Abstract
PURPOSE
To study whether fixation patterns changed over time in patients with central scotomas from geographic atrophy from age-related macular degeneration.
DESIGN
Prospective cohort study.
METHODS
SETTING
Institutional.
PATIENT OR STUDY POPULATION
Prospective natural history study of geographic atrophy included 34 eyes of 25 patients with baseline acuity between 20/80 and 20/200 and with subsequent follow-up.
OBSERVATION PROCEDURES
Baseline and annual follow-up visits included best-corrected visual acuity, scanning laser ophthalmoscope macular perimetry, reading rate, and clinical evaluation.
MAIN OUTCOME MEASURES
Location of eccentric preferred retinal locus for fixation (PRL).
RESULTS
At baseline, 77% of study eyes had a PRL. At the final visit (median follow-up, 5.3 years), 91% of study eyes had a PRL, with 81% of the eyes retaining the baseline PRL location. Fixation with the scotoma to the right and fixation with the scotoma superior were the first and second most common fixation patterns, respectively. Reading rates of <50 words/min were present in 54% of eyes. Eyes fixating with the scotoma to the left tended to have lower reading rates than eyes fixating with right or superior patterns.
CONCLUSION
Fixation with right pattern remained the most common fixation pattern, both in patients with a PRL at baseline and in patients who had a PRL during follow-up. Eyes with a PRL at baseline generally retained this pattern. The reading rate data suggest an advantage of fixation with right or superior pattern, rather than left. Reading rate declined further during follow-up in most patients.
For a patient with a central scotoma to optimize the use of the remaining seeing retina, it is important that an eccentric site for fixation, called a preferred retinal locus (PRL), be established. In this way, a patient can place the object of interest onto seeing retina in a consistent manner, by fixating so that the scotoma is moved away from the object of interest. Unless a patient can move the scotoma away, the patient will not be able optimally to use low-vision devices or the remaining seeing retina. In addition, the adoption of a PRL allows the patient systematically to place the object of interest there and avoids the scanning back and forth eye and head movements that occur when there is no established PRL.1
We and others have reported on the predilection of fixation patterns so that the scotoma is to the right or above fixation in patients with central scotomas.2–6 However, little is known about the long-term stability of fixation patterns in these patients.
In 1996, we reported on fixation patterns in patients who had visual acuity between 20/80 and 20/200 from central scotomas that were associated with geographic atrophy (GA), the advanced form of atrophic age-related macular degeneration.4 Our natural history study of GA allowed long-term follow-up evaluation of these patients. The patients did not undergo eccentric fixation training or formal low-vision training that was related to scotoma awareness. We report on the long-term findings of stability in fixation patterns in these patients. To our knowledge, this is the first report about long-term fixation behavior in patients with central scotomas. We also report on the relationship of reading rate to fixation pattern.
PATIENTS AND METHODS
This was part of a prospective natural history study of GA that took place at the Wilmer Institute. Our 1996 article4 included all patients who were seen initially from June 1992 through October 1994 with visual acuity reduced to the 20/80 to 20/200 range from GA in one or both eyes. Of the 35 patients included then, follow-up data are available for 25 patients who form the basis of this article.
We asked patients to return annually for a study visit for at least four years, and we also continued to follow interested patients annually after the study ended. Each visit included measurement of best-corrected visual acuity for each eye, using an Early Treatment Diabetic Retinopathy Study chart and a protocol refraction. The patients underwent a number of other visual function tests, as detailed elsewhere, which included visual acuity under reduced luminance, contrast sensitivity, and reading speed.7 Annual fundus photographs and clinical examination also were performed. Written informed consent was obtained from all subjects after an explanation of the nature and possible consequences of the study had been given. The research was approved by the Johns Hopkins institutional review board.
Scanning laser ophthalmoscope (SLO) macular perimetry was performed at each annual visit. For the first few years of the study, a prototype Rodenstock SLO (G. Rodenstock Instrumente GmbH, Munich, Germany) was used. A one-degree fixation cross was used, and the patient’s fixation behavior was monitored during SLO macular perimetry. An image was captured at the end of the testing that showed the location of fixation, and written comments were appended that described any variations in fixation during the testing. Beginning in the second year of the study, a grid of points, which were predefined and customized for each patient, was tested, with correction for eye movements, as described elsewhere.8 Subsequently, a commercial Rodenstock SLO was acquired, and testing was performed using the Rodenstock scotometry software (G. Rodenstock Instrumente GmbH). The location of the PRL for fixation was the main outcome measure.
RESULTS
The median age of the 25 patients at baseline was 79 years (range, 70 to 90 years). The median follow-up time was 5.3 years (range, 1.1 to 7.2 years), and 21 patients (84%) had ≥4 years of follow-up visits. The last follow-up visit is used for the final fixation pattern, except in three patients who developed choroidal neovascularization in the eye with GA during follow-up evaluation. For these patients, the last visit before the diagnosis of choroidal neovascularization is considered the final visit.
