Abstract
Restoration of shoulder function is one of the most critical goals of treatment of brachial plexus injuries. Primary repair or nerve grafting of avulsion injuries of the upper brachial plexus in adults often leads to poor recovery. Nerve transfers have provided an alternative treatment with great potential for improved return of function. Many different nerves have been utilized as donor nerves for transfer to the suprascapular nerve and axillary nerve for return of shoulder function with variable results. As our knowledge of shoulder neuromuscular anatomy and physiology improves and our experience with nerve transfers increases, so evolve the specific transfer procedures. This article presents a technique and rationale for reconstructing shoulder function by transferring the distal spinal accessory nerve to the suprascapular nerve and the nerve branch to the medial head of the triceps to the axillary nerve, both through a posterior approach.
Keywords: Nerve, Palsy, Reconstruction, Nerve transfer, Shoulder, Brachial plexus
Introduction
Loss of shoulder and elbow function is typical of upper brachial plexus injuries. Disruption of the C5 and C6 roots results in an Erb-type palsy, with loss of supply to muscles innervated by the suprascapular nerve, axillary nerve, and musculocutaneous nerve. With particular regard to shoulder abduction, it is not uncommon for the axillary nerve (C5, C6) component of the posterior cord to be compromised, whereas the radial nerve (C5, C6, C7, C8, T1) component remains intact because of its more plentiful nerve root sources. In cases where spontaneous recovery does not occur, reconstruction is recommended. When these components of the brachial plexus are compromised, restoration of elbow flexion is generally the first priority. Shoulder abduction and external rotation are of next greatest priority, as these are critical functions whose absence is particularly devastating to the patient.
These upper brachial plexus injuries are most commonly root avulsion injuries. In these cases no feasible proximal nerve reconstruction procedure exists. Other options for shoulder stability include arthrodesis, which sacrifices motion, and tendon transfer, which provides suboptimal results. Recent developments in nerve transfer procedures promise improved results over traditional reconstructive procedures. Nerve transfers provide earlier reinnervation to the target muscles by taking advantage of anatomic proximity compared to procedures performed at the nerve root level. In this article, we present our preferred technique for reconstruction of shoulder function—through a posterior approach similar to that of Bahm et al. [1], the distal spinal accessory nerve is transferred to the suprascapular nerve and the nerve to the medial head of the triceps is transferred to the axillary nerve proximal to the teres minor branch—and describe how this meets the criteria for favorable nerve transfer [14].
Technique
The patient is induced under general anesthesia in the supine position and then placed onto the operating table in the prone position with the arms adducted at the sides. The superior and posterior shoulder, the axilla, and the entire arm are prepped as a surgical field. Surgical markings are presented in Fig. 1, schematic representations of the transfers are provided in Fig. 2, and intraoperative exposures are provided in Fig. 3.
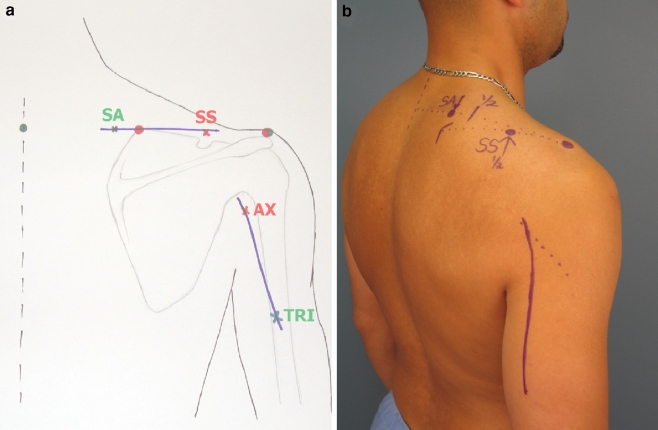
Figure 1.
