Abstract
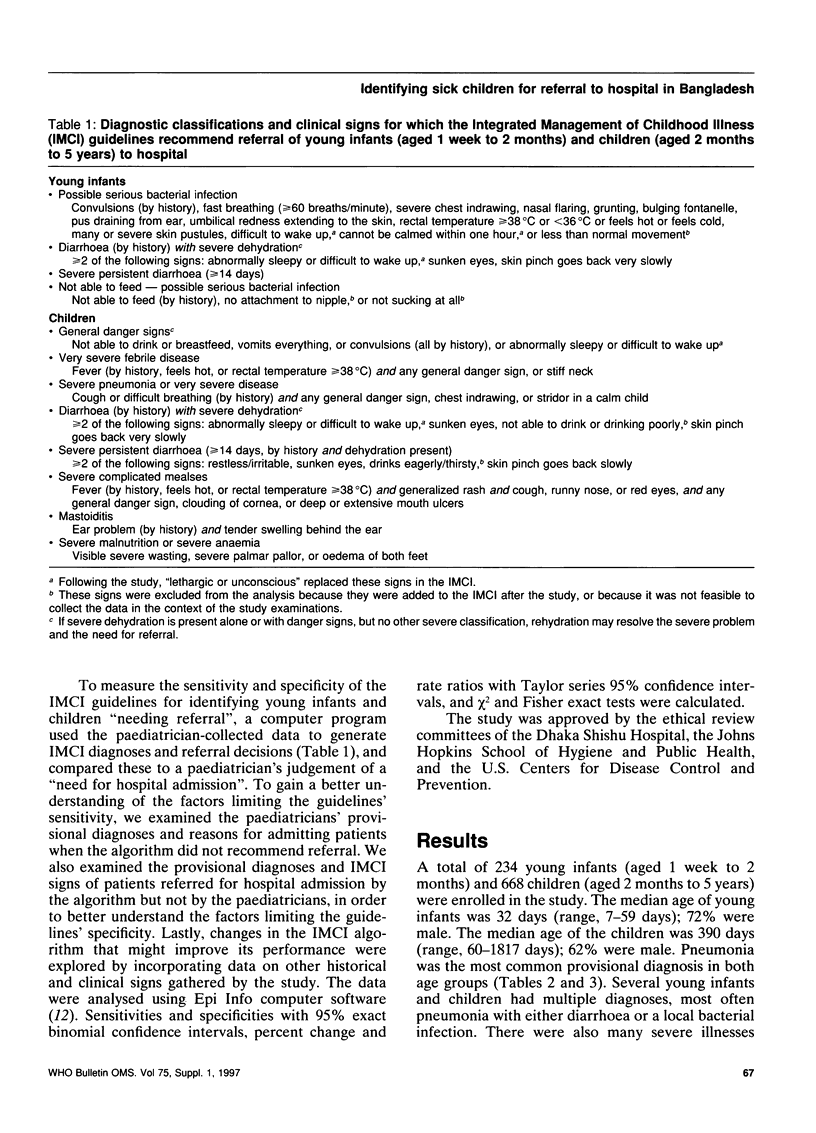
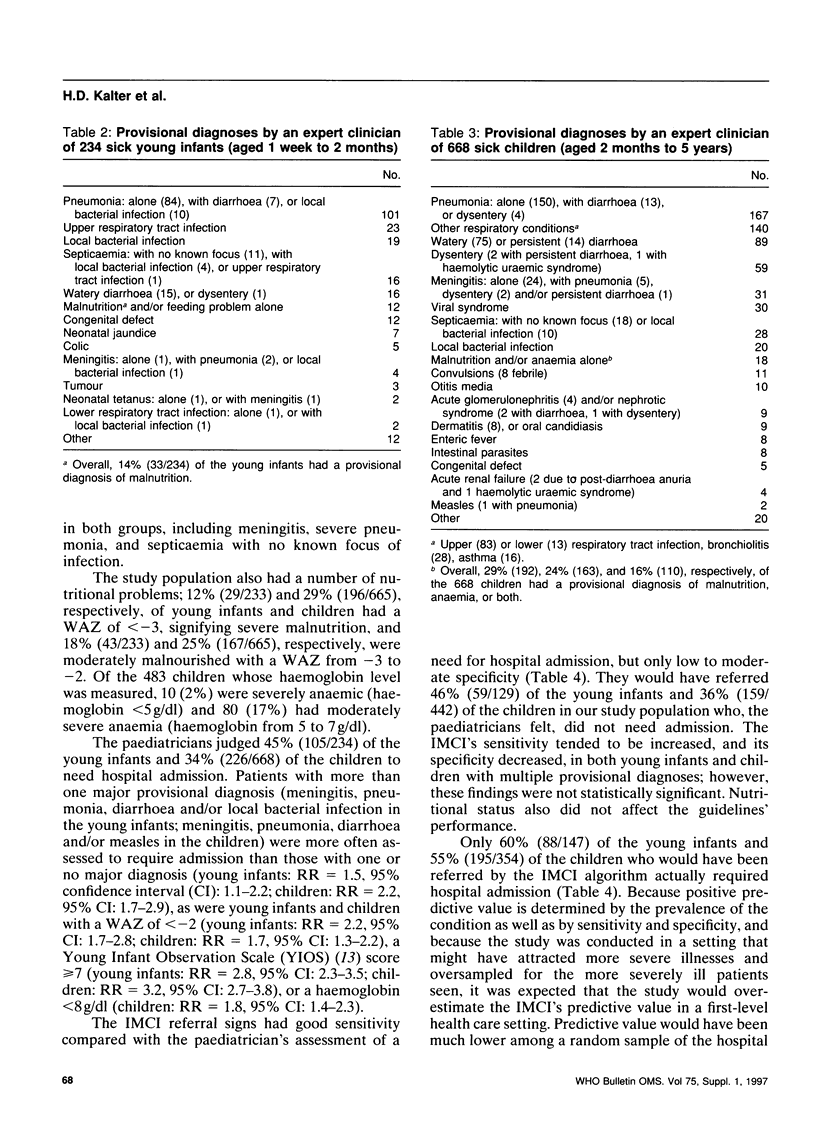
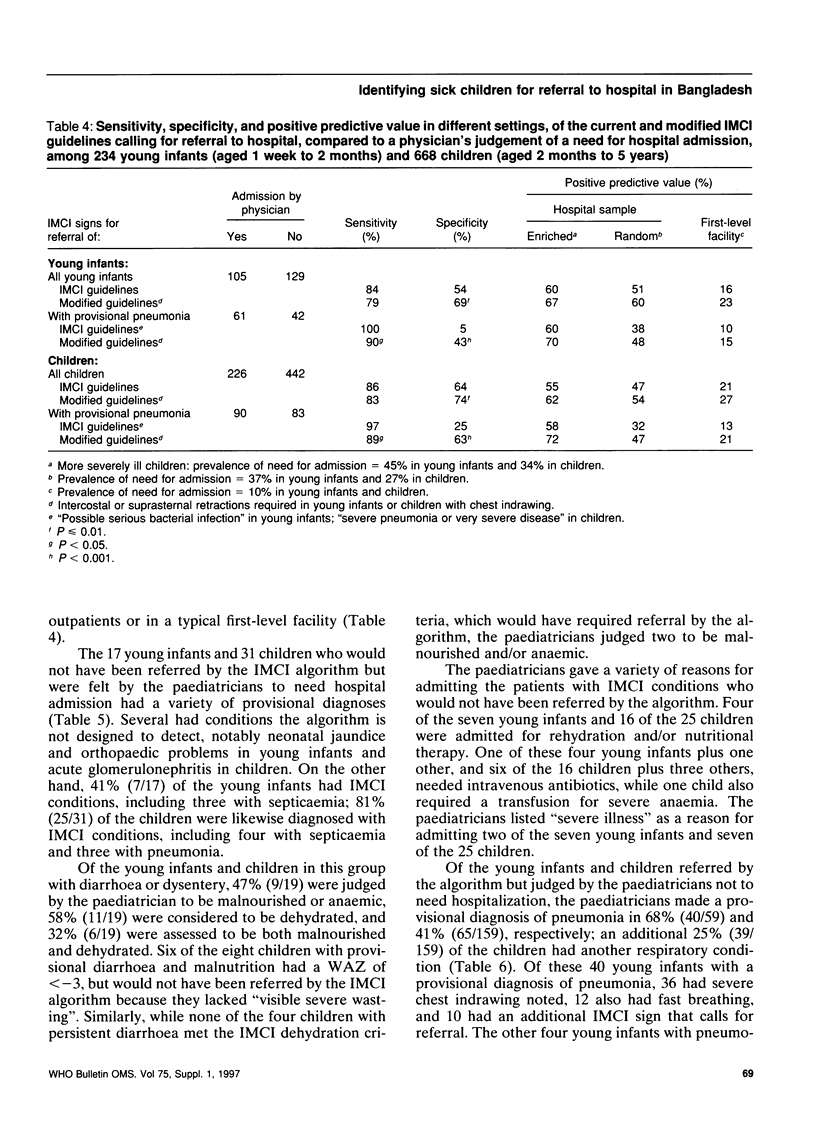
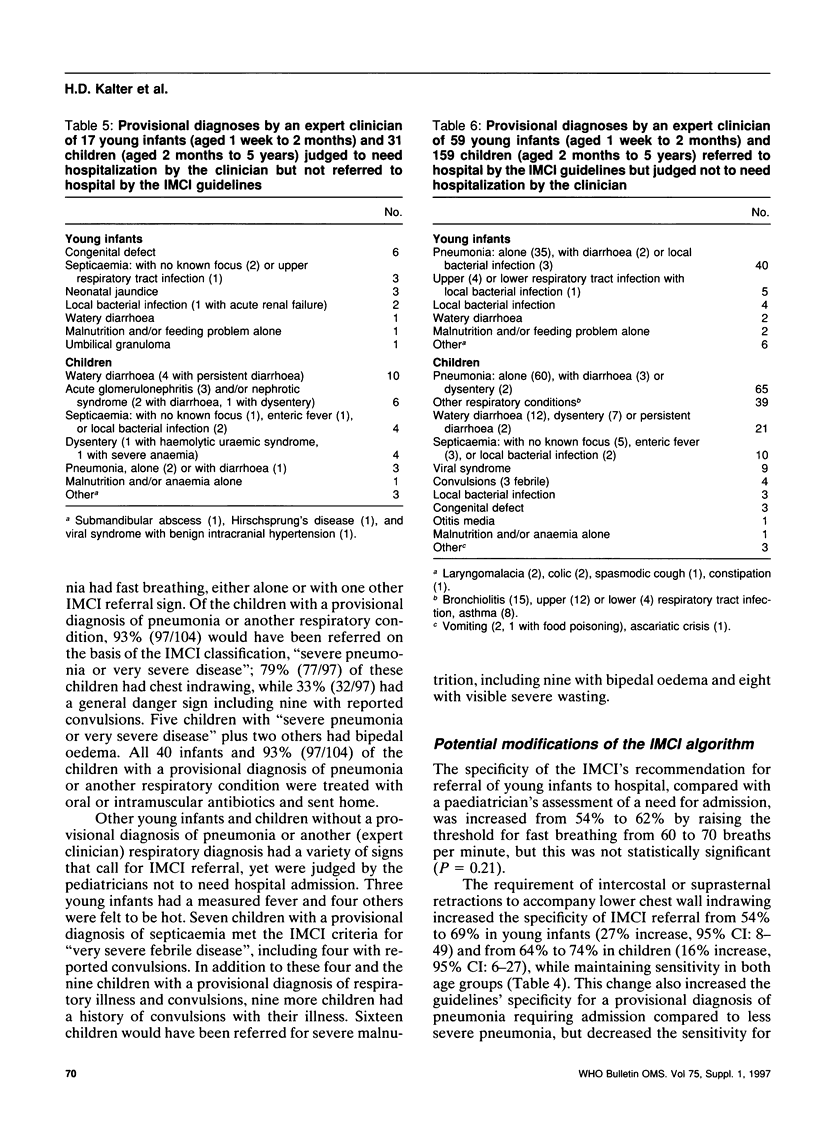
The object of this study was to evaluate and improve the guidelines for the Integrated Management of Childhood Illness (IMCI) with respect to identifying young infants and children requiring referral to hospital in an area of low malaria prevalence. A total of 234 young infants (aged 1 week to 2 months) and 668 children (aged 2 months to 5 years) were prospectively sampled from patients presenting at a children's hospital in Dhaka, Bangladesh. The study paediatricians obtained a standardized history and carried out a physical examination, including items in the IMCI guidelines developed by WHO and UNICEF. The paediatricians made a provisional diagnosis and judged whether each patient needed hospital admission. Using the paediatrician's assessment of a need for admission as the standard, the sensitivity and specificity of the current and modified IMCI guidelines for correctly referring patients to hospital were examined. The IMCI's sensitivity for a paediatrician's assessment in favour of hospital admission was 84% (95% confidence interval (CI): 75-90) for young infants and 86% (95% CI: 81-90) for children, and the specificity was, respectively, 54% (95% CI: 45-63) and 64% (95% CI: 59-69). One fourth or more in each group had a provisional diagnosis of pneumonia, and the IMCI's specificity was increased without lowering sensitivity by modifying the respiratory