Twenty of the patients had bilateral GA. Both eyes were eligible for this PRL study for nine of these patients, and only one eye was eligible in 11 patients. Four patients had GA without choroidal neovascularization in the study eye and choroidal neovascularization in the fellow eye. One patient had the fellow eye enucleated from trauma. Thus, 34 eyes of the 25 patients met the eligibility criteria for this data analysis (eye with GA with visual acuity in the 20/80 through 20/200 range at baseline) and are included here.
FIXATION PATTERNS
Table 1 gives the fixation patterns that are present at baseline and at the last follow-up visit for the 34 study eyes. At baseline, eight eyes (23%) fixated either in a central region that was surrounded by multifocal GA (here called central), in a spared region that was surrounded by atrophy (called spared), or had no established fixation (no fixation). By no fixation, we mean that the patient put the fixation cross in the atrophy and could not see it or scanned repeatedly without any specific fixation site. Twenty-six eyes (77%) had established a PRL outside the atrophy at baseline. Of these 26 eyes, 50% fixated with the scotoma to the right, and 31% fixated with the scotoma superior to fixation.
TABLE 1.
Eyes With Central Scotomas From Geographic Atrophy Associated With Age-Related Macular Degeneration, With Visual Acuity 20/80–20/200 at Baseline: Baseline and Final Fixation Patterns by Eye
| Pattern | No. of Eyes | Percentage of All Eyes (n = 34) | Percentage of Eyes With PRL* |
|---|---|---|---|
| Baseline fixation | |||
| Central† | 2 | 6 | |
| Spared‡ | 3 | 9 | |
| No fix§ | 3 | 9 | |
| R∥ | 13 | 38 | 50 |
| L¶ | 4 | 12 | 15 |
| S# | 8 | 24 | 31 |
| I** | 1 | 3 | 4 |
| Final fixation | |||
| Central† | 0 | 0 | |
| Spared‡ | 2 | 6 | |
| No fix§ | 1 | 3 | |
| R∥ | 19 | 56 | 61 |
| L¶ | 4 | 12 | 13 |
| S# | 7 | 21 | 23 |
| I** | 1 | 3 | 3 |
Baseline fixation: n = 26; final fixation, n = 31.
Appears to be at (or near) the foveal center, generally surrounded by multifocal geographic atrophy.
In a spared region within the atrophy.
No fixation site was demonstrated.
The scotoma to the right of fixation.
The scotoma to the left of fixation.
The scotoma above (superior to) fixation in visual field space.
The scotoma below (inferior to) fixation in visual field space.
At the final follow-up visit, three eyes fixated in a spared region or had no established fixation, and none of the eyes fixated centrally. Thus, 31 eyes (91%) had established a PRL outside the atrophy. Of these 31 eyes, 19 eyes (61%) fixated with the scotoma to the right; seven eyes (23%) fixated with the scotoma above; four eyes (13%) fixated with the scotoma to the left, and one eye (3%) fixated with the scotoma below fixation. Figure 1 shows a patient who fixated with the scotoma to the right, both at baseline and at the final visit. The PRL is more eccentric at the final visit, which reflects growth of the GA. Figure 2 shows a patient who fixated within a spared region at baseline and switched to fixating with the scotoma superior in the visual field at the final visit.
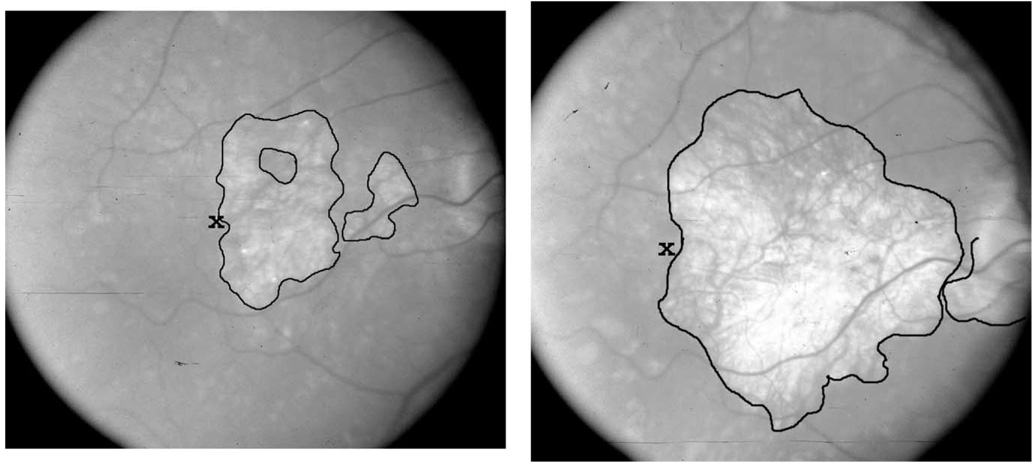
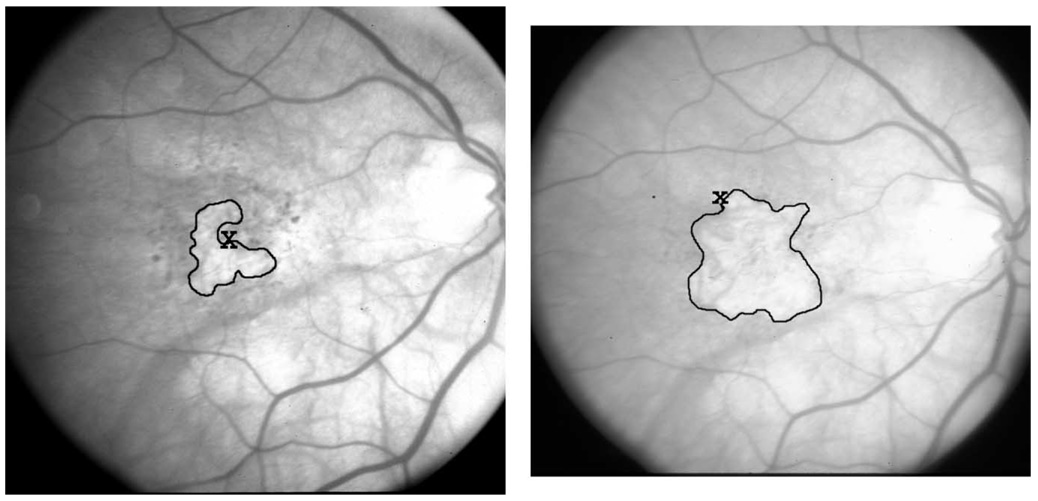
Figure 1.