(a) Posterior approach, double nerve transfer for shoulder function surgical markings. The midline spinous process is marked (green dot) as is the acromion (red/green dot). The location of the spinal accessory nerve is marked (SA) at a distance 40% from the dorsal midline to the acromion parallel to a line along the superior border of the scapula. The superior angle of the scapula is marked (red dot), and the location of the suprascapular notch containing the suprascapular nerve is identified and marked (SS) at the midpoint between the superior angle of the scapula and the acromion along the superior border of the scapula. The surgical incision is planned in a transverse fashion to expose both nerves. The posterior approach to the quadrangular space containing the axillary nerve (AX) is marked at the posterior border of the deltoid muscle just inferior to the scapular neck and infraglenoid tubercle. The surgical incision is planned from this point distally along the posterior border of the arm in line with the interval between the long and lateral heads of the triceps muscle, approximately 10–12 cm in length. At the distal aspect of this approach, the nerve branch to the medial head of the triceps muscle (TRI) is located. (b) Preoperative markings on human subject. SA, spinal accessory; SS, suprascapular. Note that SA is marked medial to the halfway point from midline to the acromion, and that SS is marked halfway from the superomedial border of the scapula to the acromion. The surgical incision connects these two points. The incision for the triceps branch-to-axillary nerve transfer is also marked at the posterior arm. The dotted line at the superior aspect of this incision mark identifies the posterior border of the deltoid muscle.
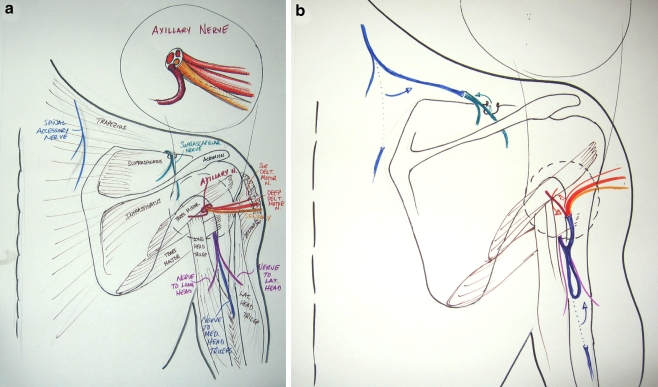
Figure 2.
(a) Posterior approach for double nerve transfer for shoulder function; posterior shoulder anatomy. Note that the posterior approach allows access to the more distal aspect of the spinal accessory nerve. The suprascapular nerve passes over the suprascapular notch beneath the superior transverse scapular ligament. The inset shows the components of the axillary nerve at the level of the quadrangular space. Note that the larger motor branch to the deltoid comprises the deep aspect of the nerve, whereas the other smaller components, including the nerve to teres minor and the sensory component (superior brachial cutaneous), comprise the superficial aspect of the nerve. The nerve branch to the medial head of the triceps is found along with the radial nerve deep to the interval between the long and lateral heads of the triceps muscle overlying the humerus. (b) Posterior approach for double nerve transfer for shoulder function, following nerve transfer. The distal spinal accessory nerve has been transected as distally as possible and the proximal segment transferred to the distal segment of the suprascapular nerve, which has been transected just proximal to the suprascapular notch. The branch to the medial head of the triceps has been transected distally and the proximal segment transferred to the distal segment of the axillary nerve. The axillary nerve has been transected as proximally as possible in the quadrangular space. The nerve to teres major is included as a recipient in the transfer and no special effort is made to exclude the sensory branch of the axillary nerve (superior brachial cutaneous nerve).
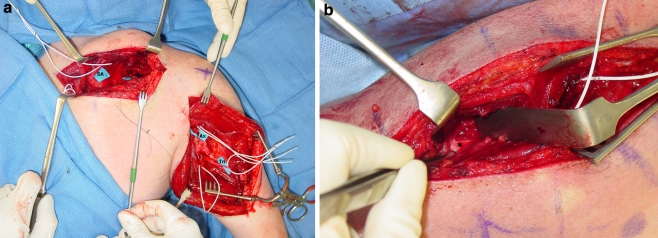
Figure 3.