signs calling for referral. These results show that the IMCI has good sensitivity for correctly referring young infants and children requiring hospital admission in a developing country setting with a low prevalence of malaria. The guidelines' moderate specificity will result in considerable over-referral of patients not needing admission, thereby decreasing opportunities for successful treatment of patients at first-level health facilities. The impact of the IMCI guidelines on children's health and the health care system must be judged in the light of current treatment practices, health outcomes and referral patterns.
Full text
PDF



Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Benninger M. S., King F., Nichols R. D. Management guidelines for improvement of otolaryngology referrals from primary care physicians. Otolaryngol Head Neck Surg. 1995 Oct;113(4):446–452. doi: 10.1016/S0194-59989570083-8. [DOI] [PubMed] [Google Scholar]
- Black R. E., Brown K. H., Becker S. Malnutrition is a determining factor in diarrheal duration, but not incidence, among young children in a longitudinal study in rural Bangladesh. Am J Clin Nutr. 1984 Jan;39(1):87–94. doi: 10.1093/ajcn/39.1.87. [DOI] [PubMed] [Google Scholar]
- Bonadio W. A., Hennes H., Smith D., Ruffing R., Melzer-Lange M., Lye P., Isaacman D. Reliability of observation variables in distinguishing infectious outcome of febrile young infants. Pediatr Infect Dis J. 1993 Feb;12(2):111–114. doi: 10.1097/00006454-199302000-00001. [DOI] [PubMed] [Google Scholar]
