Abstract
Purpose
Heart failure is the ultimate complication of cardiac involvements in diabetes. The purpose of this review was to summarize current literature on heart failure among people with diabetes mellitus in sub-Saharan Africa (SSA).
Method
Bibliographic search of published data on heart failure and diabetes in sub-Saharan Africa over the past 26 years.
Results
Heart failure remains largely unexplored in general population and among people with diabetes in Africa. Heart failure accounts for over 30% of hospital admission in specialized cardiovascular units and 3%–7% in general internal medicine. Over 11% of adults with heart failure have diabetes. Risk factors for heart failure among those with diabetes include classical cardiovascular risk factors, without evidence of diabetes distinctiveness for other predictors common in Africa. Prevention, management, and outcomes of heart failure are less well known; recent data suggest improvement in the management of risk factors in clinical settings.
Conclusions
Diabetes mellitus is growing in SSA. Related cardiovascular diseases are emerging as potential health problem. Heart failure as cardiovascular complication remains largely unexplored. Efforts are needed through research to improve our knowledge of heart failure at large in Africa. Multilevel preventive measures, building on evidences from other parts of the world must go along side.
Keywords: diabetes mellitus, cardiovascular diseases, heart failure, sub-Saharan Africa
Introduction
Diabetes mellitus, accounted for in major part by type 2 diabetes is increasing alarmingly in all parts of the world, including sub-Saharan Africa (SSA) (Wild et al 2004). According to the International Diabetes Federation (IDF) estimations, 246 millions people around the world suffer from diabetes in 2007. This figure will increase by 55% to reach 380 million by the year 2025 (IDF 2006). Diabetes-related complications, led by cardiovascular complication (CVD) are already contributing a great deal to the global burden of disease (Roglic et al 2005). In General, up to 80% of deaths among people with diabetes occur thru CVD, and CVD account for 75% of hospital admission in diabetes. Numerous epidemiological studies are concordant over the fact that the risk of experiencing a CVD event in people with diabetes is two to four times greater than that among those without diabetes (Kannel and McGee 1979; Panzram 1987; Stamler et al 1993; APCSC 2003). While atherosclerotic vascular disease accounts for much of the cardiovascular morbidity and mortality among diabetic patients, congestive heart failure (CHF) is another key complication associated with diabetes, with an incidence that is two to five times greater than that among individuals without diabetes (APCSC 2003). Once heart failure occurs, patients with diabetes have poorer prognosis than their nondiabetic counterparts.
Despite the growing importance of diabetes mellitus in SSA, evidence to support the related complications and particularly cardiovascular complications are still few. In a recent review, we have shown that although considered to be rare, CVD was on the rise among people with diabetes in SSA and was regularly associated with classical risk factors (Kengne et al 2005). However, individual cardiovascular complications and more precisely heart failure among people with diabetes in SSA are less well known. We aim in this review to summarize currently existing literature on heart failure in diabetes in SSA. Such information has relevance both for clinical and epidemiological purposes, given the rapidly changing pattern of disease occurrence in this part of the world.
Source of data
We searched MEDLINE® and reference lists of literature on heart failure and diabetes in SSA in June 2007. Initial MEDLINE search using the keys words “heart failure”, “diabetes”, and “Africa” provided 23 entries spanning from 1966 to 2006. This was considered inconsistent and an extended search using a combination of key words like “heart failure”, “cardiovascular disease”, “stroke”, and “Africa” without restriction to people with diabetes yielded 1,245 entries extending from 1961 to 2007. Data search used in this review was limited to studies published after 1980. This cut-off was chosen because data collected before 1980 may no longer reflect the current situation of heart failure in SSA. The database obtained was contracted by eliminating duplicates, studies from Northern African countries, studies done on migrant Africans, case reports, and studies without heart failure or cardiovascular disease as main focus. The final database consisted of 181 studies from a number of SSA countries, distributed over the 26 years, which is depicted by Figure 1. Some of these publications included multiple reports from the same studies. Literature from other parts of the world is used where relevant. The majority of articles were retrospective hospital-based studies in major urban cities that addressed aspects of heart failure and cardiovascular disease including incidence, types, risk factors, management, and outcomes. The data sources are mentioned wherever used in the text.
Figure 1.
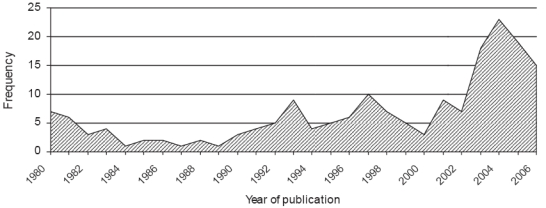
Evolution of published literature on cardiovascular diseases and heart failure in sub-Saharan Africa over the period 1980–2006.
There are very limited published studies describing the burden of heart failure in SSA, most particularly among people with diabetes. Extrapolations from data published elsewhere have serious limitations. As new and better epidemiological data become available in the region, it will be possible to know the actual burden of heart failure in people with diabetes from this region.
