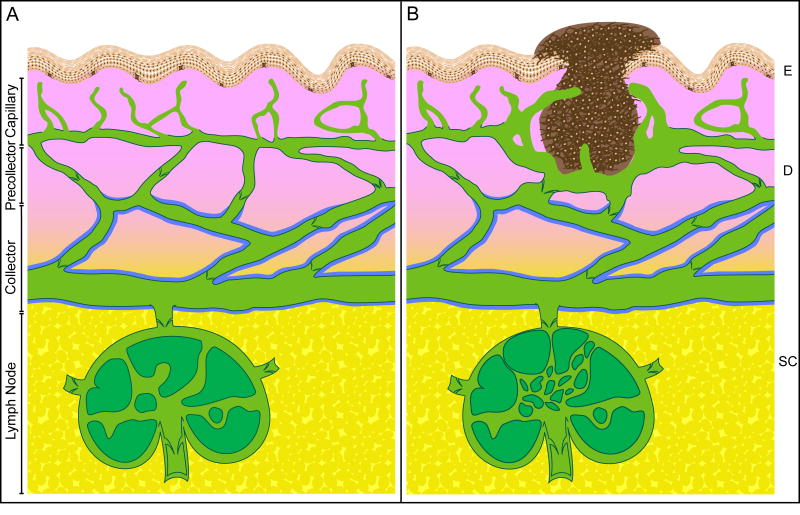
Figure 1.
Structural diagram of the cutaneous lymphatic system under physiological and pathological (tumor-bearing) conditions. A. Interstitial fluid is drained through wide luminal capillaries (green color) that extend up near the epidermis (E, peach color). Capillaries are composed of thin layers of endothelial cells connecting to the extracellular matrix through anchoring filaments. Capillaries possess inter-endothelial cell gaps, discontinuous basement membrane, no valves, and no pericyte coverage. In the dermis (D, pink color), capillaries drain into lymphatic vessels called precollectors that have a continuous basement membrane (denoted by dark green line) and valves that prevent the reflux of lymph. At the border to the subcutis (SC, yellow color), precollectors drain into collecting lymphatic vessels that are surrounded with smooth muscle cells or pericytes (denoted by blue line) that constrict to propel the lymph along to regional lymph nodes. B. An invasive melanoma (dark brown color) is shown. Tumor cells metastasize through peri-tumoral and intratumor lymphatic capillaries. Lymphatic capillary density around the tumor is increased and tumor-associated lymphatic capillaries are dilated and hyperplastic. A few lymphatic capillaries have sprouted into the tumor. The sentinel lymph node is shown with lymphangiogenic vessels as well. Note: this diagram is not drawn exactly to scale.