- Campbell H., Byass P., Lamont A. C., Forgie I. M., O'Neill K. P., Lloyd-Evans N., Greenwood B. M. Assessment of clinical criteria for identification of severe acute lower respiratory tract infections in children. Lancet. 1989 Feb 11;1(8633):297–299. doi: 10.1016/s0140-6736(89)91308-1. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Mortality from congestive heart failure--United States, 1980-1990. MMWR Morb Mortal Wkly Rep. 1994 Feb 11;43(5):77–81. [PubMed] [Google Scholar]
- Charlson M. E., Sax F. L., MacKenzie C. R., Fields S. D., Braham R. L., Douglas R. G., Jr Assessing illness severity: does clinical judgment work? J Chronic Dis. 1986;39(6):439–452. doi: 10.1016/0021-9681(86)90111-6. [DOI] [PubMed] [Google Scholar]
- Cherian T., John T. J., Simoes E., Steinhoff M. C., John M. Evaluation of simple clinical signs for the diagnosis of acute lower respiratory tract infection. Lancet. 1988 Jul 16;2(8603):125–128. doi: 10.1016/s0140-6736(88)90683-6. [DOI] [PubMed] [Google Scholar]
- Fauveau V., Henry F. J., Briend A., Yunus M., Chakraborty J. Persistent diarrhea as a cause of childhood mortality in rural Bangladesh. Acta Paediatr Suppl. 1992 Sep;381:12–14. doi: 10.1111/j.1651-2227.1992.tb12365.x. [DOI] [PubMed] [Google Scholar]
- Gillam S. J. Mortality risk factors in acute protein-energy malnutrition. Trop Doct. 1989 Apr;19(2):82–85. doi: 10.1177/004947558901900214. [DOI] [PubMed] [Google Scholar]