Progression of geographic atrophy (GA) with a stable fixation pattern. (Left) At baseline, fixation (x) was placed with the atrophy and its corresponding scotoma to the right (circled white areas; there is a nonfoveal spared region within the larger area of GA, which is not used for fixation). At this time, visual acuity was 20/112, and the total area of GA was 3.3 Macular Photocoagulation Study (MPS) disc areas. (Right) Five years later, the GA has enlarged significantly, now measuring 10.3 MPS disc areas. Fixation remains positioned with the atrophy and its corresponding scotoma to the right. At this time, visual acuity was 20/235.
Figure 2.
Progression of geographic atrophy (GA) with the adoption of an eccentric preferred retinal locus (PRL). (Left) At baseline, fixation (x) was placed centrally, with surrounding c-shaped geographic atrophy (circled white area). At this time, visual acuity was 20/118, and the total area of GA was 1.2 Macular Photocoagulation Study (MPS) disc areas. (Right) One year later, the GA has enlarged to 2.4 MPS disc areas and involves the central area. Fixation is now maintained superior to the atrophy on the retina, which corresponds to fixation with the scotoma above fixation in visual field space. Visual acuity is now 20/214.
Table 2 shows the persistence of fixation pattern as a function of the baseline PRL. As expected, the fixation with the scotoma inferior was both a rare occurrence and was not stable. The other fixation patterns are more stable, with 81% of eyes overall retaining the original fixation pattern.
TABLE 2.
Eyes with Central Scotomas From Geographic Atrophy That Is Associated With Age-Related Macular Degeneration, With Visual Acuity 20/80–20/200 at Baseline: Stability of Fixation Pattern From Baseline to Final Visit
| Fixation Pattern at Baseline | No. Remaining the Same at Final valuation |
|---|---|
| R* | 12/13 (92%) |
| L† | 3/4 (75%) |
| S‡ | 6/8 (75%) |
| I§ | 0/1 (0%) |
| Total remaining the same | 21/26 (81%) |
The scotoma to the right of fixation.
The scotoma to the left of fixation.
The scotoma above (superior to) fixation in visual field space.
The scotoma below (inferior to) fixation in visual field space.
Because the status of the fellow eye had an influence on stability of fixation pattern, further analysis of changes in fixation over time includes both eyes of each patient. Table 3 summarizes the changes for each patient by baseline fixation pattern. Nine of the 10 patients, in whom both eyes had the same fixation pattern at baseline, remained with the original fixation pattern at the final follow-up visit. Of five patients in whom one eye had a PRL and the fellow eye could not fixate, four patients retained the original fixation pattern (three patients with the scotoma above fixation and one patient with the scotoma to the left of fixation), and one patient changed fixation patterns (from scotoma below to scotoma above). Of the three patients with one eye fixating with the scotoma to the left and one eye fixating with the scotoma to the right, one patient retained the original fixation; one patient converted to both eyes fixating with the scotoma to the right, and one patient converted to fixating with the scotoma to the left as before and the fellow eye to fixating with the scotoma below fixation.
TABLE 3.
