Acupuncture. BMJ 1999319973–976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moore F A, Mickinley B A, Moore E E. The next generation in shock resuscitation. Lancet 20043631988–1996. [DOI] [PubMed] [Google Scholar]
- 3.Lin M C, Nahin R, Gershwin M E.et al State of complementary and alternative medicine in cardiovascular, lung and blood research (executive summary of a workshop). Circulation 20011032038–2041. [DOI] [PubMed] [Google Scholar]
- 4.Lin P, Pitsillides K, Rendig S.et al Reversal of reflex‐induced myocardial ischemia by median nerve stimulation: a feline model of electroacupuncture. Circulation 1998971186–1194. [DOI] [PubMed] [Google Scholar]