Results and discussion
The burden of diabetes in Sub-Saharan Africa
The burden of diabetes in Africa has been presented in details elsewhere (Motala 2002; IDF 2006; Kengne and Mbanya 2006). The consistent theme is that the magnitude of diabetes mellitus and related health issues has not been reliably estimated for African countries. Extrapolation from existing point prevalence data suggest that 0.5% to 10% of adult population in Africa suffer from type 2 diabetes (Mbanya et al 2006). Plotting these figures on a time scale indicates that the prevalence of diabetes has increased by two- to ten-folds in both rural and urban settings in most African countries over the past two to three decades, (Mbanya et al 2006). The Diabetes Atlas provides some estimates and projections of diabetes figures for all its regions. In SSA, 10.4 million individuals currently have diabetes, and projections by the IDF suggest that these figures will exceed 18.7 million by 2025 (IDF 2006). Determinants of the growing prevalence of diabetes in Africa are similar to those reported elsewhere. These include rapid urbanization, sedentary lifestyles, obesity, and unhealthy eating diets (Mbanya et al 2006). Available prevalence studies are concordant over the fact that diabetes in Africa is 1.5 to 2 times more frequent in urban compared to rural areas. However, unpublished data from Cameroon suggest an attenuation of this rural–urban gradient with time.
Epidemiology of heart failure in Sub-Saharan Africa
Heart failure is a major and growing public health problem on a global perspective. In spite of the scarcity of published literature on heart failure in SSA, the few available evidence suggest that the rate of hospital admission for heart failure is comparable with rates from the rest of the world, but the pathophysiology and etiologies are different (Mayosi 2007). Heart failure failure seems to be mainly due to systolic dysfunction and occurs as a major complication of high blood pressure in Africa and the first cause of hospital admission among those with hypertension (Table 1) in cardiology units (Njoh 1990; Mensah et al 1994). In general internal medicine services, heart failure has been described as the 5–6th cause of admission (Bardgett et al 2006). In Zimbabwe, while the proportion of hospital admission of patients with noncommunicable diseases has decreased over time, patients with heart failure have continued to contribute about 6% of hospital admission (Bardgett et al 2006). More importantly, over the same period, the proportion of death resulting from heart failure has significantly increased.
Table 1.
Prevalence of heart failure among patients with hypertension in selected African countries
| Country | Year | Study sample | Prevalence of heart failure |
|---|---|---|---|
| Liberia (Njoh 1990) | 1990 | 105 | 55.2% |
| Niger (Toure et al 1992) | 1989 | 54 | 32.0% |
| Nigeria (Isezuo 2003) | 2003 | 440 | 36.4% |
| Nigeria (Ayodele et al 2005) | 2005 | 203 | 10.8% |
The underlying process leading to heart failure in most developed countries is dominated by coronary heart disease (Mendez and Cowie 2001). In developing countries and most particularly those of SSA, nonischaemic causes of heart failure are dominant, with hypertensive heart disease, rheumatic heart disease, and cardiomyopathy accounting for over 75% of cases in most series (Amoah and Kallen 2000; Mendez and Cowie 2001). However, ischemic cardiomyopathies also seem to be growing in this setting (Table 2). That cardiac involvements in human immunodeficiency virus (HIV) infection, cor pulmonale, and pericarditis contribute to over 20% of cases of heart failure in SSA reflects the continuing impact of HIV and tuberculosis on heart disease on the continent (Magula and Mayosi 2003; Mayosi et al 2005). Earlier reports from SSA highlight the major importance of rheumatic valvular diseases among causes of heart failure. However, recently published data favor hypertension as the dominant cause of heart failure in this part of the world (Mayosi 2007). Lessons from the changing epidemiology of heart failure in developed countries suggest that the burden of this disease will dramatically increase over the first half of this century.
Table 2.
Main causes of heart failure in African adults
| Country | Sample | Men(%) | Mean age (years) | Hypertension | Cardiomyopathy | Valvular disease | IHD | Pericardial diseases | Pulmonar diseases | Congenital heart disease |
|---|---|---|---|---|---|---|---|---|---|---|
| Cameroon (Kingue et al 2005) | 167 | 59.3% | 57 | 54.5% | 26.3% | 24.5% | 2.4% | 2.4% | 7.8% | 1.2% |
| Ghana (Amoah and Kallen 2000) | 572 | 54.5% | 42 | 22.6% | 16.9% | 20.2% | 10.2% | 7.3% | - | 7.5% |
| Guinea (Fofana et al 1988) | 574 | 59.7% | 49 | 37.5% | 37.4% | 14% | - | 0.3% | - | - |
| Kenya(Oyoo and Ogola 1999) | 91 | 48.4% | - | 17.6% | 25.2% | 32% | 2.2% | 13.2 | - | - |
| Nigeria(Ola et al 2006) | 100 | 58.0% | 63 | 58% | 11% | 10% | - | - | 15% | 8% |
| Senegal(Thiam 2003) | 170 | - | 50 | 45% | 28% | 44.7% | 18.9% | - | 3.5% | - |
Compared to studies from other part of the world, heart failure in Africa tends to occur at a much younger age with most cases recorded around the 5th and 6th decade (Table 2). This young age reflect the major contribution of rheumatic valvular disease to heart failure, but could also be accounted for by the early onset and severity of hypertension among Blacks. As reported elsewhere, most African studies have uniformly described a male predominance among those with heart failure in Africa (Table 2). Although heart failure management has benefited from major advances in the recent years, case fatality among people with heart failure remains high worldwide. Hospital case fatality among those with heart failure in Africa ranges from 9% to 12.5%. This consistent death rate ranks heart failure among the major causes of death of cardiovascular origin in Africa.