Eyes With Central Scotomas From Geographic Atrophy That Is Associated With Age-Related Macular Degeneration, With Visual Acuity 20/80–20/200 at Baseline: Summary of Long-Term Fixation Patterns in Both Eyes,* by Patient
| Baseline Pattern | Final Pattern | No. of Patients With this Pattern | No Change (%) |
|---|---|---|---|
| Both eyes with same baseline fixation pattern (n = 10 patients, 16 eyes) | 90 | ||
| R, R (n = 7)† | R, R† | 7 | |
| L, L‡ | L, L‡ | 1 | |
| S, S§ | S, S§ | 1 | |
| S, S§ | R, R† | 1 | |
| One eye eccentric fixation, fellow eye no fixation, CNV, or enucleated (n = 5 patients, 5 eyes) | 80 | ||
| S (n = 3)§ | S§ | 3 | |
| L‡ | L‡ | 1 | |
| I∥ | R† | 1 | |
| Different patterns in the two eyes (n = 3 patients, 4 eyes) | 33 | ||
| L‡, R (n = 3)† | L‡, R† | 1 | |
| R, R† | 1 | ||
| L‡, I∥ | 1 | ||
| Eyes without previous PRL outside atrophy (n = 7 patients, 9 eyes) | 38 | ||
| Central (n = 2)¶ | R† | 1 | |
| S§ | 1 | ||
| No fix (n = 3)# | No fix# | 1 | |
| R† | 2 | ||
| Spared (n = 3)** | Spared ** | 2 | |
| L‡ | 1 | ||
CNV = Choroidal neovascularization.
Fixation pattern in both eyes is meant to indicate the findings of monocular SLO fixation analysis for the two eyes of each patient.
Fixation with the scotoma to the right of fixation.
Fixation with the scotoma to the left of fixation.
Fixation with the scotoma above (superior to) fixation in visual field space.
Fixation with the scotoma below (inferior to) fixation in visual field space.
No fixation site was demonstrated.
Fixation appears to be at (or near) the foveal center.
Fixation is in a spared region within the atrophy.
For the remaining seven patients (nine eyes) who fixated within an area of multifocal atrophy, within a spared region, or had no fixation in one or both GA study eyes at baseline, five eyes acquired a PRL outside the atrophy. These included three eyes that fixated with the scotoma to the right, one eye that fixated with the scotoma above fixation, and one eye that fixated with the scotoma to the left of fixation. In only one of these patients was there an eccentric PRL in the fellow eye at baseline. By the final visit, one patient was fixating with the scotoma to the right in both eyes; one patient was fixating with the scotoma above fixation in both eyes, and the remaining patients had an eccentric PRL in at most one eye.
VISUAL ACUITY
LogMAR visual acuities were used to calculate the mean acuities at baseline and at the final visit. The mean visual acuity at baseline was 20/120 (0.78 logMAR), with the baseline acuities constrained to 20/80 to 20/200 inclusive by the eligibility criteria. At the final visit, the mean visual acuity was 20/280 (1.15 logMAR), with a mean worsening of 3.6 lines of Early Treatment Diabetic Retinopathy Study visual acuity. The distribution of acuity loss is given in Table 4. The numbers are small, but there was no evidence that fixation pattern or change in pattern affected the amount of acuity change, except that the two eyes that lost their central fixation tended to worsen more than the other eyes.
TABLE 4.
Eyes With Central Scotomas From Geographic Atrophy That Is Associated With Age-Related Macular Degeneration, With Visual Acuity 20/80–20/200 at Baseline: Change in Visual Acuity From Baselin to Final Visit
| Variable | No. of Eyes |
|---|---|
| Improved by ≥1 line | 2 (6%) |
| Stayed within 1 line of baseline | 4 (12%) |
| Worsened by ≥1 line, but <3 lines | 11 (32%) |
| Worsened by ≥3 lines, but <6 lines | 9 (26%) |
| Worsened by ≥6 lines | 8 (24%) |
READING RATE
One of the most critical consequences of GA is a reduction of reading rate because of the central scotoma and reduced acuity. In our previous article,4 we showed that, within the constrained range of visual acuities, reading rate did not depend on visual acuity. We also showed a significant correlation of reading rate with the size of GA, both measured at baseline.4
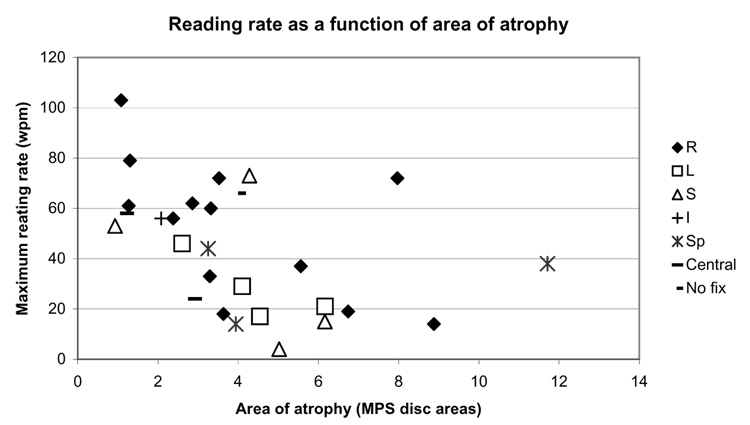
