Abstract
Background. We intend to give an overview of our experiences with the implementation of a new dissection technique in open and laparoscopic surgery. Methods. Our database comprises a total of 950 patients who underwent liver resection. Three hundred and fifty of them were performed exceptionally with the water-jet dissector. Forty-one laparoscopic partial liver resections were accomplished. Results. Using the water-jet dissection technique it was possible to reduce the blood loss, the Pringle- and resection time in comparison to CUSA® and blunt dissection. In the last five years we could reduce the Pringle-rate from 48 to 6% and the last 110 liver resections were performed without any Pringle's manoeuvre. At the same time, the transfusion-rate decreased from 1.86 to 0.46 EC/patient. In oncological resections, the used dissection technique had no influence on long-time survival. Conclusions. The water-jet dissection technique is fast, feasible, oncologically safe and can be used in open and in laparoscopic liver surgery.
Keywords: water-jet, hydro-jet, dissection technique, liver resection, hemihepatectomy, open and laparoscopic surgery
Introduction
Principles of dissection
The liver consists of a three-dimensional network of afferent and efferent duct- and vessel systems. Because of the higher content of collagen and elastin, these duct- and vessel systems differ essentially in their structure and resistance from the liver parenchyma. The bile ducts are more resistant in their structure compared to arteries, portal vein branches and hepatic veins.
Because of their task to collect the blood from the liver lobules, the wall of the hepatic veins is especially thin and vulnerable. Due to these physical properties it is possible to release and dissect the duct- and vessel systems mechanically from the liver parenchyma.
The dissection modalities which take advantage of the anatomic conditions are called selective. The water-jet effects hereby like an intelligent knife and separates the more resistant duct- and vessel structures automatically from the parenchyma which thus become visible. When visible they can be closed easily under controlled conditions.
An indicator of the selectivity would be the quantity of the isolated duct structures per dissection plane which is a value difficult to specify however. The water-jet, the ultrasonic aspirator (CUSA®) and the blunt dissection can be categorised under selective dissection techniques. Non-selective techniques cannot discriminate between duct structures and parenchyma. To mention are finger fracture and mechanical instruments as the scalpel, the scissors and with reservation the linear stapler as well as thermal instruments as the high-frequency electrocoagulator, the laser, the bipolar forceps or the scissors of the UltraCision® 1,2,3,4,5.
Historical development of water-jet dissection technique
Cutting with a high pressure water-jet was a development which was primarily used in the industrial technique. At pressure levels about 20,000 bar the water beam reaches supersonic speed at the tip of the nozzle, which enables effortless cutting of wood- and even steel plates without development of heat.
For application in surgery, the nozzle tip- and pressure parameters had to be adjusted to the structural properties of parenchymal organs. The first developments were made by Papachristou and Bengmark 6,7, who implemented this technology in experimental and clinical investigations. Simultaneously our working group refined this technique by means of the results of in vitro and in vivo trials and introduced it after improvement 1990 into clinical routine in liver surgery. In experimental examinations we found out that a pressure of 30–40 bar and a nozzle diameter of 0.1 mm is very effective to dissect normal liver tissue. In case of cirrhotic liver parenchyma the pressure needed for dissection is 10 bar higher. Above these parameters the quality of dissection gets worse and the rate of vessel injuries, especially of the hepatic veins, increases, which corresponds to a higher blood loss 8.
Despite the positive clinical experiences it took another six years until the first commercial devices were available. Meanwhile only in Europe more than 30 medical centres who deal with hepato-biliary surgery use the water-jet.
Pulsed jet
In the first experimental researches, a water-jet impulse was used which was generated by means of a holmium laser with a wavelength of 2.1 µm. The absorbed holmium laser energy in water causes a water-jet impulse. The impulse rate of the holmium laser and therefore also of the water-jet amounts to 8 Hz, the energy per impulse is 1 Joule. Experimental investigations of in vivo showed a comparable parenchyma dissection to continuous water-jetting. The jet impulse, however, swirled droplets of blood which could not be removed adequately even by integrating a suction system. Through this the visibility conditions of the operating field deteriorated sharply 9.