The clinical presentation of heart failure in Africa is characterized by the high proportion of symptomatic patients. More than 50% of patients present in stage III and IV of the NYHA classification (Fofana et al 1988). Clinical signs and symptoms are similar to those reported elsewhere, but are dominated by the high prevalence of nonspecific features (Kingue et al 2005). Most clinical studies of heart failure in SSA were conducted in the pre-echocardiographic era or without the application of echocardiography. With recent echocardiographic studies, it is heartening to note that systolic dysfunction, a treatable and preventable form of heart failure is the most frequent cardiac dysfunction found (Kingue et al 2005). Most echocardiographic findings are typical findings expected for the various potential underlying aetiologies of heart failure. Three major trends emerge from few studies that have addressed the issue of management of heart failure in SSA: Firstly, underutilization of medications with proven efficacy such as angiotensin-converting enzyme inhibitors (ACEI) and beta blockers. For example, in a study from Nigeria, only 65% of heart failure patients were on ACEI (Adewole et al 1996). In another study from Cameroon, 19% of patients with heart failure were on beta blockers (Kingue et al 2005). Second, when medications are appropriately prescribed, this is not always followed by patient compliance (Bhagat and Mazayi-Mupanemunda 2001). Finally, we were unable to identify reports of cardiac resynchronization therapy or ventricular assistant devices and heart transplantation, which are therapeutic options not yet accessible in most African countries.
Heart failure and diabetes in sub-Saharan Africa
Studies from other parts of the world suggest that up to 25% of people with heart failure have diabetes (Bauters et al 2003). In the Heart Failure in Israel Survey (HFIS), up to 50% of patients admitted with heart failure had diabetes (Garty et al 2007). Diabetes mellitus has also been recognized to play a key role in the pathogenesis, prognosis, and outcomes of heart failure (Solang et al 1999). Available data from Africa relate to prevalence of diabetes among those with heart failure in hospital retrospective review studies. In the study by Thiam and coworkers (2003) in Senegal, 11.8% of heart failure patients had diabetes. In a study of 572 consecutive patients with heart failure in Ghana, 17% of those with coronary artery disease had diabetes (Amoah and Kallen 2000). In a selective group of patients with heart failure in Nigeria, the proportion of those with diabetes was found to be 58% (Ola et al 2006). No study has so far directly compared the features of heart failure among people with and without diabetes in SSA.
Determinants of heart failure in diabetes in Africa
Many mechanisms exist to explain the high vulnerability of people with diabetes to heart failure. These include competing cardiovascular risk factors, diabetic specific cardiomyopathy, and other diabetes related risk factors, the accelerated coronary atherosclerosis in diabetes, and in the African setting, the potential interaction between diabetes and other risk factor for heart failure prevalent in SSA.
Classical cardiovascular risk factors
Available evidence supports the view that major cardiovascular risk factors affect the risk of future cardiovascular events in a similar way regardless of diabetes status (Kannel and McGee 1979; Balkau et al 1993; Adlerberth et al 1998). However, because most of these risk factors tend to cluster in people with diabetes, the resulting absolute risk of experiencing a cardiovascular event will be much higher among people with diabetes compared with their nondiabetic counterparts (Stamler et al 1993). Major risk factors are also consistent across populations and include in addition to diabetes mellitus, age, hypertension and dyslipidemia, smoking, and male gender. Although outcomes studies relating the exposure to these factors to the risk of major cardiovascular events including heart failure are still lacking in SSA for both the general population and people with diabetes, it would be anticipated that the nature of this association will be similar to that reported in other parts of the world. However, the strength of the association may differ at least for some risk factors. For example, in the INTERHEART study, African participants with myocardial infarction were significantly younger compared with participants from other parts of the world (Steyn et al 2005). Similarly, when most of the classical risk factors are considered on their absolute levels, people with diabetes from Africa tend to display different profiles. For instance, the age at onset of type 2 diabetes in Africa is much younger, while people with diabetes from Africa tend to display high prevalence of hypertension (Choukem et al 2007) and prevalence of dyslipidemia, and smoking habits are still low among Africans in general.
Diabetes-related risk factors
Chronic hyperglycemia, insulin resistance and accumulation of collagen and other glycation end-products in the myocardium of people with diabetes are believed to be associated with pathological changes at the level of cardiac myocytes that ultimately result in diabetic cardiomyopathy with increased myocardial stiffness and early abnormal diastolic function. Diabetic cardiomyopathy is characterized by defects of left ventricular function in the absence of significant CAD or systemic hypertension (Bell 1995, 2003). The condition is associated with important clinical consequences, such as increased susceptibility to hypertension-mediated damage, an increased mortality rate after acute myocardial infarction and progression to symptomatic heart failure (Factor et al 1980; Jaffe et al 1984). In addition to diabetic cardiomyopathy, left ventricular hypertrophy and systolic dysfunction that is often asymptomatic and may lead to congestive heart failure have been described in African diabetic patients. Indeed up to 50% of asymptomatic diabetic patients may present with echocardiographic abnormalities (Babalola and Ajayi 1992). However, appropriate comparison of ventricular indexes with matched background nondiabetic population is still lacking. In one of the earliest study of infra-clinical alterations of the left ventricular functions, Famuyiwa and co-workers (1985) compared 89 participants with diabetes with 45 nondiabetic controls, and reached the conclusion that people with diabetes were less vulnerable to vascular complications. However, this study has been contradicted by most recent reports both from Nigeria and elsewhere (Mbanya et al 2001; Danbauchi et al 2005). In a study from Cameroon, Mbanya and his colleagues (Mbanya et al 2001) found a 40% and 55% prevalence of left ventricular hypertrophy and systolic dysfunction among their selective sample of 40 patients with diabetes. This was in keeping with another study from Nigeria in which Danbauchi and his team reported significant sub-clinical cardiomyopathy in people with diabetes (Danbauchi et al 2005). In another recent study among population with hypertension in South Africa, the prevalence of LVH was not different between those with and without type 2 diabetes. In addition, diabetes in this study was not an independent predictor of LVH in multivariate analysis (Rayner and Becker 2006). In the midst of these inconsistencies, cardiomyopathy among people with diabetes in Africa deserves further attention, both to clarify the existence and explore underlying pathophysiologic derangements.
