Abstract
Core competencies have been used to redefine curricula across the major health professions in recent decades. In 2006, the Association of Schools of Public Health identified core competencies for the master of public health degree in graduate schools and programs of public health. We provide an overview of the model development process and a listing of 12 core domains and 119 competencies that can serve as a resource for faculty and students for enhancing the quality and accountability of graduate public health education and training. The primary vision for the initiative is the graduation of professionals who are more fully prepared for the many challenges and opportunities in public health in the forthcoming decade.
The need for change in educational practices across the health professions has been widely addressed in the literature, as well as in all 4 of the seminal Institute of Medicine reports published during the past 9 years.1–4 As a result, a resounding call for reform in health professions education, training, and professional development programs has been made in relation to curricular content, outcomes, and process review.5–9
On the basis of outcomes from related research,10,11 educators generally agree that competency- or outcomes-based education can improve individual performance, enhance communication and coordination across courses and programs, and provide an impetus for faculty development, curricular reform, and leadership in educational innovation.4 In addition, explicitly specified, action-oriented behavioral competencies can significantly enhance learning and assessment outcomes.12 Consequently, several initiatives have been launched to identify and specify competencies for graduates of educational programs in the health professions, including medicine, nursing, pharmacy, dentistry, and health management.13
Competency-based education has also begun to redefine accreditation and certification oversight activities across the health professions.14,15 In 1997, the American Council on Pharmaceutical Education adopted accreditation standards focused on 18 professional competencies. In 1999, the Accreditation Council for Graduate Medical Education and the organization of certifying boards, the American Board of Medical Specialties, endorsed 6 general competencies as the foundation for all graduate medical education. These include (1) patient education, (2) medical knowledge, (3) practice-based learning and improvement, (4) interpersonal and communication skills, (5) professionalism, and (6) systems-based practice. Currently, these competencies are being phased into educational programs across both medical schools and specialty board licensure processes.4
Other competency model deployment initiatives have been undertaken by the American Association of Colleges of Nursing and their Commission on College Nursing Education, the American Organization of Nurse Executives, the American Association of Dental Schools Commission on Dental Accreditation, the Council on Linkages between Academia and Public Health Practice, the National Center for Healthcare Leadership, and the Commission on Accreditation of Health Management Education, the last of which accredits programs in health policy and management associated with many schools of public health across the United States and Canada. A more complete listing of recent competency model development initiatives is outlined in works by Calhoun et al.13 and Garman and Johnson.16
The accreditation of graduate schools of public health and of certain graduate public health programs is overseen by the Council on Education for Public Health (CEPH). A similar trend toward a new focus on the use of competencies in the evaluation of the instructional, research, and service efforts in the graduate schools accredited by the CEPH is evidenced in the differences in the accreditation standards as amended in 2002 and again in 2005. The January 2002 Accreditation Standards for Graduate Schools of Public Health17 includes only a single reference to the concept of competencies (page 10), which was used in relation to defining learning objectives. No references were made to the terms competency or competency-based education. By contrast, in the most current CEPH standards, the June 2005 Accreditation Criteria for Schools of Public Health,18 there are more than 30 references to competencies across 6 different pages (pages 3 and 16–20) with an entirely new section (Section 2.6 on pages 15–16) specifically addressing “Required Competencies.” The 2005 section also outlines the interpretation of competencies, their relation with instructional objectives, and required documentation for the review process associated with the required competencies.
Of note in the 2005 “Required Competencies” section (page 15), competencies are defined as “what a successful learner should know and be able to do upon completion of a particular program or course of study.” As well, the newer standards specifically differentiate between “competencies” and “learning objectives,” stating that the “relationship between competencies and learning objectives (the incremental learning experiences at the course and experiential levels that lead to the development of the competencies) should be explicit.”
RESPONDING TO THE NEED FOR COMPETENCY-BASED PROFESSIONAL EDUCATION
The Association of Schools of Public Health (ASPH) initiated its Core Competency Model Development Project for the master of public health (MPH) degree in 2004 with support from the US Centers for Disease Control and Prevention. The ASPH represents the 40 accredited schools of public health in North America, with a combined faculty of more than 7500 and an annual enrollment of nearly 21 000 students.