In this study, 28 of the 34 eyes had reading measured at the baseline visit. Figure 3 shows the reading rate vs GA area, with the fixation pattern coded by symbols. The correlation between reading rate and GA area (r = 0.44) is readily apparent. Table 5 shows the relationship between reading rate and fixation pattern when the data are stratified by GA area being three Macular Photocoagulation Study (MPS) disc areas or higher vs fewer than three MPS disc areas. (MPS disc areas are equivalent to 2.54 mm2 on the retina.9) Overall, 46% of the eyes had reading rates of ≥50 words/min. For the group with the smaller area of GA, 80% (eight of 10 eyes) had reading rates of ≥50 words/min. In the group with the larger area of GA, 28% (five of 18 eyes) had reading rates of ≥50 words/min (difference between groups significant, P = .007, with chi-square test). In both groups, no eye that fixated with the scotoma to the left had a reading rate of ≥50 words/min. For eyes fixating with the scotoma to the right, the reading rate was ≥50 words/min in 100% (five of five eyes) for the small GA area and 38% (three of eight eyes) for the large GA area group. The comparable findings for eyes that fixated with the scotoma above fixation were 100% (one of one eye) for the small area group and 33% (one of three eyes) for the large area group. None of the three eyes with spared centers that were surrounded by atrophy (all with GA areas of three or more MPS disc areas) had a reading rate of ≥50 words/min.
Figure 3.
Reading rate as a function of area of atrophy, coded for fixation pattern. Reading rate in words/min (wpm) as a function of the area of the atrophy Macular Photocoagulation Study (MPS) disc areas. The symbols for each eye are coded for the fixation pattern that was present, as noted in the figure. Central = Fixation appears to be at (or near) the foveal center, generally surrounded by multifocal geographic atrophy; I = fixation with the scotoma below (inferior to) fixation in visual field space; L = fixation with the scotoma to the left of fixation; No fix = no fixation site was demonstrated; R = fixation with the scotoma to the right of fixation; S = fixation with the scotoma above (superior to) fixation in visual field space; Sp = fixation is in a spared region within the atrophy.
TABLE 5.
Eyes With Central Scotomas From Geographic Atrophy Associated With Age-Related Macular Degeneration, With Visual Acuity 20/80–20/200 at Baseline: Baseline Reading Rate as a Function of Fixation Pattern, Stratified by Size of Geographic Atrophy (GA)
| GA area <3 MPS Disc Areas (n) |
GA area ≥3 MPS Disc Areas (n) |
|||
|---|---|---|---|---|
| Fixation Pattern | Reading Rate ≥50 wpm | Reading Rate <50 wpm | Reading Rate ≥50 wpm | Reading Rate <50 wpm |
| Central* | 1 | 1 | 0 | 0 |
| Spared† | 0 | 0 | 0 | 3 |
| No fixation‡ | 0 | 0 | 1 | 0 |
| R§ | 5 | 0 | 3 | 5 |
| L∥ | 0 | 1 | 0 | 3 |
| S¶ | 1 | 0 | 1 | 2 |
| I# | 1 | 0 | 0 | 0 |
| Total (%) | 8 (80) | 2 (20) | 5 (28) | 13 (72) |
Overall, 13 of 28 eyes (46%) had reading rates of ≥50 wpm. The distribution of reading rates between the two area groups is statistically significant (chi-square test, P = .007). wpm = Words per minute.
Fixation appears to be at (or near) the foveal center, with multifocal GA surrounding it.
Fixation is in a spared region within the atrophy.
No fixation site was demonstrated.
Fixation with the scotoma to the right of fixation.
Fixation with the scotoma to the left of fixation.
Fixation with the scotoma above (superior to) fixation in visual field space.
Fixation with the scotoma below (inferior to) fixation in visual field space.
During follow-up evaluation, the area of atrophy enlarged in all patients. At baseline, the mean atrophic area was four MPS disc areas (median, 3.6; range, 0.9 to 11.7). At the final follow-up visit, the mean atrophic area was 9.1 MPS disc areas (median, 8.1; range, 2.1 to 22.8). Twenty-three of the eyes had reading measured both at the baseline and the final visits. Table 6 shows the change in reading rate from the baseline to the final visit. For eyes with a baseline reading rate of ≥50 words/min, 67% of the eyes (eight of 12 eyes) had a reduction in reading rate; 58% of the eyes (seven of 12 eyes) were still reading at a rate of ≥50 words/min at the final visit. For eyes with a baseline reading rate of <50 wpm, 82% of the eyes (9 of 11 eyes) had a reduction in reading rate. Thus, even within an individual who already has a central scotoma, further enlargement of the atrophy is associated with further reduction in reading rate.