Other contributors
Underlying causes of heart failure vary consistently across regions in the world. In SSA, hypertension, valvular heart diseases, and various cardiomyopathies are the dominant causes among adults (Sliwa et al 2005; Commerford and Mayosi 2006; Opie 2006). One question is whether there is any interaction between diabetes and other determinants of heart failure mostly found in Africa. In the first analysis, it could be envisaged that diabetes would act at least as a co-factor and may further accelerate the onset of heart failure in patients who are cumulating other risk factors. A controversial role of diabetes as independent risk factor for nonrheumatic valvular disease has been described elsewhere, but not yet in Africa (Movahed et al 2007). However, if confirmed in addition to rheumatic heart disease, already common in Africa, a greater contribution of valvular disease to heart failure would be expected in Africa in the context of the growing burden of diabetes. Anemia, a common finding in individuals with diabetes and particularly those with kidney involvement, may precipitate the unset or exacerbate the already established heart failure in this category of patients. In Africa, even among those without diabetes, anemia is already frequent as a result of infectious diseases and nutritional deficiencies (Ladipo 1981). Heart failure is rare among pregnant women in Africa and is most often the consequence of valvular heart diseases (Abengowe et al 1980; Aggarwal 1980). The congestive phase tends to occur more in the postpartum period and the incidence is not affected by parity and socioeconomic class (Abengowe et al 1980). As a contributor, diabetes has not yet been reported.
Management of heart failure in diabetes
The long-term care of diabetic patients with heart disease poses a particular challenge. Various combinations of risk factors, progression of the coronary heart disease, and complications with further organic damage by the underlying diabetes frequently necessitate a differentiated diagnostic work-up and management.
Control of cardiovascular and diabetes-related risk factors
Compelling evidence from cardiovascular outcomes trials indicates that treatment with drugs that block the rennin – angiotensin system are cardioprotective in diabetics with microalbuminuria and early stages of kidney disease. Multiple risk factor intervention aimed at optimal blood pressure control, lowering LDL cholesterol and triglyceride levels, treatment with an ACEI or an angiotensin II receptor blocker, administration of once daily low-dose aspirin and smoking cessation together reduce cardiovascular morbidity and mortality in type 2 diabetics. Since there is epidemiologic evidence of a relationship between poor metabolic control and development of heart failure (Iribarren et al 2001), it would be interesting to evaluate whether aggressive treatment addressing the metabolic consequences of diabetes would improve outcome in diabetic patients with heart failure. However, data on glucose control and heart failure are rare and inconclusive (Tang 2006). This is partly due to the lack of trials targeting specifically those with diabetes and heart failure, but also to the poor understanding of the pathophysiologic derangements linking diabetes to heart failure.
Medical treatment of heart failure
Standard medical treatments applied for heart failure in population without diabetes are associated with at least similar beneficial impact in those with diabetes. There remain however some uncertainties about the safety of current antidiabetic medications when used in people with heart failure (Fisman et al 2004; Skouri and Wilson Tang 2007). In addition, agents of the thiazolidinedione class may be associated with increased risk of heart failure in people with diabetes (Lincoff et al 2007; Singh et al 2007). These medications however are likely to be infrequently used in SSA. Despite the concerns about adverse metabolic effect of beta blockers, available evidence support the view that beta blockers and particularly the nonselective vasodilating ones like carvedilol confer similar survival benefit in heart failure patients with and without diabetes (Bell et al 2006). Subgroup analyses from large clinical studies have shown that ACEIs not only reduce mortality in diabetic patients with heart failure, but also reduce the incidence of heart failure in at-risk diabetic patients (Vermes et al 2003).
Cardiac resynchronization therapy and implantable cardioverter-defibrillators
Several trials have shown that cardiac resynchronization therapy (CRT) improves symptoms in patients with advanced heart failure and wide QRS complexes who remain symptomatic in spite of optimal medical therapy (Bradley et al 2003). Comparison of effectiveness of CRT in patients with and without diabetes mellitus shows that the benefit of CRT is similar in both groups (Kies et al 2005). While ICD do not improve functional outcomes, they do provide substantial mortality benefits by preventing sudden cardiac death in patients with heart failure who have an ischemic substrate, poor ejection fraction, and history of ventricular arrhythmias. To our knowledge, no study in SSA has reported results of these novel therapies of heart failure.