The principle of this pulsed technique was picked up again with a higher pulse frequency of 15–20 Hz in a mechanical pulse system (Saphir Medical Products GmbH). This time, the suction system was adapted to the impulse rate to avoid permanent suction. The essential advantages of this proceeding lie in the laparoscopy because the lenses stay clean and a constant pneumoperitoneum can be maintained. Both techniques could not achieve clinical relevance.
Materials and methods
Water-jet
In open surgery the water-jet was used with a nozzle diameter of 0.1 mm and a pressure of 30–40 bar. Up to now we used five different types of water-jet dissectors which were continuously improved regarding handpieces and practicability. The latest model is depicted in Figure 1. As jet liquid we used physiological sodium solution. For a hemihepatectomy we usually need about 400 mls jet-solution.
Figure 1. .
Water-jet dissector (Helix Hydro-Jet®; Erbe Elektromedizin GmbH, Tuebingen, Germany).
In laparoscopic surgery the water-jet was applied through angularly adjustable handpieces and lately the nozzle tip was connected to a high-frequency device.
As standard procedure in open surgery we accomplish a meticulous preparation of the hilar vessels and the hepatic veins prior to parenchyma dissection. The right hemiliver is completely mobilised from the diaphragma and then an intraoperative ultrasound is performed to detect the localisation of the tumour and its proximity to the vascular structures.
Intraoperative blood loss during the dissection causes the need of the Pringle's manoeuvre. Our intention was always to keep both to a minimum. During dissection we practice a well organised work-sharing between dissecting, clipping of the dissected vessels and finally cutting them in between the clips.
Results
In order to take into account the extent of resection, blood loss, resection time and Pringle-time were referred to the intraoperatively measured resection plane. The blood loss per resection plane with the water-jet was with 10.57±15.35 ml/cm2 significantly lower compared to the CUSA® with 18.26±30.13 ml/cm2 and to blunt dissection, which came off worst with 72.72±497.26 ml/cm2. This is also validated by the need of blood transfusion, which was only half as high in the water-jet group with 0.012±0.06 EC/cm2 as in the CUSA® group with 0.024 ±0.054 EC/cm2 or in the blunt dissection group with 0.095±0.806 EC/cm2. These differences were statistically significant in the Kruskal–Wallis test (p=0.002).
In clinical practice the water-jet technique proves to be considerably faster. This can also be verified by the calculation of the resection time in relation to the resection plane. With 0.29±0.67 min/cm2 this technique is significantly faster in comparison with the CUSA® with 0.48±0.85 min/cm2 and the blunt dissection with 0.77±1.75 min/cm2 (p=0.043). This was also confirmed by the comparison of the Pringle-time per resection plane, which makes up less than half with 0.13±0.18 min/cm2 by using the water-jet. The corresponding values were 0.29±0.47 min/cm2 for the CUSA® and 0.23±0.56 min/cm2 for blunt dissection.
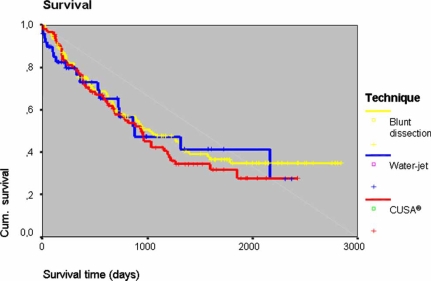
To control whether the dissection technique has influence on the prognosis, 340 patients with liver metastases were analysed according to the applied dissection technique. It is to mention, that with the CUSA® – and the water-jet technique mostly extended liver resections were performed. Nevertheless there were no differences in the Kaplan-Meier analysis (Figure 2). Another Kaplan-Meier analysis was carried out in 87 patients with hepatocellular carcinoma which did not reveal significant differences likewise.