TABLE 6.
Eyes With Central Scotomas From Geographic Atrophy Associated With Age-Related Macular Degeneration, With Visual Acuity 20/80–20/200 at Baseline: Change in Reading Rate as a Function of Baseline Fixation Pattern, Stratified by Baseline Reading Rate
| Baseline Reading Rate ≥50 wpm (n) |
Baseline Reading Rate <50 wpm (n) |
Baseline Reading Rate ≥50 wpm (n) |
||||
|---|---|---|---|---|---|---|
| Fixation Pattern | Final Reading Rate Same or Better Than Baseline | Final Reading Rate Worse Than Baseline | Final Reading Rate Same or Better Than Baseline | Final Reading Rate Worse Than Baseline | Final Reading Rate ≥50 wpm | Final Reading Rate <50 wpm |
| Central* | 0 | 1 | 0 | 1 | 0 | 1 |
| Spared† | 0 | 0 | 0 | 2 | 0 | 0 |
| No fixation‡ | 0 | 1 | 0 | 0 | 0 | 1 |
| R§ | 2 | 5 | 0 | 4 | 4 | 3 |
| L∥ | 0 | 0 | 1 | 2 | 0 | 0 |
| S¶ | 1 | 1 | 1 | 0 | 2 | 0 |
| I# | 1 | 0 | 0 | 0 | 1 | 0 |
| Total (%) | 4 (33) | 8 (67) | 2 (18) | 9 (82) | 7 (58) | 5 (42) |
26% of all eyes had final reading rate the same or better than baseline.
Fixation appears to be at (or near) the foveal center, with multifocal GA surrounding it.
Fixation is in a spared region within the atrophy.
No fixation site was demonstrated.
Fixation with the scotoma to the right of fixation.
Fixation with the scotoma to the left of fixation.
Fixation with the scotoma above (superior to) fixation in visual field space.
Fixation with the scotoma below (inferior to) fixation in visual field space.
DISCUSSION
THE VALUE OF A PRL
The use of a PRL in patients with central scotoma contributes importantly to the optimal use of their remaining vision.1 Visual acuity may improve when a patient adopts a PRL,10 and the effectiveness of low-vision devices may be enhanced. Research is beginning, with functional magnetic resonance imaging and other techniques, to determine whether there is remapping of the primary visual cortex that formerly served the now silent foveal area and whether this remapping enhances the use of the PRL as a “pseudofovea.”11
Our study shows that the PRL remains stable over a follow-up period of >4 years in most patients. Thus, once the patient adopts techniques for the use of a PRL, whether consciously or unconsciously, the technique adopted (looking to the right, or looking up, for example) is likely to be continued over time, with only minor modifications of the degree of eccentric movement needed (Figure 1).
THE LOCATION OF THE PRL
The patients that were assessed continued to fixate predominantly with the scotoma to the right, as we showed in the 1996 study.4 In that study, we found that this preferred fixation pattern overrode factors such as the distance from the fovea to the PRL and the fact that, for left eyes, this fixation pattern involves putting the PRL between peripapillary atrophy and macular atrophy in some patients. The preference for fixation with the scotoma to the right was also seen in the final fixation pattern of eyes that had no eccentric PRL at baseline (number 4 in Table 3). In other groups of patients, with central scotomas from choroidal neovascularization, macular holes, or Stargardt disease, fixation is with the scotoma superior to fixation in most patients.2– 6,12 The pattern of fixation with the scotoma superior was the second most common pattern at the final evaluation of patients in our study. One hypothesis is that, as GA progresses, it is more common for a strip of retina to be spared horizontally, so that a patient becomes used to using the horizontal spared strip and then keeps the PRL at a similar horizontal location as the fovea, by placing it so that the scotoma is to the right or to the left of fixation. The preference for the scotoma to the right, rather than to the left, may be dependent on reading, because one study showed that, in contrast to our findings, readers of languages that are read right to left prefer fixating with the scotoma to the left.13
The SLO measured the patient’s fixation when the patient is viewing monocularly. One assumes that the monocular fixation data represent the binocular fixation pattern, at least for the better seeing eye, but this may not be the case.14,15 Certainly for eyes with noncorresponding PRLs, at least the worst eye cannot be fixating with the monocular PRL at the same time that the better eye is fixating with its monocular PRL. Our study showed that 10 of 13 patients (77%) with PRLs in each eye at baseline had the same pattern of fixation in both eyes (Table 3). Patients with the same fixation pattern in both eyes maintained corresponding fixation patterns over the follow-up period. Of the three patients who had different fixation patterns in each eye at baseline, one patient had adopted the same fixation pattern in both eyes by the final visit.