Revascularisation
Diabetic patients are known to have reduced long-term survival following percutaneous transluminal coronary angioplasty compared with nondiabetic patients. This survival disadvantage has persisted over time and can at least in part be explained by the high prevalence of comorbidities among people with diabetes (Mathew et al 2004; Wilson et al 2004). There are also some controversies regarding the worse post-procedure outcome in insulin-treated patients compared with those on diet or oral agents (Mathew et al 2004). However, a difference in the outcome if any should be interpreted in the light of the severity of diabetes and related vascular involvements in insulin-treated type 2 diabetic patients.
Heart transplantation
Heart transplantation is the most indicated treatment for end-stage heart failure, but its impact is limited by the scarcity of donor organs and stringent selection criteria for both donors and recipients. For example, the presence of diabetes complications in the past has limited this approach in people with diabetes. Few data are available to suggest that long-term survival in people with diabetes and diabetes related complications compare to that among their counterparts without complications (Morgan et al 2004; Felker et al 2005; Ikeda et al 2007). However, post transplant follow-up face with important diabetogenic effects of classical immunosuppressive drugs. Even when indicated, this treatment option is not widely available in SSA.
Conclusions
One of the earliest documented clinical observations of the syndrome of heart failure originates from Africa (Saba et al 2006). Surprisingly, this disease entity has remained largely unexplored in this part of the world and particularly among the highly vulnerable population with diabetes mellitus. In the general internal medicine service in urban settings, heart failure account for more than 3% of hospital admission, and over 30% among those admitted for cardiovascular diseases. Hypertension, valvular heart diseases, and cardiomyopathies are the main providers of heart failure in SSA, accounting for over 75% of cases in most series. The contribution of diabetes is still ill-studied. However, more than 10% of adults with heart failure also have diabetes. Determinants of heart failure reported elsewhere in people with diabetes are also found among people with diabetes in Africa, but, there are still some inconsistencies about the contribution of diabetic cardiomyopathy. The available pharmacological treatments, such as ACEIs, beta-blockers, and possibly angiotensin receptor blockers, together with a tight glycemic control, as reported elsewhere, must be effective for the treatment of heart failure if adequately used among people with diabetes in Africa.
There is need for more elaborate studies of heart failure in the general population in Africa and in people with diabetes in particular, given their high vulnerability. It is expected that initiatives such as The Heart of Soweto Study (Stewart et al 2006) will provide a body of information on heart diseases and therefore heart failure as observed in SSA communities. There is evidence in support of the existing and growing capacity for research on chronic and cardiovascular diseases in SSA (Hofman et al 2006). If encouraged and provided with the needed support, their efforts are likely to translate into more insight into heart failure and other cardiovascular diseases in countries of this region.
References
- Abengowe CU, Das CK, Siddique AK. Cardiac failure in pregnant Northern Nigerian women. Int J Gynaecol Obstet. 1980;17:467–70. doi: 10.1002/j.1879-3479.1980.tb00190.x. [DOI] [PubMed] [Google Scholar]
- Adewole AD, Ikem RT, Adigun AQ, et al. A three year clinical review of the impact of angiotensin converting enzyme inhibitors on the intra hospital mortality of congestive heart failure in Nigerians. Cent Afr J Med. 1996;42:253–5. [PubMed] [Google Scholar]
- Adlerberth AM, Rosengren A, Wilhelmsen L. Diabetes and long-term risk of mortality from coronary and other causes in middle-aged Swedish men. A general population study. Diabetes Care. 1998;21:539–45. doi: 10.2337/diacare.21.4.539. [DOI] [PubMed] [Google Scholar]
- Aggarwal VP. Obstetric emergency referrals to Kenyatta National Hospital. East Afr Med J. 1980;57:144–9. [PubMed] [Google Scholar]
- Amoah AG, Kallen C. Aetiology of heart failure as seen from a National Cardiac Referral Centre in Africa. Cardiology. 2000;93:11–18. doi: 10.1159/000006996. [DOI] [PubMed] [Google Scholar]
- APCSC. The effects of diabetes on the risks of major cardiovascular diseases and death in the Asia-Pacific region. Diabetes Care. 2003;26:360–6. doi: 10.2337/diacare.26.2.360. [DOI] [PubMed] [Google Scholar]