(a) Intraoperative exposure. All nerves have been identified and marked with blue backgrounds. SA, spinal accessory nerve; SS, suprascapular nerve; Ax, axillary nerve; Tri, nerve branch to medial head of triceps. Note that the suprascapular nerve is deep within the operative site. It and the axillary nerve have been divided. The donor nerves have not yet been divided. (b) Intraoperative exposure; a closer view of the suprascapular dissection. The trapezius muscle has been divided and is being retracted. The superior transverse scapular ligament (asterisk) has been identified. The ligament is glistening white. Note that the superior border forms a sharp edge. The forceps are resting in the hollow of the notch below the ligament.
Accessory to Suprascapular Nerve Transfer
Proper preoperative identification and marking of relevant landmarks is critical for ease of identification of both the distal accessory and suprascapular nerves. To identify the location of the distal accessory nerve, the dorsal midline and the acromion are marked. A point 40% of the distance from the dorsal midline to the acromion along the superior border of the scapula is marked and identifies the approximate location of the distal accessory nerve. To identify the location of the suprascapular nerve, the superior angle of the scapula and the acromion are marked. A point marked midway between these two points identifies the area of the suprascapular notch that transmits the suprascapular nerve (Fig. 1). The dissection is performed under loupe magnification, and bipolar electrocautery is used throughout for hemostasis. The surgical incision is planned with a straight line between the marks identifying the two nerves. The skin is incised along this line and the dissection is carried just deep to the trapezius muscle. The superior border of the scapula is palpated and dissection carried deep, through or above the supraspinatus muscle, toward the notch with care taken to identify the suprascapular artery, which courses over, or superior to, the superior transverse scapular ligament that forms the roof over the notch. The identification of the ligament and notch is very “tactile.” The ligament is felt on the “upsweep” of the scapula with the index finger, and the hollow of the foramen is felt below the ligament. With the artery protected, the ligament is palpated as a sharp band and is exposed bluntly with a “peanut” sponge, or Kittner gauze (Fig. 3b). The ligament is then divided sharply under direct vision. In some cases, the ligament will be bony, not fibrous, and use of a small-tipped rongeur will be necessary. In most cases, the nerve is not identified until the ligament has been divided. Again, the presence of the nerve is heralded by surrounding adipose. The nerve is exposed as it passes through the suprascapular notch and distally. It is deep in the fat and, again, sweeping with a “peanut” or slow spreading in this area with scissors or a hemostat will eventually allow visualization of the nerve. It is dissected as proximally as possible to accommodate a tension-free transfer. The nerve is confirmed to be inactive with a disposable nerve stimulator. After isolation of the suprascapular nerve, the separation of the trapezius muscle is carried medially toward the location of the spinal accessory nerve. Care is taken to separate the trapezius parallel to the course of its fibers. The presence of the nerve is generally heralded by adipose tissue, and identification is greatly aided with the use of a disposable nerve stimulator. The nerve is generally found running in a superolateral-to-inferomedial direction as it enters the deep surface of the trapezius muscle. After confirmation of activity of the accessory and inactivity of the suprascapular nerve by nerve stimulation, the suprascapular nerve is divided first at its most proximally identified point, and then the accessory nerve divided as distal as necessary to allow a transfer without tension. With this approach, proximal branches of the accessory nerve need not be divided and adequate nerve length obviates the need for nerve grafting. The nerve ends are prepared and the proximal segment of the accessory nerve is transferred and sutured to the distal segment of the suprascapular nerve with interrupted 9–0 nylon under an operating microscope. This approximation is usually performed after dissection and transfer of the medial triceps branch to the axillary nerve to consolidate time under the microscope.