To equip graduates for analysis and consideration of solutions to public health problems at the community, institutional, and societal levels, the MPH curriculum in graduate schools and programs of public health has traditionally been organized around 5 core disciplines: biostatistics, epidemiology, environmental health science, health policy and management, and social and behavioral sciences. Public health graduates typically concentrate in one of the core discipline areas; however, study can also be focused on particular population groups or subject areas, such as aging studies, global health, maternal and child health, mental health, or public health nutrition.
We provide an overview of the development process for the ASPH Core Competency Model for the MPH degree. Also presented are the final model; its core competency domains, including domain definitions; and each of the domain-specific competencies as guidelines for improving the quality and accountability of public health education and training. For the purpose of the modeling project, we defined the MPH core competencies as a unique set of applied knowledge, skills, and other attributes, grounded in theory and evidence, for the broad practice of public health.
MODEL DEVELOPMENT PROCESS
The project was completed over a 2-year period from 2004 to 2006 under the guidance and direction of the ASPH Education Committee in 2 separate phases: Phase 1, Discipline-Specific Competency Identification and Specification, and Phase 2, Crosscutting Competency Identification and Specification.
Parallel processes were conducted across both phases, with individual expert panels or workgroups being appointed to identify and specify the competencies for each competency domain (outlined in the process flow diagram in the appendix that is available as a supplement to the online version of this article at http://ajph.org). The chairs for the work-group, representing 14 different universities (as listed in the appendix that is available as a supplement to the online version of this article at http://ajph.org), were charged with coming to consensus on the top 8 to 10 competencies required by any MPH student upon graduation, regardless of area of specialization or intended career direction. For example, the set of competencies that emerged from the biostatistics workgroup reflected the knowledge, skills, and other attributes that any MPH graduate must possess independent of specialization in any of the other core areas or specialty tracks, such as global health, maternal and child health, and public health nutrition.
Although the workgroups varied in the methods they used to draft an initial list of universal competencies for their specific domain, all of the workgroups used nominal group technique, a modified Delphi process, to refine their draft competency lists. Three modified Delphi surveys were subsequently undertaken by each core workgroup to delineate and refine their competencies. After each survey, core members convened to discuss the results of the survey in order to distill and refine the next list of competencies. For each of the 3 survey rounds, individual workgroup respondents had the opportunity to provide input by using a “general comments” section.
Throughout the modeling activities, the workgroups maintained open communication among members and with the public health community by publishing progress results (conference call minutes and draft competency lists) on the ASPH Web site. In addition, the ASPH “Friday Letter” was used to disseminate all workgroup outcomes and each of the draft competency sets as they were identified during the survey activities. A special ASPH e-mail box was also used to track input from members and from the public health community.
Phase 1: Discipline-Specific Competencies.
In the fall of 2004, the ASPH Education Committee established the first 6 workgroups, 5 in each of the 5 core public health areas (biostatistics, environmental health sciences, epidemiology, health policy and management, and social and behavioral sciences) and 1 group devoted to public health biology. Public health biology was included in Phase-1 planning, model development, and review in recognition of existing gaps between the historical and current backgrounds of students seeking the MPH degree. Although historically the MPH curriculum had served to augment students’ medical or health science degrees, in reality, most students currently enter into masters-level degree programs without grounding in the biological bases of health and illness. The public health biology work-group was therefore established to similarly identify competencies for more fully informing both faculty and students of the relevant biological processes influencing 21st-century population-based health.
Each workgroup member was nominated by a dean or public health partner (the American Public Health Association, the Association of State and Territorial Health Officials, or the National Association of County and City Health Officials). Workgroup chairs, or co-chairs, were selected and then asked to identify, from the nominees, a group of 10 content specialists or practitioners to serve as members of the core workgroup. Additional nominees were invited to serve on discipline-specific resource task groups providing supplementary review and input on drafts. Also, other interested individuals, such as ASPH council members and faculty members from programs in public health who expressed interest in becoming involved in the process, were added to the resource groups. A total of 135 members participated in Phase 1. Ultimately, the workgroups were composed of faculty and selected leaders from both practitioner organizations and public health programs.
