Abstract
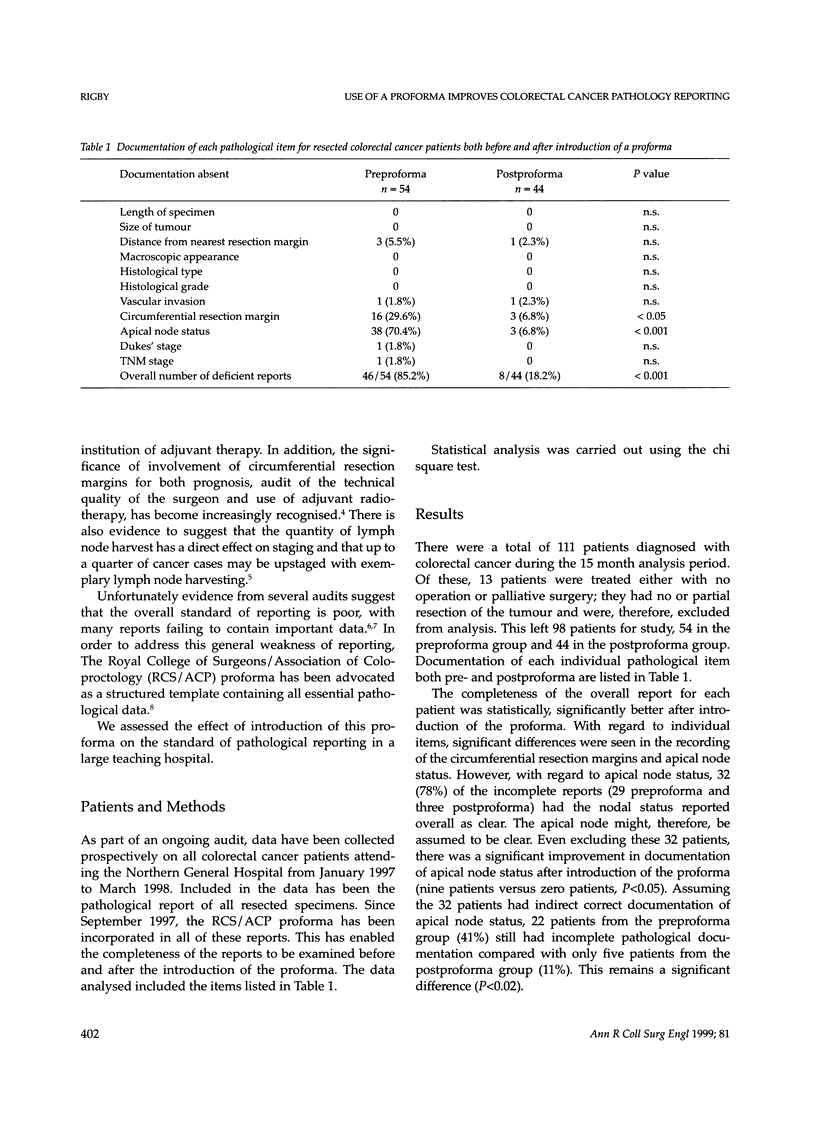
The detail and accuracy of pathological reporting for colorectal cancer is becoming increasingly recognised as important in the overall management of the patient. However, there is criticism of the variable standards of reporting. We assessed how the use of a proforma affected the completeness of reporting within one hospital. Data on all colorectal cancer patients attending one teaching hospital has been collected prospectively over a 15 month period from 1997 to 1998. The Royal College of Surgeons/Association of Coloproctology proforma lists all items considered to be essential for a complete pathological report of colorectal cancer. Its introduction in September 1997 allowed us to compare reporting before the proforma to that after. Of 54 patients, 46 (85%) had one or more items missing from their report before introduction of the proforma compared with only 8/44 (18%) patients after the proforma (P < 0.001). Circumferential resection margins and apical node status were the items most often absent, being significantly more frequently reported after the proforma (P < 0.05 and P < 0.001, respectively). There was no difference in the median number of lymph nodes harvested after proforma introduction. The introduction of the proforma has not only resulted in improvements in reporting, but has increased the dialogue between surgical oncologists and pathologists. These features should result in improved overall management of the colorectal cancer patient.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Blenkinsopp W. K., Stewart-Brown S., Blesovsky L., Kearney G., Fielding L. P. Histopathology reporting in large bowel cancer. J Clin Pathol. 1981 May;34(5):509–513. doi: 10.1136/jcp.34.5.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bull A. D., Biffin A. H., Mella J., Radcliffe A. G., Stamatakis J. D., Steele R. J., Williams G. T. Colorectal cancer pathology reporting: a regional audit. J Clin Pathol. 1997 Feb;50(2):138–142. doi: 10.1136/jcp.50.2.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fielding L. P., Stewart-Brown S., Blesovsky L., Kearney G. Anastomotic integrity after operations for large-bowel cancer: a multicentre study. Br Med J. 1980 Aug 9;281(6237):411–414. doi: 10.1136/bmj.281.6237.411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McArdle C. S., Hole D. Impact of variability among surgeons on postoperative morbidity and mortality and ultimate survival. BMJ. 1991 Jun 22;302(6791):1501–1505. doi: 10.1136/bmj.302.6791.1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips R. K., Hittinger R., Blesovsky L., Fry J. S., Fielding L. P. Local recurrence following 'curative' surgery for large bowel cancer: I. The overall picture. Br J Surg. 1984 Jan;71(1):12–16. doi: 10.1002/bjs.1800710104. [DOI] [PubMed] [Google Scholar]
- Quirke P., Durdey P., Dixon M. F., Williams N. S. Local recurrence of rectal adenocarcinoma due to inadequate surgical resection. Histopathological study of lateral tumour spread and surgical excision. Lancet. 1986 Nov 1;2(8514):996–999. doi: 10.1016/s0140-6736(86)92612-7. [DOI] [PubMed] [Google Scholar]
- Scott K. W., Grace R. H. Detection of lymph node metastases in colorectal carcinoma before and after fat clearance. Br J Surg. 1989 Nov;76(11):1165–1167. doi: 10.1002/bjs.1800761118. [DOI] [PubMed] [Google Scholar]