Medial Triceps to Axillary Nerve Transfer
Again, under loupe magnification, a longitudinal incision approximately 10 to 15 cm in length is made from the posterior border of the deltoid muscle along a line falling between the long and lateral heads of the triceps muscles (Fig. 1). Dissection is carried deep to expose the quadrangular space that transmits the axillary nerve and a triangular space bounded by the teres major superiorly, the long head of the triceps medially, and the lateral head of the triceps laterally that contains the radial nerve and triceps nerve branches. The teres major muscle with its transversely oriented fascia, unique in this area, is the key landmark, with the axillary nerve located above it and the radial nerve located below it. The nerve branch to the medial head of the triceps is isolated centrally in this space, running closely adjacent to the radial nerve although distinctly separate from it. Identification can be confirmed by electrical stimulation. The axillary nerve in the quadrangular space is easily identified by tracing its sensory branch proximally. Care is taken to isolate the axillary nerve proximal to the takeoff of the branch to teres minor. No specific effort is made to exclude the sensory division of the axillary nerve, although in some circumstances this division has already occurred and it may be excluded without any significant effort, as it is the most inferior branch of the axillary nerve. After confirmation of lack of activity with a disposable nerve stimulator, the axillary nerve at its most proximal point is then divided. The nerve to the medial head of the triceps is then divided distally, and in most cases provides enough length to comfortably reach the recipient axillary nerve with adequate redundancy without any other maneuvers. However, if necessary, the tendinous portion of the inferior border of the teres major may be divided and the medial head triceps branch may be neurotized from the radial nerve proper or from the branch to the lateral head of the triceps to allow further proximal reach of the nerve branch. The patient's elbow and shoulder are then put through range of motion to assure a tension-free repair. The cut nerve ends are prepared appropriately and the reflected proximal segment of the donor triceps branch is sutured to the distal segment of the recipient axillary nerve with interrupted 9–0 nylon suture under the operating microscope.
The wounds are then closed in a layered fashion with use of a subcutaneous closed system drain as deemed appropriate. If a drain is used, it is removed by postoperative day 3. The patient is placed in a shoulder immobilizer postoperatively, allowing intermittent gentle elbow range of motion to prevent stiffness. At approximately 3 weeks, shoulder and elbow motion are gradually resumed to maintain range of motion. Strengthening is begun after reinnervation and resumption of deltoid muscle activity.
Discussion
Although the first reported nerve transfer for reconstruction of shoulder function was reported by Lurje [13] in 1948, the last two decades have witnessed their revival for reconstruction of the brachial plexus, with major advances in the development of nerve transfers made in the last decade. Procedures have utilized donors from the intercostal nerves [5, 6, 20], thoracodorsal nerve [20], medial pectoral nerve [20, 21], long thoracic nerve [20], phrenic nerve [6], distal accessory nerve [6, 11, 19], ipsilateral C7 root [7], contralateral C7 root [8], suprascapular nerve [20], and hypoglossal nerve [16]. Although tendon transfers still provide a reconstructive option when no potential for target muscle recovery exists as a result of a prolonged denervation and extensive atrophy, it seems increasingly clear that nerve transfers offer greater potential for functional recovery of shoulder function than tendon transfers, largely because of unaltered muscular biomechanics with nerve transfers. As we gain more experience, our selection of procedures becomes more refined, as exemplified by the current development of transfers to restore axillary nerve function.
Our group reported transfer of triceps fascicles of the radial nerve to the axillary nerve in 2000 [18]. More recently, Leechavengvongs et al. [12] and Witoonchart et al. [24] developed a transfer utilizing the nerve branch to the long head of the triceps and targeting the deltoid motor branch of the axillary nerve through a posterior approach. This and other transfers utilizing various components of the radial nerve show promising results [2, 10, 12]. Use of the distal triceps nerve branches allows transfer to the recipient axillary nerve much closer to the target muscle than using triceps fascicles isolated from the more proximal radial nerve. This is a principle criterion for a favorable nerve transfer and one of its key benefits over traditional proximal nerve repair or nerve grafting. In addition, the synergistic function of the triceps and deltoid muscles simplifies retraining and facilitates functional recovery. The posterior approach allows maximum exploitation of these principles, and in partial axillary nerve injuries, it allows identification and reconstruction of the nonfunctioning branches with preservation of the functioning branches. Currently, there are two uncertainties with regard to the specifics of this transfer: (1) which triceps nerve branches provide the best donor, and (2) which aspects of the axillary nerve constitute the ideal recipient. Although we agree with Leechavengvongs et al. that a posterior approach provides excellent access to the donor and recipient nerves for axillary nerve reconstruction, we disagree with their choice of donor triceps branch and their recommendation not to innervate the nerve to teres minor.