The individual workgroups determined their own methods and resources for their initial competency selection and development activities. The specific numbers of competencies reviewed during each of the 3 Delphi surveys during Phase 1, as well as the reviewer response rate from the respective workgroup, are listed in Table 1 ▶. The average response rate was 91% during Phase 1.
TABLE 1—
Summary of Discipline-Specific and Crosscutting Delphi Processes
| Delphi 1 | Delphi 2 | Delphi 3 | Final List | |||||
| Competency Domains | No. of Competencies | Response Rate, % | No. of Competencies | Response Rate, % | No. of Competencies | Response Rate, % | No. of Discipline-Specific Competencies | No. of Crosscutting Competencies |
| Social and Behavioral Sciences | 41 | 81 | 21 | 89 | 11 | 72 | 10 | 10 |
| Biostatistics | 30 | 81 | 14 | 94 | 9 | 100 | 10 | 0 |
| Environmental Health | 17 | 100 | 14 | 100 | 9 | 100 | 8 | 0 |
| Epidemiology | 24 | 100 | 15 | 92 | 11 | 81 | 10 | 2 |
| Health and Policy Management | 46 | 90 | 50 | 92 | 13 | 100 | 10 | 2 |
| Public Health Biology | 55 | 81 | 16 | 81 | 10 | 100 | 10 | 1 |
| Total | . . . | . . . | . . . | . . . | . . . | . . . | 58 | 15 |
| Communication and Informatics | 76 | 92 | 18 | 90 | 11 | 77 | . . . | 10 |
| Diversity and Culture | 65 | 82 | 21 | 65 | 10 | 100 | . . . | 10 |
| Leadership | 60 | 91 | 31 | 86 | 12 | 66 | . . . | 9 |
| Professionalism | 41 | 100 | 25 | 77 | 14 | 80 | . . . | 11 |
| Program Planning | 52 | 100 | 28 | 66 | 13 | 75 | . . . | 10 |
| Systems Thinking | 58 | 100 | 32 | 76 | 14 | 100 | . . . | 11 |
| Total | . . . | . . . | . . . | . . . | . . . | . . . | . . . | 61 |
| Total of Phase 1 and 2 | . . . | . . . | . . . | . . . | . . . | . . . | . . . | 119 |
After each of the 10 workgroups had separately distilled a core set of MPH competencies in their respective discipline, a Core Competency Council was established that comprised the chairs of each of the work-groups and 2 practitioners, who were also drawn from the workgroups. This collective council was charged with integrating the disparate sets from the 10 independent workgroups into an overarching model reflecting the full range of knowledge, skills, and other attributes required for current and future public health practice, including both discipline-specific domains and essential interdisciplinary, crosscutting competency domains for graduate public health education and training. Using expert panel identification and consensus-building processes, the council initially identified the following 9 interdisciplinary domains: (1) communication, (2) data analysis and information management, (3) diversity and cultural proficiency, (4) ecological determinants of health, (5) leadership, (6) management and policy, (7) professionalism, (8) program planning and assessment, and (9) systems thinking.
In line with the 8 to 10 competencies identified for the discipline-specific domains, members of the council also drafted an initial set of concepts and illustrative competencies and subcompetencies for the first set of crosscutting competencies, as well as definitions for each of the domains. This first round of interdisciplinary domain concept formation was supplemented with competencies identified by the Phase-1 workgroups, with suggestions that had been previously submitted to the council, and by the literature, including prior competency specification initiatives such as those guided by the Institute of Medicine and the Council on Linkages. This draft set was subsequently reviewed by the council once again via a modified Delphi process and was then presented to the Education Committee in May of 2005 as model version 1.0. On the basis of comments from the meeting participants and the Education Committee, the 9 crosscutting domains were ultimately revised and consolidated into the following 6 domains for subsequent Phase-2 specification and refinement: (1) communication, (2) diversity and cultural proficiency, (3) leadership, (4) professionalism and ethics, (5) program planning and assessment, and (6) systems thinking.
Three of the 9 interdisciplinary domains, data analysis and information management, ecological determinants of health, and management and policy, were re-integrated into the preexisting discipline-specific competency areas for additional review and vetting during Phase 1 of model development.