- Ayodele OE, Alebiosu CO, Salako BL, et al. Target organ damage and associated clinical conditions among Nigerians with treated hypertension. Cardiovasc J S Afr. 2005;16:89–93. [PubMed] [Google Scholar]
- Babalola RO, Ajayi AA. A cross-sectional study of echocardiographic indices, treadmill exercise capacity and microvascular complications in Nigerian patients with hypertension associated with diabetes mellitus. Diabet Med. 1992;9:899–903. doi: 10.1111/j.1464-5491.1992.tb01728.x. [DOI] [PubMed] [Google Scholar]
- Balkau B, Eschwege E, Papoz L, et al. Risk factors for early death in non-insulin dependent diabetes and men with known glucose tolerance status. BMJ. 1993;307:295–9. doi: 10.1136/bmj.307.6899.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bardgett HP, Dixon M, Beeching NJ. Increase in hospital mortality from non-communicable disease and HIV-related conditions in Bulawayo, Zimbabwe, between 1992 and 2000. Trop Doct. 2006;36:129–31. doi: 10.1258/004947506777978217. [DOI] [PubMed] [Google Scholar]
- Bauters C, Lamblin N, Mc Fadden EP, et al. Influence of diabetes mellitus on heart failure risk and outcome. Cardiovasc Diabetol. 2003;2:1. doi: 10.1186/1475-2840-2-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell DS. Diabetic cardiomyopathy. A unique entity or a complication of coronary artery disease? Diabetes Care. 1995;18:708–14. doi: 10.2337/diacare.18.5.708. [DOI] [PubMed] [Google Scholar]
- Bell DS. Diabetic cardiomyopathy. Diabetes Care. 2003;26:2949–51. doi: 10.2337/diacare.26.10.2949. [DOI] [PubMed] [Google Scholar]
- Bell DS, Lukas MA, Holdbrook FK, et al. The effect of carvedilol on mortality risk in heart failure patients with diabetes: results of a meta-analysis. Curr Med Res Opin. 2006;22:287–96. doi: 10.1185/030079906X80459. [DOI] [PubMed] [Google Scholar]
- Bhagat K, Mazayi-Mupanemunda M. Compliance with medication in patients with heart failure in Zimbabwe. East Afr Med J. 2001;78:45–8. doi: 10.4314/eamj.v78i1.9112. [DOI] [PubMed] [Google Scholar]
- Bradley DJ, Bradley EA, Baughman KL, et al. Cardiac resynchronization and death from progressive heart failure: a meta-analysis of randomized controlled trials. JAMA. 2003;289:730–40. doi: 10.1001/jama.289.6.730. [DOI] [PubMed] [Google Scholar]
- Choukem SP, Kengne AP, Dehayem YM, et al. Hypertension in people with diabetes in sub-Saharan Africa: revealing the hidden face of the iceberg. Diabetes Res Clin Pract. 2007;77:293–9. doi: 10.1016/j.diabres.2006.11.007. [DOI] [PubMed] [Google Scholar]
- Commerford P, Mayosi B. An appropriate research agenda for heart disease in Africa. Lancet. 2006;367:1884–6. doi: 10.1016/S0140-6736(06)68822-3. [DOI] [PubMed] [Google Scholar]
- Danbauchi SS, Anumah FE, Alhassan MA, et al. Left ventricular function in type 2 diabetes patients without cardiac symptoms in Zaria, Nigeria. Ethn Dis. 2005;15:635–40. [PubMed] [Google Scholar]
- Factor SM, Minase T, Sonnenblick EH. Clinical and morphological features of human hypertensive-diabetic cardiomyopathy. Am Heart J. 1980;99:446–58. doi: 10.1016/0002-8703(80)90379-8. [DOI] [PubMed] [Google Scholar]
- Famuyiwa OO, Odia OJ, Osotimehin BO, et al. Non-invasive cardiac study in diabetic Nigerians using systolic time intervals. Trop Geogr Med. 1985;37:143–9. [PubMed] [Google Scholar]
- Felker GM, Milano CA, Yager JE, et al. Outcomes with an alternate list strategy for heart transplantation. J Heart Lung Transplant. 2005;24:1781–6. doi: 10.1016/j.healun.2005.03.014. [DOI] [PubMed] [Google Scholar]
- Fisman EZ, Tenenbaum A, Motro M, et al. Oral antidiabetic therapy in patients with heart disease. A cardiologic standpoint. Herz. 2004;29:290–8. doi: 10.1007/s00059-004-2476-5. [DOI] [PubMed] [Google Scholar]
- Fofana M, Toure S, Dadhi Balde M, et al. Etiologic and nosologic considerations apropos of 574 cases of cardiac decompensation in Conakry. Ann Cardiol Angeiol (Paris) 1988;37:419–24. [PubMed] [Google Scholar]
- Garty M, Shotan A, Gottlieb S, et al. The management, early and one year outcome in hospitalized patients with heart failure: a national Heart Failure Survey in Israel – HFSIS 2003. Isr Med Assoc J. 2007;9:227–33. [PubMed] [Google Scholar]
- Hofman K, Ryce A, Prudhomme W, et al. Reporting of non-communicable disease research in low- and middle-income countries: a pilot bibliometric analysis. J Med Libr Assoc. 2006;94:415–20. [PMC free article] [PubMed] [Google Scholar]
- [IDF] International Diabetes Federation. Diabetes Atlas. Brussels: IDF; 2006. [Google Scholar]