Fixation behavior was assessed for only a single task: fixating a high-contrast cross. This behavior generally correlated with the way the patient read the acuity chart. That is, patients who fixated with the scotoma to the right in the SLO tended to miss the last letters on the line, unless they looked further to the right to move the scotoma away. Fixation behavior while reading single words or paragraphs was not tested systematically. Patients with a partially spared central region may shift fixation to a peripheral PRL when a low-luminance cross is used.16 Likewise, it is not known whether the patient adopts the same pattern when walking or when looking at a large scene. Nonetheless, this is the method that has been used consistently for defining the PRL, and our findings support the persistence of a stable pattern over time.
For this study, the location of fixation was assessed by the position of the fixation cross on the image saved at the conclusion of SLO testing and by written comments by the examiner during the course of the testing. Because different SLOs with different software were used at different points in the study, a quantitative analysis of fixation was not possible. However, as noted in the past, the data on fixation stability that were obtained from the degree of change of position of the retinal landmark each time a stimulus are presented, and the image that is grabbed is necessarily an underestimate of instability.8 This is because the examiner generally waits until the eye has stabilized or coaches the patient to look at the cross before the stimulus is presented.
These patients did not undergo eccentric fixation training or systematic low vision intervention in terms of scotoma awareness training, although the SLO findings that were related to their fixation were explained to the patient. The degree to which an eccentric PRL can be trained17 and whether a trained PRL will be stable over time cannot be answered from this study.
READING AND PRL LOCATION
Although the numbers are small, the data (Table 5) suggest that patients who fixate with the scotoma to the right of fixation or above fixation have better reading rates than patients who fixate with the scotoma to the left. Thus, these two fixation patterns not only are the most prevalent, but they also seem to confer an advantage in reading rate. As noted, this agrees with the findings of others, although it runs counter to evidence from simulated scotomas that the visual span to the right is more important.18,19 These data must be taken into account when consideration is given to training a PRL. (A single patient in this study fixated with the scotoma below fixation and had a good reading rate, but this pattern is extremely uncommon and would likely confer no reading advantage in general.) It is possible that anchoring oneself at the beginning of a line is more important than the refixations that are necessary to move the scotoma further to the right as a line is read.
PROGRESSIVE WORSENING OF READING RATE OVER TIME
Two analyses provide evidence that an enlargement in the area of atrophy is associated with a reduction in reading rate. First, the cross-sectional analysis shows a strong inverse relationship between the size of the GA and the reading rate. Second, 74% of eyes in this study continued to worsen in reading rate as the atrophy enlarged over time. Both of these analyses, along with the data in Table 4 that show continued loss of visual acuity imply that an intervention that could slow or halt the further enlargement of atrophy would confer benefit in terms of reading rate, even when the acuity is in the 20/80 to 20/200 range and even when the fovea is already lost.
LIMITATIONS OF THIS STUDY
The chief limitation of this study is that we relied on a single image that showed the fixation location and our written notes that described fixation during testing to define the location of the PRL. More precise statistical data would require analysis of fixation behavior throughout the testing session, with the construction of a bivariate ellipse enclosing most of the fixations, or the use of other statistical means of expressing the location and variation of fixation. This was done as thoroughly as possible and was described in a previous article.8 The procedure was tedious and time-consuming and had limitations. For this study, fixation data to quantitatively measure fixation stability were not available, in part because of the different machines that were used and in part because of inadequate manpower to do the necessary data analysis. We were thorough in reporting the nature of the fixation that was demonstrated in each SLO session and had a form on which this was queried. For this study, we therefore have been fairly general in defining the fixation pattern; for example, fixation with the scotoma to the right could mean anywhere between the 2 o’clock and 5 o’clock positions. Because patients, of necessity and with consistency, moved their PRL more eccentrically as the atrophy enlarged, there was bound to be a change in the exact location of the PRL, even when the pattern remained the same. Likewise, we could not determine the quantitative correlation between the fixation pattern that was used in the every day world as compared with the fixation pattern in the SLO. The SLO findings generally corresponded to the way that the patient read the eye chart; for example, a patient with a scotoma to the right of fixation would be expected to find the final letters on a line more difficult to read, but we did not always capture this behavior on our data sheets.
Two other limitations are the relatively small number of patients who were included and the fact that the length of follow-up time was not uniform. Nonetheless, the data form a consistent picture of PRL behavior over time.
Acknowledgments
Supported by National Institutes of Health grants EY08552 and EY14148 and the Research to Prevent Blindness Physician Scientist Merit Award (J.S.S.).
Footnotes
Presented in part at the 2004 annual meeting of the Association for Research in Vision and Ophthalmology, April 25–29, 2004, Fort Lauderdale, Florida.