- Griffin P. M., Ryan C. A., Nyaphisi M., Hargrett-Bean N., Waldman R. J., Blake P. A. Risk factors for fatal diarrhea: a case-control study of African children. Am J Epidemiol. 1988 Dec;128(6):1322–1329. doi: 10.1093/oxfordjournals.aje.a115085. [DOI] [PubMed] [Google Scholar]
- Howard N. J., Laing R. O. Changes in the World Health Organisation essential drug list. Lancet. 1991 Sep 21;338(8769):743–745. doi: 10.1016/0140-6736(91)91455-4. [DOI] [PubMed] [Google Scholar]
- Integrated management of the sick child. Bull World Health Organ. 1995;73(6):735–740. [PMC free article] [PubMed] [Google Scholar]
- Jelley D., Madeley R. J. Primary health care in practice: a study in Mozambique. Soc Sci Med. 1984;19(8):773–782. doi: 10.1016/0277-9536(84)90392-7. [DOI] [PubMed] [Google Scholar]
- Khanum S., Ashworth A., Huttly S. R. Controlled trial of three approaches to the treatment of severe malnutrition. Lancet. 1994 Dec 24;344(8939-8940):1728–1732. doi: 10.1016/s0140-6736(94)92885-1. [DOI] [PubMed] [Google Scholar]
- Mondal G. P., Raghavan M., Bhat B. V., Srinivasan S. Neonatal septicaemia among inborn and outborn babies in a referral hospital. Indian J Pediatr. 1991 Jul-Aug;58(4):529–533. doi: 10.1007/BF02750936. [DOI] [PubMed] [Google Scholar]
- Mulholland E. K., Simoes E. A., Costales M. O., McGrath E. J., Manalac E. M., Gove S. Standardized diagnosis of pneumonia in developing countries. Pediatr Infect Dis J. 1992 Feb;11(2):77–81. doi: 10.1097/00006454-199202000-00004. [DOI] [PubMed] [Google Scholar]
- Nicholas D. D., Heiby J. R., Hatzell T. A. The Quality Assurance Project: introducing quality improvement to primary health care in less developed countries. Qual Assur Health Care. 1991;3(3):147–165. doi: 10.1093/intqhc/3.3.147. [DOI] [PubMed] [Google Scholar]