In addition to proximity to the target muscle and synergy of function, principal criteria for a donor nerve for transfer include providing an adequate size match, corresponding function (motor donor to restore motor function, sensory donor to restore sensory function), ability of functional reeducation, and expendability [1, 7]. Existing transfers of the nerve branch to the long head of the triceps are supported by the use of the long head of the triceps as a pedicled or free flap for tissue reconstruction, first reported by Hartrampf et al. [9]. The long head of the triceps is generally the largest of the three, and in contrast to the other two heads, it provides some stability of humeroscapular adduction as it originates from the infraglenoid tubercle of the scapula. It is preferred over the medial and lateral heads as a free flap because of its size and because it has a separable blood supply. Although there is some evidence that the long head favors isometric function and the lateral and medial heads favor isotonic function [23], all three heads promote elbow extension and there is no evidence that loss of any one of the three causes a noticeable deficit in triceps function. Thus, the choice of which nerve branch to the triceps to favor for transfer may be based on other factors. In strict terms of principles of donor selection, the long head of the triceps, as a humeral adductor, is not synergistic with deltoid function. The nerve branch to the medial head of the triceps is usually the easiest to expose at the interval between the lateral and long heads. In addition, it is longer and its harvest does not require intramuscular dissection, which may be required to obtain an adequate length of the branch to the long head or lateral head. We feel that the benefits of the ease of identifying the branch to the medial head and the added length it provides support its use as a more appropriate donor.
More important in determining the ideal nerve transfer for reconstruction of shoulder function is which aspects of the axillary nerve constitute the best recipient. External shoulder rotation is a critical element of function and a principal goal of reconstruction. It seems well accepted that restoration of shoulder abduction and external rotation by reconstruction of both the axillary nerve and the suprascapular nerve provides better results than reconstruction of either one alone [2, 6, 12, 17]. Similarly, the teres minor provides two important functions: glenohumeral capsular stability and external rotation. Given the importance of the suprascapular-innervated muscle for shoulder stability and external rotation, and the major contribution of the teres minor to these functions, it seems logical to include teres minor in the reconstructive effort, and donor nerve contributions to its reinnervation are not felt to be wasted or to detract significantly from the ability to reinnervate the deltoid. For this reason, we prefer to include the branch of the axillary nerve to teres minor as a recipient in the nerve transfer. In cases where it cannot be easily excluded, we make no great effort to exclude the sensory branch of the axillary nerve, as studies have shown that donor motor nerves will preferentially seek motor targets over sensory targets [4]. We feel that this does not detract from the ability of the donor nerve to reinnervate the teres minor and deltoid muscles, and is thus outweighed by the risk and operative time required to actively exclude the sensory component. Occasionally, however, the inferior, sensory component can be easily identified and excluded from the recipient axillary nerve.
Previous experiences with nerve transfers for reconstruction of elbow flexion have taught us a valuable lesson about the effect of recipient nerves on the functional results. The Oberlin transfer of ulnar nerve motor fascicles to the biceps branch of the musculocutaneous nerve alone provided lesser degrees of recovered elbow flexion strength than prior, more proximal nerve transfers to the entire musculocutaneous nerve including branches to both the biceps and the brachialis muscles. This provided the impetus for the senior author's (S.E.M.) development of a double fascicular transfer from both the median and the ulnar nerves to musculocutaneous branches to both the biceps and the brachialis, which provides better recovery of elbow flexion strength than reinnervation of the biceps muscle alone [15, 22]. Similarly, for reconstruction of the axillary nerve, transfers that reinnervate the teres minor in addition to the deltoid would be expected to provide better shoulder function, particularly with regard to external rotation and glenohumeral stability, than those that exclude the branch to teres minor.