Figure 2. .
Kaplan-Meier survival curves after resection of liver metastases (n=340).
The postoperative complications do not distinguish between the different groups regarding the number of postoperative bile fistulae and subhepatic abscesses (Table I). The postoperative liver dysfunction especially liver failure was not dependent on the performed dissection technique but rather the consequence of the extent of resection and the functional reserve of the remnant liver.
Table I. Postoperative complications after liver resection.
| Biliary complications |
Abscess |
Liver dysfunction |
Lethality |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Technique | Number of operations | n | % | n | % | n | % | n | % |
| Water-jet | 137 | 7 | 5.1 | 4 | 2.9 | 11 | 8 | 5 | 3.6 |
| CUSA® | 175 | 11 | 6.3 | 11 | 6.3 | 22 | 12.5 | 6 | 3.4 |
| Blunt dissection | 279 | 15 | 5.3 | 10 | 3.5 | 27 | 9.8 | 8 | 2.8 |
In the period from 1991 to 2007 we could reduce the rate of application of the Pringle's manoeuvre from 46 to 6%. Additionally, the loss of blood and the amount of erythrocyte concentrates (EC) per patient could be decreased (Table II). This table also documents the effect of the learning curve of the surgical team.
Table II. The development of operation parameters in liver resection using the water-jet over the course of 16 years.
| 1991–1996 | 1997–2002 | 2003–2007 | |
|---|---|---|---|
| N | 96 | 120 | 134 |
| Pringle-rate (%) | 46 | 48 | 6 |
| Operating time (min) | 214 | 294 | 181 |
| Blood loss (ml) | 1442.6 | 1337.9 | 523.7 |
| EC per patient | 1.86 | 0.71 | 0.46 |
Overall 350 partial liver resections were performed using the water-jet technique. Since 2002 we use this technique exceptionally. The last 110 liver resections have been performed without any Pringle's manoeuvre.
In the group of laparoscopic liver resections were two conversions to open surgery. In a patient with a hydatid cyst, the arterial pCO2 increased with insufflation of CO2 and intraabdominal gas pressure had to be reduced. Visualisation of minor venous bleeding was thereupon not satisfactory and conversation was necessary for safety reasons. This patient developed a bile fistula and pneumonia postoperatively and was hospitalised for a total of 39 days. Another conversion had to be done because of major portal venous bleeding.
Discussion
By reason of the positive results when using the water-jet in meanwhile 350 liver resections we implemented this technique as our standard dissection procedure.
The reduction of blood loss and application of the Pringle's manoeuvre is not only a question of the dissection technique but also a result of the surgical team's learning curve.
Given that no blood is transferred in 80% of all liver resections, we also do not use a Cell-Saver anymore. Finally in our experience the water-jet is superior to blunt dissection and CUSA® regarding blood loss, dissection- and Pringle-time.
New and promising methods such as the UltraCision® technology or the LigaSure™ as well as the bipolar scissors can be effectively used in the surface area of the liver. Here, a good hemostasis can be achieved. However, they are less efficient in the depth of the parenchyma because especially the thin-walled liver veins cannot be closed and therefore difficult bleedings arise. As these bleedings are of venous origin, unfortunately, the Pringle's manoeuvre is less effective. In order to minimise venous bleedings, the central venous pressure has to be low 14,15. A good coordination with the anesthesiologists is therefore required.
The presented data comprise a period of 16 years of our experience which revealed three essential complexes contributing to the improvement of the results of partial liver resections:
The improvement of three-dimensional imaging and the possibility of virtual operation planning.
The recent findings about hemostasis and intraoperative volume management as well as the principles of ischemia–reperfusion damages and their influence on surgical proceedings in liver surgery.
The development of modern selective dissection techniques.