- Pandey M. R., Daulaire N. M., Starbuck E. S., Houston R. M., McPherson K. Reduction in total under-five mortality in western Nepal through community-based antimicrobial treatment of pneumonia. Lancet. 1991 Oct 19;338(8773):993–997. doi: 10.1016/0140-6736(91)91847-n. [DOI] [PubMed] [Google Scholar]
- Pelletier D. L., Frongillo E. A., Jr, Habicht J. P. Epidemiologic evidence for a potentiating effect of malnutrition on child mortality. Am J Public Health. 1993 Aug;83(8):1130–1133. doi: 10.2105/ajph.83.8.1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sazawal S., Black R. E. Meta-analysis of intervention trials on case-management of pneumonia in community settings. Lancet. 1992 Aug 29;340(8818):528–533. doi: 10.1016/0140-6736(92)91720-s. [DOI] [PubMed] [Google Scholar]
- Shann F., Hart K., Thomas D. Acute lower respiratory tract infections in children: possible criteria for selection of patients for antibiotic therapy and hospital admission. Bull World Health Organ. 1984;62(5):749–753. [PMC free article] [PubMed] [Google Scholar]
- Stevens S. M., Richardson D. K., Gray J. E., Goldmann D. A., McCormick M. C. Estimating neonatal mortality risk: an analysis of clinicians' judgments. Pediatrics. 1994 Jun;93(6 Pt 1):945–950. [PubMed] [Google Scholar]
- von Schenck H., Falkensson M., Lundberg B. Evaluation of "HemoCue," a new device for determining hemoglobin. Clin Chem. 1986 Mar;32(3):526–529. [PubMed] [Google Scholar]