The posterior approach to the distal spinal accessory nerve is critical in the effort to gain adequate length of the donor nerve to avoid the need for grafting while at the same time targeting the suprascapular nerve at a point much closer to the muscles it innervates. In addition, it allows greater potential for preservation of the more proximal branches from the accessory nerve to the upper trapezius muscle, potentially reducing donor morbidity [3]. This variation in the accessory-to-suprascapular nerve transfer thus maximizes adherence to the principles of nerve transfer in a similar manner to the medial head triceps branch-to-axillary nerve transfer. In addition, decompression of the suprascapular nerve at the notch is an added benefit of this posterior approach. Finally, approaching both nerve transfers posteriorly, with no need for patient repositioning to reconstruct shoulder function, provides for greater technical convenience and economy of operating time.
Beyond elbow function, there is no more important goal of reconstruction of upper brachial plexus injuries than shoulder function. We regard the restoration of suprascapular nerve function as preferable to that of axillary nerve function, but every effort should be made to restore both when possible. Results of nerve transfers to the suprascapular and axillary nerves are well known, and there seems to be a consensus that reconstruction of both nerves is superior to either one alone [6, 12, 17]. Differences in outcomes among the more specific variations on these transfers will require continued experience and further study. The purpose of the present article is to present our preferred nerve transfer technique for reconstruction of shoulder function. The nerve branches to the triceps muscles provide ideal donor nerves for transfer to the axillary nerve, and the distal accessory nerve provides an ideal donor for transfer to the suprascapular nerve, both in proximity to and in synergy with the target muscles. We feel that the posterior approach for this double nerve transfer is ideal in terms of technical accomplishment and functional shoulder restoration of upper brachial plexus injury.
References
- 1.Bahm J, Naoman H, Becker M. The dorsal approach to the suprascapular nerve in neuromuscular reanimation for obstetric brachial plexus lesions. Plast Reconstr Surg 2005;115:240–4. [PubMed]
- 2.Bertelli JA, Ghizoni MF. Reconstruction of C5 and C6 brachial plexus avulsion injury by multiple nerve transfers: spinal accessory to suprascapular, ulnar fascicles to biceps branch, and triceps long or lateral head branch to axillary nerve. J Hand Surg 2004;29A:131–9. [DOI] [PubMed]
- 3.Bertelli JA, Ghizoni MF. Improved technique for harvesting the accessory nerve for transfer in brachial plexus injuries. Neurosurgery 2006;58(4) Suppl 2:ONS-366-70; discussion ONS-370. [DOI] [PubMed]
- 4.Brushart TME. Preferential reinnervation of motor nerves by regenerating motor axons. J Neurosci 1988;8:1026–31. [DOI] [PMC free article] [PubMed]
- 5.Celli L, Rovesta C, Balli A. Neurotization of brachial plexus avulsion with intercostal nerves (personal techniques). In: Brunelli G, editor. Textbook of microsurgery. Milano: Masson; 1988. p. 789–95.