- Ikeda Y, Tenderich G, Zittermann A, et al. Heart transplantation in insulin-treated diabetic mellitus patients with diabetes-related complications. Transpl Int. 2007;20:528–33. doi: 10.1111/j.1432-2277.2007.00478.x. [DOI] [PubMed] [Google Scholar]
- Iribarren C, Karter AJ, Go AS, et al. Glycemic control and heart failure among adult patients with diabetes. Circulation. 2001;103:2668–73. doi: 10.1161/01.cir.103.22.2668. [DOI] [PubMed] [Google Scholar]
- Isezuo SA. Seasonal variation in hospitalisation for hypertension-related morbidities in Sokoto, north-western Nigeria. Int J Circumpolar Health. 2003;62:397–409. doi: 10.3402/ijch.v62i4.17583. [DOI] [PubMed] [Google Scholar]
- Jaffe AS, Spadaro JJ, Schechtman K, et al. Increased congestive heart failure after myocardial infarction of modest extent in patients with diabetes mellitus. Am Heart J. 1984;108:31–7. doi: 10.1016/0002-8703(84)90541-6. [DOI] [PubMed] [Google Scholar]
- Kannel WB, McGee DL. Diabetes and cardiovascular disease. The Framingham study. JAMA. 1979;241:2035–8. doi: 10.1001/jama.241.19.2035. [DOI] [PubMed] [Google Scholar]
- Kannel WB, McGee DL. Diabetes and cardiovascular risk factors: the Framingham study. Circulation. 1979;59:8–13. doi: 10.1161/01.cir.59.1.8. [DOI] [PubMed] [Google Scholar]
- Kengne AP, Amoah AG, Mbanya JC. Cardiovascular complications of diabetes mellitus in sub-Saharan Africa. Circulation. 2005;112:3592–601. doi: 10.1161/CIRCULATIONAHA.105.544312. [DOI] [PubMed] [Google Scholar]
- Kengne AP, Mbanya JC. Diabetes management in Africa – Challenges and opportunities. SA J Diabet Vasc Dis. 2006;3:161–7. [Google Scholar]
- Kies P, Bax JJ, Molhoek SG, et al. Comparison of effectiveness of cardiac resynchronization therapy in patients with versus without diabetes mellitus. Am J Cardiol. 2005;96:108–11. doi: 10.1016/j.amjcard.2005.02.055. [DOI] [PubMed] [Google Scholar]
- Kingue S, Dzudie A, Menanga A, et al. A new look at adult chronic heart failure in Africa in the age of the Doppler echocardiography: experience of the medicine department at Yaounde General Hospital. Ann Cardiol Angeiol (Paris) 2005;54:276–83. doi: 10.1016/j.ancard.2005.04.014. [DOI] [PubMed] [Google Scholar]
- Ladipo GO. Congestive cardiac failure in elderly Nigerians: a prospective clinical study. Trop Geogr Med. 1981;33:257–62. [PubMed] [Google Scholar]
- Lincoff AM, Wolski K, Nicholls SJ, et al. Pioglitazone and risk of cardiovascular events in patients with type 2 diabetes mellitus: a meta-analysis of randomized trials. JAMA. 2007;298:1180–8. doi: 10.1001/jama.298.10.1180. [DOI] [PubMed] [Google Scholar]
- Magula NP, Mayosi BM. Cardiac involvement in HIV-infected people living in Africa: a review. Cardiovasc J S Afr. 2003;14:231–7. [PubMed] [Google Scholar]
- Mathew V, Frye RL, Lennon R, et al. Comparison of survival after successful percutaneous coronary intervention of patients with diabetes mellitus receiving insulin versus those receiving only diet and/or oral hypoglycemic agents. Am J Cardiol. 2004;93:399–403. doi: 10.1016/j.amjcard.2003.10.031. [DOI] [PubMed] [Google Scholar]
- Mathew V, Gersh BJ, Williams BA, et al. Outcomes in patients with diabetes mellitus undergoing percutaneous coronary intervention in the current era: a report from the Prevention of REStenosis with Tranilast and its Outcomes (PRESTO) trial. Circulation. 2004;109:476–80. doi: 10.1161/01.CIR.0000109693.64957.20. [DOI] [PubMed] [Google Scholar]
- Mayosi BM. Contemporary trends in the epidemiology and management of cardiomyopathy and pericarditis in sub-Saharan Africa. Heart. 2007;93:1176–83. doi: 10.1136/hrt.2007.127746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayosi BM, Burgess LJ, Doubell AF. Tuberculous pericarditis. Circulation. 2005;112:3608–16. doi: 10.1161/CIRCULATIONAHA.105.543066. [DOI] [PubMed] [Google Scholar]
- Mbanya JC, Kengne AP, Assah F. Diabetes care in Africa. Lancet. 2006;368:1628–9. doi: 10.1016/S0140-6736(06)69673-6. [DOI] [PubMed] [Google Scholar]
- Mbanya JC, Sobngwi E, Mbanya DS, et al. Left ventricular mass and systolic function in African diabetic patients: association with microalbuminuria. Diabetes Metab. 2001;27:378–82. [PubMed] [Google Scholar]
- Mendez GF, Cowie MR. The epidemiological features of heart failure in developing countries: a review of the literature. Int J Cardiol. 2001;80:213–19. doi: 10.1016/s0167-5273(01)00497-1. [DOI] [PubMed] [Google Scholar]
- Mensah GA, Barkey NL, Cooper RS. Spectrum of hypertensive target organ damage in Africa: a review of published studies. J Hum Hypertens. 1994;8:799–808. [PubMed] [Google Scholar]
- Morgan JA, John R, Weinberg AD, et al. Heart transplantation in diabetic recipients: a decade review of 161 patients at Columbia Presbyterian. J Thorac Cardiovasc Surg. 2004;127:1486–92. doi: 10.1016/j.jtcvs.2003.11.063. [DOI] [PubMed] [Google Scholar]