Subsequent iterations of the proposed model version 1.1 (completed on June 17, 2005) and version 1.2 (finalized on July 15 after review and input by the associate deans of schools of public health at their annual meeting) were both disseminated widely for comments. Version 1.2 was also presented to the ASPH deans at their retreat on July 21 for final revisions and approval. Version 1.3, which was limited to the discipline-specific competencies in the 5 basic public health science areas, was finalized on November 23 and was approved by the ASPH Education Committee on November 29. Version 1.3, with 48 competencies in 5 discipline-specific domains, was then approved by the ASPH board of directors on December 12, 2005.
Phase 2: Crosscutting Competencies.
Phase 2 of the ASPH Core Competency Model Development Project was launched in the Fall of 2005 with the formation of 6 new work-groups to further identify and refine competencies for the remaining 6 crosscutting domains. All ASPH member schools, the Association of Prevention Teaching and Research, and practitioner organizations (the American Public Health Association, the Association of State and Territorial Health Officials, and the National Association of County and City Health Officials) were invited to nominate representatives to the crosscutting domain workgroups. Also, on the basis of input from the deans of schools of public health and the ASPH Education Committee, the public health biology workgroup was revitalized with new nominations from member schools and both academic and practice partners. This group was charged with identifying additional illustrative public health biology subcompetencies that would provide more guidance to faculty and students in this area. A total of 197 members participated in the 7 workgroups formed in Phase 2.
As with the discipline-specific competency modeling process, each workgroup came to consensus on the top 8 to 10 competencies in the 6 crosscutting domains required by any MPH student, again regardless of area of specialization or intended career trajectory upon graduation. Each of the 6 crosscutting domains were prepopulated with 5 to 8 competencies on the basis of suggestions from the preliminary work of the 6 discipline-specific workgroups and the first Core Competency Council, as well as from a review of the related literature. During Phase 2, the work-groups also finalized the following domain constructs, as well as the definition of each: (1) communication and informatics, (2) diversity and culture, (3) leadership, (4) professionalism, (5) program planning, (6) public health biology, and (7) systems thinking.
As the Phase-2 processes evolved, the communication workgroup members decided to include informatics in their domain title and definition because a considerable number of informatics competencies for all MPH graduates emerged during their discussions and survey activities. Consequently, a small subgroup on informatics worked under the direction of the communication workgroup.
The specific numbers of competencies reviewed during each of the 3 rounds of Phase-2 modified-Delphi surveys, as well as the reviewer response rate from the respective workgroup, are listed in Table 1 ▶. The average response rate for the surveys was 85% in Phase 2. Similar to Phase 1, members convened in a second Core Competency Council meeting for Phase 2 in March 2006. This meeting included chairs of the 6 crosscutting areas, a public health biology chair, a practice partner, a representative from the Association of Prevention Teaching and Research, and a Phase-1 chair. The group discussed the rationale for each of the interdisciplinary domains and finalized the complete competency model. During this meeting, public health biology was designated as a crosscutting domain.