Blood loss and the ischemia–reperfusion syndrome represent important risk-factors for postoperative liver failure which is the main cause of postoperative lethality.
The major anatomical partial liver resection today represents a widely standardised intervention with a lethality rate of less than 3%.
Especially, the introduction of new dissection techniques such as the water-jet or the CUSA® led to a reduction of blood loss and resection time. By this the necessity of the Pringle's manoeuvre and the hereby caused disadvantages of ischemia and reperfusion can be reduced.
Oncological aspects
In the beginning the water-jet dissection technique was assessed very critically, especially in oncological resections. It was feared that the water beam might penetrate the liver tissue without control so that it would contact the tumour and tumour cells could be spread into the operating field. By this the local recurrence rate might increase and the over – all survival might decrease.
The analysis of the over-all survival following resection of liver metastases and hepatocellular carcinoma however showed that the dissection technique has no influence on the long-term survival. In a comparative clinical study between the different dissection techniques water-jet, CUSA® and blunt dissection of 591 patients who underwent liver resection, no significant differences were found between the Kaplan-Meier survival curves, even in cases of extended liver resections 12,13.
Laparoscopic liver resection
In case of a favourable localisation of the tumour the above-mentioned techniques even allow a laparoscopical approach. Innovative dissection techniques are currently tested for their applicability in liver resection. Subject to the localisation of the liver area which has to be removed and to the consistence of the liver tissue one of the different dissection techniques might prove to be more convenient versus the competing methods.
Laparoscopic handpieces are available which are employed in laparoscopically performed liver resections 16,10 and in other laparoscopic surgical fields 17. In the meantime, angularly adjustable handpieces are obtainable which enhance the action scope and the range of application of the water-jet in laparoscopic surgery.
Beyond doubt, every instrument is only as good as the hand that uses it. Besides the objective characteristics of a dissection technique, the individual experience of a certain technique is crucial.
Outlook
In the experimental studies additional application of high-frequency current or laser energy were able to essentially raise the dissection speed with retained selectivity. Smaller vessels with a diameter up to 1 mm are thereby coagulated, larger vessels remain unharmed 18. Up to now these techniques have not achieved clinical practice yet.
Conclusion
The water-jet dissection technique is safe and feasible in hepato-biliary surgery. In our experience this technique is considerably faster than CUSA® or blunt dissection. Pringle-time and blood loss can be reduced by using the water-jet. Finally, the full potential of this technique has not been tapped yet. Especially, the combination of water-jetting with high-frequency current or laser energy might be very interesting for future investigations. However, innovative and auspicious methods as the UltraCision® – technology or the LigaSure™, but also further developments of the ultrasound dissection in combination with high-frequency current should be considered.
Acknowledgements and disclosures
We want to thank Stichlmayr G. and Sattler M. for the support.