- Motala AA. Diabetes trends in Africa. Diabetes Metab Res Rev. 2002;18(Suppl 3):S14–20. doi: 10.1002/dmrr.284. [DOI] [PubMed] [Google Scholar]
- Movahed MR, Hashemzadeh M, Jamal MM. Significant increase in the prevalence of non-rheumatic aortic valve disease in patients with type 2 diabetes mellitus. Exp Clin Endocrinol Diabetes. 2007;115:105–7. doi: 10.1055/s-2007-949656. [DOI] [PubMed] [Google Scholar]
- Njoh J. Complications of hypertension in adult urban Liberians. J Hum Hypertens. 1990;4:88–90. [PubMed] [Google Scholar]
- Ola BA, Adewuya AO, Ajayi OE, et al. Relationship between depression and quality of life in Nigerian outpatients with heart failure. J Psychosom Res. 2006;61:797–800. doi: 10.1016/j.jpsychores.2006.04.022. [DOI] [PubMed] [Google Scholar]
- Opie LH. Heart disease in Africa. Lancet. 2006;368:449–50. doi: 10.1016/S0140-6736(06)69149-6. [DOI] [PubMed] [Google Scholar]
- Oyoo GO, Ogola EN. Clinical and socio demographic aspects of congestive heart failure patients at Kenyatta National Hospital, Nairobi. East Afr Med J. 1999;76:23–7. [PubMed] [Google Scholar]
- Panzram G. Mortality and survival in type 2 (non-insulin-dependent) diabetes mellitus. Diabetologia. 1987;30:123–31. doi: 10.1007/BF00274216. [DOI] [PubMed] [Google Scholar]
- Rayner B, Becker P. The prevalence of microalbuminuria and ECG left ventricular hypertrophy in hypertensive patients in private practices in South Africa. Cardiovasc J S Afr. 2006;17:245–9. [PubMed] [Google Scholar]
- Roglic G, Unwin N, Bennett PH, et al. The burden of mortality attributable to diabetes: realistic estimates for the year 2000. Diabetes Care. 2005;28:2130–5. doi: 10.2337/diacare.28.9.2130. [DOI] [PubMed] [Google Scholar]
- Saba MM, Ventura HO, Saleh M, et al. Ancient Egyptian medicine and the concept of heart failure. J Card Fail. 2006;12:416–21. doi: 10.1016/j.cardfail.2006.03.001. [DOI] [PubMed] [Google Scholar]
- Singh S, Loke YK, Furberg CD. Long-term risk of cardiovascular events with rosiglitazone: a meta-analysis. JAMA. 2007;298:1189–95. doi: 10.1001/jama.298.10.1189. [DOI] [PubMed] [Google Scholar]
- Skouri HN, Wilson Tang WH. The impact of diabetes on heart failure: opportunities for intervention. Curr Heart Fail Rep. 2007;4:70–7. doi: 10.1007/s11897-007-0003-8. [DOI] [PubMed] [Google Scholar]
- Sliwa K, Damasceno A, Mayosi BM. Epidemiology and etiology of cardiomyopathy in Africa. Circulation. 2005;112:3577–83. doi: 10.1161/CIRCULATIONAHA.105.542894. [DOI] [PubMed] [Google Scholar]
- Solang L, Malmberg K, Ryden L. Diabetes mellitus and congestive heart failure. Further knowledge needed. Eur Heart J. 1999;20:789–95. doi: 10.1053/euhj.1998.1472. [DOI] [PubMed] [Google Scholar]
- Stamler J, Vaccaro O, Neaton JD, et al. Diabetes, other risk factors, and 12-yr cardiovascular mortality for men screened in the Multiple Risk Factor Intervention Trial. Diabetes Care. 1993;16:434–44. doi: 10.2337/diacare.16.2.434. [DOI] [PubMed] [Google Scholar]
- Stewart S, Wilkinson D, Becker A, et al. Mapping the emergence of heart disease in a black, urban population in Africa: the Heart of Soweto Study. Int J Cardiol. 2006;108:101–8. doi: 10.1016/j.ijcard.2006.01.001. [DOI] [PubMed] [Google Scholar]
- Steyn K, Sliwa K, Hawken S, et al. Risk factors associated with myocardial infarction in Africa: the INTERHEART Africa study. Circulation. 2005;112:3554–61. doi: 10.1161/CIRCULATIONAHA.105.563452. [DOI] [PubMed] [Google Scholar]
- Tang WH. Glycemic control and treatment patterns in patients with heart failure. Heart Fail Monit. 2006;5:10–14. [PubMed] [Google Scholar]
- Thiam M. Cardiac insufficiency in the African cardiology milieu. Bull Soc Pathol Exot. 2003;96:217–18. [PubMed] [Google Scholar]
- Toure IA, Salissou O, Chapko MK. Hospitalizations in Niger (West Africa) for complications from arterial hypertension. Am J Hypertens. 1992;5:322–4. doi: 10.1093/ajh/5.5.322. [DOI] [PubMed] [Google Scholar]
- Vermes E, Ducharme A, Bourassa MG, et al. Enalapril reduces the incidence of diabetes in patients with chronic heart failure: insight from the Studies Of Left Ventricular Dysfunction (SOLVD) Circulation. 2003;107:1291–6. doi: 10.1161/01.cir.0000054611.89228.92. [DOI] [PubMed] [Google Scholar]
- Wild S, Roglic G, Green A, et al. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27:1047–53. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- Wilson SR, Vakili BA, Sherman W, et al. Effect of diabetes on long-term mortality following contemporary percutaneous coronary intervention: analysis of 4,284 cases. Diabetes Care. 2004;27:1137–42. doi: 10.2337/diacare.27.5.1137. [DOI] [PubMed] [Google Scholar]