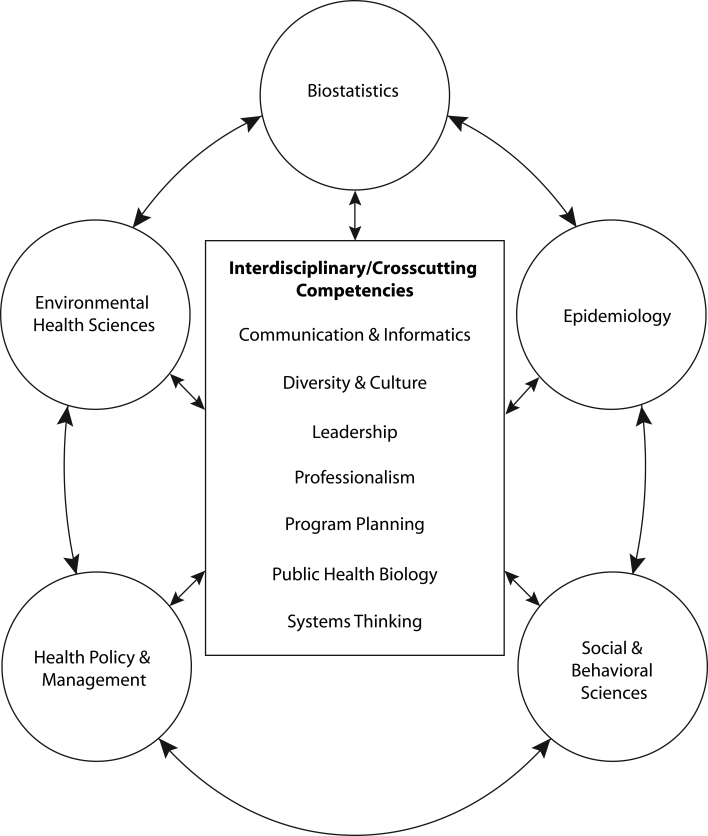
The ASPH Education Committee reviewed the Phase-2 version 2.0 of the model in April 2006, which was also presented to ASPH members and partners in May 2006. Version 2.1 was subsequently presented to the associate deans at their summer retreat in June; and version 2.2 was reviewed and approved by the ASPH deans at their retreat in July. The ASPH board accepted version 2.2 with minor revisions, which were reflected in the final ASPH Core Competency Model for the MPH degree, version 2.3, released in August 2006. The full ASPH MPH Core Competency Model is graphically depicted in Figure 1 ▶. The definitions and competencies for each of the 12 domains comprising the ASPH Core Competency Model are further outlined in Box 1. The definitions were developed to provide the context by which the workgroups’ competency modeling activities took place, versus describing the entire field of a particular discipline’s scholarship and practice. A total of 119 competencies are included in the final 2.3 version of the model.
FIGURE 1—
Association of Schools of Public Health Core Competency Model for the MPH Degree
DISCUSSION AND SUMMARY
In total, more than 400 individuals directly contributed to or provided input to the development of the final ASPH Core Competency Model, version 2.3, that was released in August 2006. The model development process was a comprehensive, grassroots, expert panel effort with ongoing field-wide dissemination and calls for input by interested parties, including faculty, public health partners, practitioners, and students. The limitations and constraints associated with expert panel and Delphi survey technique are well recognized by the ASPH Education Committee. However, given the diversity of the field and the many career paths and work settings for graduates with the MPH, the initiative provides the first national consensus-building model for continued review, development, and refinement. In addition, the model represents an integration of the core competencies for both the core disciplines and the integrative, crosscutting competencies in the field of academic public health practice.
The ASPH has disseminated the competencies to a wide audience beyond its member schools. In particular, we anticipate that the competencies will be useful to graduate public health programs, employers, practice and agency partners, CEPH, and the National Board of Public Health Examiners. Through this process, the ASPH sought to provide direction and specification regarding essential educational outcomes for the MPH core curriculum and to provide leadership in defining contemporary and future education in public health graduate education. The model also serves as a basis for launching individual initiatives associated with the many career pathways and professional employment positions that make up the field of public health.
A comprehensive overview of the ASPH MPH core competency modeling process, the complete listing of all the competencies considered by the workgroups during the model development process, and a list of resources that were used in support of the development of the Core Competency Model are available on the Internet.19–21
The Core Competency Model, version 2.3, is considered the ASPH’s best effort to date in defining the core competencies for the MPH degree. However, competency model development is an iterative process, and the model will have to be regularly updated on the basis of faculty deployment of the competencies, continued dialogue regarding the use of the competencies, input on the currency and relevancy of the competency set, and ongoing changes and progress in the field of public health. Competency sets generally have a lifespan of 3 to 5 years, and it will soon be time to revisit the set and initiate new activities for further refinement and updating in line with new thinking and future challenges to the field. The model will not remain static.
The competencies are intended to serve as a resource and guide for those interested in improving the quality and accountability of public health education and training. They were developed with respect for the uniqueness and diversity of the schools of public health. Therefore, the model may be of assistance to schools of public health in identifying specific subcompetencies and specialty competencies that apply to individual schools and unique program missions. The competencies are not meant to prescribe the methods or processes for achievement; implementation of the competencies may vary as a function of each school’s mission and goals.