- 6.Chuang DC-C, Lee GW, Hashem F, Wei F-C. Restoration of shoulder abduction by nerve transfer in avulsion brachial plexus injury: evaluation of 99 patients with various nerve transfers. Plast Reconstr Surg 1995;96:122–8. [DOI] [PubMed]
- 7.Gu YD, Cai PQ, Xu F, Peng F, Chen L. Clinical application of ipsilateral C7 nerve root transfer for treatment of C5 and C6 avulsion of brachial plexus. Microsurgery 2003;23(2):105–8. [DOI] [PubMed]
- 8.Gu YD, Zhang GM, Chen DS, Cheng XM, Zhang LY, Yan JG, Cai PQ, Shen LY. Cervical nerve root transfer from contralateral normal side for treatment of brachial plexus root avulsions. Chin Med J 1991;104:208–11. [PubMed]
- 9.Hartrampf CR, Elliott LF, Feldman S. A triceps musculocutaneous flap for chest-wall defects. Plast Reconstr Surg 1990;86:502–9. [DOI] [PubMed]
- 10.Kawai H, Akita S. Shoulder muscle reconstruction in the upper type of the brachial plexus injury by partial radial nerve transfer to the axillary nerve. Tech Hand Up Extrem Surg 2004;8:51–5. [DOI] [PubMed]
- 11.Kline DG, Hudson AR. Stretch injuries to the brachial plexus. In: Kline DG, Hudson AR eds. Nerve injuries: operative results for major nerve injuries, entrapments, and tumors. Philadelphia: Saunders; 1995, 135: p. 415–6.
- 12.Leechavengvongs S, Witoonchart K, Uerpairojkit C, Thuvasethakul P. Nerve transfer to deltoid muscle using the nerve to the long head of the triceps, part II: a report of 7 cases. J Hand Surg 2003;28A:633–8. [DOI] [PubMed]
- 13.Lurje A. Concerning surgical treatment of traumatic injury of the upper division of the brachial plexus (Erb's-type). Ann Surg 1948;127:317–26. [DOI] [PMC free article] [PubMed]
- 14.Mackinnon SE, Novak CB. Nerve transfers. New options for reconstruction following nerve injury. Hand Clin 1999;15:643–66. [PubMed]
- 15.Mackinnon SE, Novak CB, Myckatyn TM, Tung TH. Results of reinnervation of the biceps and brachialis muscles with a double fascicular transfer for elbow flexion. J Hand Surg 2005;30A:978–85. [DOI] [PubMed]
- 16.Malessy MJA, Hoffmann CFE, Thomeer RTWM. Initial report on the limited value of hypoglossal nerve transfer to treat brachial plexus root avulsions. J Neurosurg 1999;91:601–4. [DOI] [PubMed]
- 17.Merrell GA, Barrie KA, Katz DL, Wolfe SW. Results of nerve transfer techniques for restoration of shoulder and elbow function in the context of a meta-analysis of the English literature. J Hand Surg 2001;26A:303–14. [DOI] [PubMed]
- 18.Nath RK, Mackinnon SE. Nerve transfers in the upper extremity. Hand Clin 2000;16:131–9. [PubMed]
- 19.Oberlin C, Beal D, Leechavengvongs S, Salon A, Dauge MC, Sarcy JJ. Nerve transfer to biceps muscle using a part of ulnar nerve for C5–C6 avulsion of the brachial plexus: anatomical study and report of four cases. J Hand Surg 1994;19A (2):232–7, Mar. [DOI] [PubMed]
- 20.Samardzic M, Grujicic D, Antunovic V. Nerve transfer in brachial plexus traction injuries. J Neurosurg 1992;76(2):191–7, Feb. [DOI] [PubMed]
- 21.Samardzic M, Grujicic D, Rasulic L, Bacetic D. Transfer of the medial pectoral nerve: myth or reality? Neurosurgery 2002; 50:1277–82. [DOI] [PubMed]
- 22.Tung TH, Novak CB, Mackinnon SE. Nerve transfers to the biceps and brachialis branches to improve elbow flexion strength after brachial plexus injuries. J Neurosurg 2003;98:313–8. [DOI] [PubMed]
- 23.Van Groeningen CJ, Erkelens CJ. Task-dependent difference between mono- and bi-articular heads of the triceps brachii muscle. Exp Brain Res 1994;100:345–52. [DOI] [PubMed]
- 24.Witoonchart K, Leechavengvongs S, Uerpairojkit C, Thuvasethakul P, Wongnopsuwan V. Nerve transfer to deltoid muscle using the nerve to the long head of the triceps: part I. An anatomic feasibility study. J Hand Surg 2003;28A:628–32. [DOI] [PubMed]