REFERENCES
- 1.White JM, Bedell HE. The oculomotor reference in human with bilateral macular disease. Invest Ophthalmol Vis Sci. 1990;31:1149–1161. [PubMed] [Google Scholar]
- 2.Guez J-E, Gargasson J-FL, Rigaudiere F, O’Regan JK. Is there a systematic location for the pseudo-fovea in patients with central scotoma? Vision Res. 1993;9:1271–1279. doi: 10.1016/0042-6989(93)90213-g. [DOI] [PubMed] [Google Scholar]
- 3.Acosta F, Lashkar K, Reynaud X, et al. Characterization of functional changes in macular holes and cysts. Ophthalmology. 1991;98:1820–1823. doi: 10.1016/s0161-6420(91)32044-x. [DOI] [PubMed] [Google Scholar]
- 4.Sunness JS, Applegate CA, Haselwood D, Rubin GS. Fixation patterns and reading rates in eyes with central scotomas from advanced atrophic age-related macular degeneration and Stargardt’s disease. Ophthalmology. 1996;103:1458–1466. doi: 10.1016/s0161-6420(96)30483-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rohrschneider K, Gluck R, Blankenagel A, Volcker HE. Fixationsverhalten bei Morbus Stargardt. Ophthalmologe. 1997;94:624–628. doi: 10.1007/s003470050171. [DOI] [PubMed] [Google Scholar]
- 6.Fletcher DC, Schuchard RA. Preferred retinal loci: relationship to macular scotomas in a low-vision population. Ophthalmology. 1997;104:632–638. doi: 10.1016/s0161-6420(97)30260-7. [DOI] [PubMed] [Google Scholar]
- 7.Sunness JS, Rubin GS, Applegate CA, et al. Visual function abnormalities and prognosis in eyes with age-related geographic atrophy of the macula and good acuity. Ophthalmology. 1997;104:1677–1691. doi: 10.1016/s0161-6420(97)30079-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sunness JS, Schuchard R, Shen N, et al. Landmark-driven fundus perimetry using the scanning laser ophthalmoscope (SLO) Invest Ophthalmol Vis Sci. 1995;36:1863–1874. [PMC free article] [PubMed] [Google Scholar]
- 9.Littmann H. Determination of the true size of an object on the fundus of the living eye. By: Littmann H, from the original article, “Zur Bestimmung der wahren Grosse eines Objektes auf dem Hintergrund des lebenden Auges,” which originally appeared in Klinisches Monatsblatter fur Augenheilkunde 1982;180:286–9. Translated by Williams TD. Optom Vis Sci. 1992;69:717–720. doi: 10.1055/s-2008-1055068. [DOI] [PubMed] [Google Scholar]
- 10.Sunness JS, Applegate C, Gonzalez-Baron J. Improvement of visual acuity over time in patients with bilateral geographic atrophy from age-related macular degeneration. Retina. 2000;20:162–169. [PubMed] [Google Scholar]
- 11.Sunness JS, Liu T, Yantis S. Retinotopic mapping of visual cortex using fMRI in a patient with central scotomas from atrophic macular degeneration. Ophthalmology. 2004;111:1595–1598. doi: 10.1016/j.ophtha.2003.12.050. [DOI] [PubMed] [Google Scholar]
- 12.Trauzettel-Klosinski S, Tornow RP. Fixation behavior and reading ability in macular scotoma. Neuro-ophthalmology. 1996;16:241–253. [Google Scholar]
- 13.Guez J-E, Le Gargasson J-F, Rigaudiere F, et al. Relation between reading and preferred retinal locus in patients with central scotoma. presented at the 1995 SLO meeting in San Antonio, Texas. [Google Scholar]
- 14.Labianca AT, et al. Monocular preferred retinal loci are inconsistent with binocular viewing. International Conference on Low Vision; 1996. pp. 381–387. [Google Scholar]
- 15.Schuchard RA, Cummings R, Ross D, Watson G. Comparison of SLO perimetry, binocular perimetry, and functional visual field perimetry in patients with macular scotomas. Invest Ophthalmol Vis Sci. 2003;44 ARVO E-Abstract 2778. [Google Scholar]
- 16.Lei H, Schuchard RA. Using two preferred retinal loci for different lighting conditions in patients with central scotomas. Invest Ophthalmol Vis Sci. 1997;38:1812–1818. [PubMed] [Google Scholar]
- 17.Nilsson UL, Frennesson C, Nilsson SE. Patients with AMD and a large absolute central scotoma can be trained successfully to use eccentric viewing, as demonstrated in a scanning laser ophthalmoscope. Vision Res. 2003;43:1777–1787. doi: 10.1016/s0042-6989(03)00219-0. [DOI] [PubMed] [Google Scholar]
- 18.Fine EM, Rubin GS. Reading with simulated scotomas: attending to the right is better than attending to the left. Vision Res. 1999;39:1039–1043. doi: 10.1016/s0042-6989(98)00208-9. [DOI] [PubMed] [Google Scholar]
- 19.Rayner K, Wall AD, Pollatsek A. Asymmetry of the effective visual field in reading. Percept Psychophys. 1980;27:537–544. doi: 10.3758/bf03198682. [DOI] [PubMed] [Google Scholar]