As well, the ASPH Core Competency Model was not designed to serve as a framework for certain required core courses or for one-to-one development of a core curriculum, but instead is aimed at providing a baseline overview of the knowledge, skills, and other attributes expected of emerging public health professionals. The competencies are anticipated to serve as a useful guide for faculty to include, as appropriate, relevant content in their existing courses and as an aid to MPH students seeking opportunities to comprehensively update their understanding and skill sets. The primary vision for the ASPH competency model development initiative is the graduation of professionals more fully prepared for the many challenges and opportunities in public health in the forthcoming decade.
Association of Schools of Public Health Core Competencies for the Master of Publich Health Degree, by Competency Domain.
| BIOSTATISTICS | ENVIRONMENTAL HEALTH SCIENCES | EPIDEMIOLOGY |
The development and application of statistical reasoning and methods in addressing, analyzing, and solving problems in public health–, health care–, and biomedical-, clinical-, and population-based research.
|
The study of environmental factors, including biological, physical, and chemical factors that affect the health of a community.
|
The study of patterns of disease and injury in human populations and the application of this study to the control of health problems.
|
| HEALTH POLICY AND MANAGEMENT | SOCIAL AND BEHAVIORAL SCIENCES | COMMUNICATION AND INFORMATICS |
A multidisciplinary field of inquiry and practice concerned with the delivery, quality, and costs of health care for individuals and populations. This definition assumes both a managerial and a policy concern with the structure, process, and outcomes of health services including the costs, financing, organization, outcomes, and accessibility of care.
|
The study of behavioral, social, and cultural factors related to individual and population health and health disparities over the life course. Research and practice in this area contributes to the development, administration, and evaluation of programs and policies in public health and health services to promote and sustain healthy environments and healthy lives for individuals and populations.
|
The ability to collect, manage, and organize data to produce information and meaning that is exchanged by use of signs and symbols; to gather, process, and present information to different audiences in-person, through information technologies, or through media channels; and to strategically design the information and knowledge exchange process to achieve specific objectives.
|
| DIVERSITY AND CULTURE | LEADERSHIP | PUBLIC HEALTH BIOLOGYa |
The ability to interact with diverse individuals and communities to produce or impact an intended public health outcome.
|
The ability to create and communicate a shared vision for a changing future, champion solutions to organizational and community challenges, and energize commitment to goals.
|
The ability to incorporate public health biology—the biological and molecular context of public health—into public health practice.
|
| PROFESSIONALISM | PROGRAM PLANNING | SYSTEMS THINKING |
The ability to demonstrate ethical choices, values and professional practices implicit in public health decisions; consider the effect of choices on community stewardship, equity, social justice, and accountability; and commit to personal and institutional development.
|
The ability to plan for the design, development, implementation, and evaluation of strategies to improve individual and community health.
|
The ability to recognize system-level properties that result from dynamic interactions among human and social systems and how they affect the relations among individuals, groups, organizations, communities, and environments.
|
aPublic health biology illustrative sub-competencies are available at http://www.asph.org/document.cfm?page=928.
Acknowledgments
This project was supported by the Centers for Disease Control and Prevention (grant U36/CCU300430-23/24).
Special recognition and appreciation is extended to the chairpersons of each of the competency domain workgroups, as listed in the appendix that is available as a supplement to the online version of this article at http://ajph.org, for their ongoing leadership and contributions throughout the ASPH Master of Public Health degree competency model development initiative. In addition, appreciation is extended to all of the individuals who served on each of the workgroups and provided advice and counsel for final model completion. A complete listing of all workgroup members can be found on the ASPH Web site at http://www.asph.org/userfiles/Version2.3.pdf.
Note. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention.
Human Participant Protection All participants were national academic and practitioner leaders serving as voluntary members of work-groups and task forces for the purpose of providing advice and counsel, as well as their opinions for the study. They were fully informed of all of the methods both verbally and in writing. For each Delphi opinion survey round, they had the option to participate or not. Data were collected anonymously and were reported on a cohort basis only. No protocol approval was needed for this study.