Footnotes
1Data from F.W. Schildberg (1991–2001) from the Surgical Department, University Hospital Großhadern, Munich, Head of the Department.Data from H.G. Rau (2002–2007) Surgical Department of visceral-, thoracic- and vascular surgery, Amper-Hospital, Dachau, Head of the Department
References
- 1.Fasulo F, Giori A, Fissi S, Bozzetti F, Doci R, Gennari L. Cavitron Ultrasonic Surgical Aspirator (CUSA) in liver resection. Int. Surg. 1992;77:64–6. [PubMed] [Google Scholar]
- 2.Gertsch P, Pelloni A, Guerra A, Krpo A. Initial experience with the harmonic scalpel in liver surgery. Hepatogastroenterology. 2000;47:763–6. [PubMed] [Google Scholar]
- 3.Lin T, Tsu K, Mien C, Chen C. Study on lobectomy on the liver. J Formosa Med Assoc. 1958;57:742–59. [Google Scholar]
- 4.Little JM, Hollands MJ. Impact of the CUSA and operative ultrasound on hepatic resection. HPB Surg. 1991;3:271–7. doi: 10.1155/1991/62986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pachter HL, Spencer FC, Hofsterr FC, Coppa GF. Experience with the finger fracture technique to achieve intrahepatic hemostasis in 75 patients with severe injusties of the liver. Ann Surg. 1983;197:771. doi: 10.1097/00000658-198306000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bengmark S. Leberchirurgie. Chir Gastroenterol. 1987;3:5–11. [Google Scholar]
- 7.Papachristou DN, Barters R. Resection of the liver with a water jet. Br J Surg. 1982;69:93–4. doi: 10.1002/bjs.1800690212. [DOI] [PubMed] [Google Scholar]
- 8.Rau HG, Arnold H, Schildberg FW. Schneiden mit dem Wasser-Strahl (Jet-Cutting) - eine Alternative zum Ultraschallaspirator? Chirurg. 1990;61:735–8. [PubMed] [Google Scholar]
- 9.Hirano T, Uenohara H, Komatsu M, Nakagawa A, Satoh M, Ohyama H, et al. Holmium:YAG laser-induced liquid jet dissector: a novel prototype device for dissecting organs without impairing vessels. Minim Invasive Neurosurg. 2003;46(2):121–5. doi: 10.1055/s-2003-39339. [DOI] [PubMed] [Google Scholar]
- 10.Rau HG, Buttler E, Meyer G, Schardey HM, Schildberg FW. Laparoscopic liver resection compared with conventional partial hepatectomy - A prospective analysis. Hepato-Gastroenterology. 1998;45:2333–8. [PubMed] [Google Scholar]
- 11.Simillis C, Constantinides VA, Darzi A, Lovegrove R, Jiao L, Antoniou A. Laparoscopic versus open hepatic resections for benign and malignant neoplasms - a meta-analysis. Surgery. 2007;141:203–11. doi: 10.1016/j.surg.2006.06.035. [DOI] [PubMed] [Google Scholar]
- 12.Rau HG, Wichmann M, Schinkel S, Buttler E, Pickelmann S, Schauer R. Surgical techniques in hepatic resections: ultrasonic aspirator versus jet cutter - a prospective randomized clinical trial. Zentralbl Chir. 2001;126:586–90. doi: 10.1055/s-2001-16573. [DOI] [PubMed] [Google Scholar]
- 13.Rau HG, Zimmermann A, Wardemann C, Schildberg FW. Standards of surgical techniques in liver metastases. Chir Gastroenterol. 2003;19:333–9. [Google Scholar]
- 14.Johnson M, Mannar R, Wu AV. Correlation between blood loss and inferior vena caval pressure during liver resection. Br J Surg. 1998;85(2):188–90. doi: 10.1046/j.1365-2168.1998.00570.x. [DOI] [PubMed] [Google Scholar]
- 15.Wang WD, Liang LJ, Huang XQ, Yin XY. Low central venous pressure reduces blood loss in hepatectomy. World J Gastroenterol. 2006;12(6):935–9. doi: 10.3748/wjg.v12.i6.935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rau HG, Meyer G, Jauch K, Cohnert TU, Buttler E, Schildberg FW. Leberresektion mit dem Wasser-Jet. Konventionell und laparoskopisch. Chirurg. 1996;67:546–51. [PubMed] [Google Scholar]
- 17.Jakob S, Kehler U, Reusche E, Friedrich HJ, Arnold H. Endoscopic use of the water jet dissector in the cerebral ventricle system - an experimental study. Zentralbl Neurochir. 2000;61(1):14–21. doi: 10.1055/s-2000-8260. [DOI] [PubMed] [Google Scholar]
- 18.Rau HG, Buttler E, Baretton G, Schardey HM, Schildberg FW. Jet-Cutting supported by high frequency current: new technique for hepatic surgery. World J. Surg. 1997;21:254–60. doi: 10.1007/s002689900225. [DOI] [PubMed] [Google Scholar]