Peer Reviewed
Contributors J. G. Calhoun conducted the research and provided the methodologic direction for the study, consulted with and advised the Association of Schools of Public Health (ASPH) on all aspects of the study and was the main developer of the article. K. Ramiah provided research, communications, and logistical support and coordinated all aspects of the project. E. McGean Weist managed the project and oversaw the submission of all study deliverables. S. M. Shortell helped to provide overall direction for the study and reviewed the article.
References
- 1.Committee on the Quality of Health Care in America. To Err is Human: Building a Safer Healthcare System. Washington, DC: Institute of Medicine; 1999.
- 2.Committee on the Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: Institute of Medicine; 2001.
- 3.Committee on Assessing the Health of the Public in the 21st Century. The Future of the Public’s Health in the 21st Century. Washington, DC: Institute of Medicine; 2002.
- 4.Committee on the Health Professions Education Summit. Health Professions Education: A Bridge to Quality. Washington, DC: Institute of Medicine; 2005.
- 5.Health Professions Education for the Future: Schools in Service to the Nation. San Francisco, CA: Pew Health Professions Commission; 1993.
- 6.Davis D, O’Brien MA, Freemantle N, Wolf FM, Mazmanian P, Taylor-Vaisey A. Impact of formal continuing medical education: do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes? JAMA. 1999;282:867–874. [DOI] [PubMed] [Google Scholar]
- 7.Halpern JM, Lee Y, Boulter PR, Phillips RR. A synthesis of 9 reports on physicians competencies for the emerging practice environment. Acad Med. 2001; 76:606–615. [DOI] [PubMed] [Google Scholar]
- 8.Wenzel F, Grady R, Freeman T. The health services delivery environment. J Health Adm Educ. 1995; 13:611–630. [PubMed] [Google Scholar]
- 9.Schweikart S. Reengineering the work of care-givers; role redefinition, team structures, and organizational redesign. Hosp Health Serv Adm. 1996;41: 19–36. [PubMed] [Google Scholar]
- 10.Lucia AD, Lepsinger R. The Art and Science of Competency Models: Pinpointing Critical Success Factors in Organizations. San Francisco, CA: Jossey-Bass/Pfeiffer; 1999.
- 11.Westera W. Competencies in education: a confusion of tongues. J Curriculum Stud. 2001;33:75–88. [Google Scholar]
- 12.Harden RM. Developments in outcome-based education. Med Teach. 2002;24:117–120. [DOI] [PubMed] [Google Scholar]
- 13.Calhoun JG, Davidson PL, Sinioris ME, Vincent ET, Griffith JR. Toward an understanding of competency identification and assessment in health care. Qual Manag Health Care. 2002;11(1)14–39. [DOI] [PubMed] [Google Scholar]
- 14.Annas GJ, Glantz LH, Scotch NA. Back to the future: the IOM report reconsidered. Am J Public Health. 1991;81:835–837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shortell SM, Weist EM, Mah-Sere KS, Foster A. Implementing the Institute of Medicine’s recommended curriculum content in schools of public health: a baseline assessment. Am J Public Health. 2004;94:10, 1671–1674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Garman AN, Johnson MP. Leadership competencies: an introduction. J Healthc Manag. 2006;51:1, 13–17. [PubMed] [Google Scholar]
- 17.Accreditation Standards for Graduate Schools of Public Health. Washington, DC: Council on Education for Public Health; 2002.
- 18.Accreditation Criteria for Schools of Public Health. Washington, DC: Council on Education for Public Health; 2005. Available at: http://www.ceph.org. Accessed May 19, 2008.
- 19.Master’s Degree in Public Health Core Competency Development Project Report, version 2.3, October 2004–August 2006. Association of Schools of Public Health, August 11, 2006. Available at: http://www.asph.org/userfiles/Version2.3.pdf (PDF file). Accessed May 19, 2008.
- 20.Competencies Considered for the ASPH Graduate Education Competency Model. Association of Schools of Public Health. Available at: http://www.asph.org/UserFiles/ALLCOMPSLIST.doc. Accessed May 19, 2008.
- 21.Competency Resources. Association of Schools of Public Health. Available at: http://www.asph.org/document.cfm?page=935. Accessed May 19, 2008.