Summary
The prevalence of overweight among children has doubled within the past two decades. Increases in the rate of childhood overweight are of particular concern due to the negative health and psychological effects noted among overweight children. As shown by previous research, the development of childhood overweight involves a complex set of factors from multiple contexts that interact with each other to place a child at risk of overweight. This multifaceted system can be conceptualized using Ecological Systems Theory (EST). EST highlights the importance of considering the context(s), or ecological niche, in which a person is located in order to understand the emergence of a particular characteristic. In the case of a child, the ecological niche includes the family and the school, which are in turn embedded in larger social contexts including the community and society at large. In this review, EST is used as a framework with which to summarize research assessing predictors of childhood overweight. Specifically, child characteristics that place children at risk of the development of overweight (including dietary intake, physical activity, and sedentary behaviour) will be reviewed while taking into consideration the influence of the familial environment, the school environment, and the community and larger social environments. It is concluded that future research needs to adopt a broader contextual approach in order to understand and intervene against the processes leading to the development of overweight among children and that the use of theories or paradigms such as EST will facilitate developing and testing models of causal processes.
Keywords: Children, obesity, overweight, family, context
Introduction
In the past two decades, a twofold increase has been noted in the rate of obesity among children; today, approximately 25% of US children between the ages of 6 and 17 years are overweight or at risk of overweight (1). Heightened rates of overweight are also noted among preschool-aged children, particularly 4–5-year-old girls (2). Consequently, childhood overweight is regarded as the most prevalent nutritional disease among US children and adolescents (3). Childhood overweight has been associated with negative health consequences including non-insulin dependent diabetes, hypertension, and sleep apnea (3), and negative psychological outcomes including depression (4), disturbed body image (5,6) and low self-concept (7,8). Due the negative consequences associated with childhood overweight, research assessing its causes is of utmost importance in order to guide the development of treatment and prevention programmes.
Research assessing behavioural correlates of childhood overweight has increased dramatically in the past 10 years. Although this surge of interest has increased our understanding of predictors of childhood overweight, the resulting body of research is limited primarily to a series of simple, or bivariate, relationships. Future research needs to move beyond bivariate relationships and develop a comprehensive model of the factors implicated in the development of childhood overweight, such as children’s dietary and activity patterns, parenting practices that shape children’s dietary and activity practices, and the environment in which parenting takes place. This model should also incorporate child characteristics, such as gender and age, that influence parenting practices and moderate the impact of risk factors on the development of overweight. Such a model could serve as a useful heuristic device to promote the investigation of the complex multifactorial aetiology of childhood overweight and facilitate the development of effective intervention and prevention programmes. Ecological Systems Theory presents an effective tool with which to develop such a model. The usefulness of EST will be illustrated by using it as a framework to evaluate and integrate research assessing risk factors for childhood overweight including children’s dietary intake, physical activity, and sedentary behaviour and to consider familial and societal characteristics that influence the emergence of child risk behaviours.
Ecological systems theory
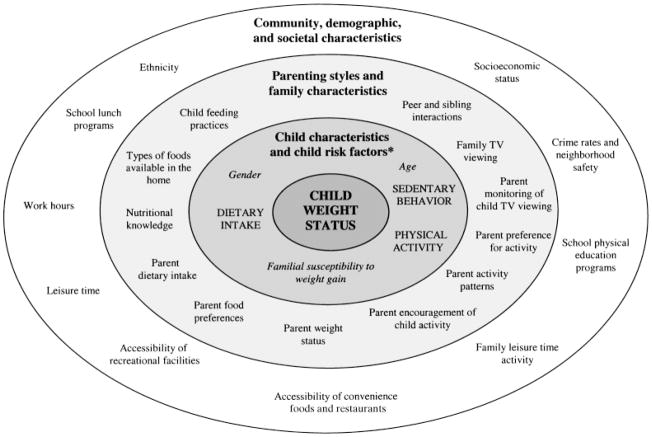
Ecological Systems Theory (EST) conceptualizes human development from an interactive contextual perspective (9,10). According to EST, development, or change in individual characteristics, cannot be effectively explained without consideration of the context, or ecological niche, in which the person is embedded. An ecological niche includes not only the immediate context in which a person is embedded, but also the contexts in which that context is situated. In the case of a child, the ecological niche includes the family and the school, which are in turn embedded in larger social contexts including the community and society in general. In addition to these larger contexts, characteristics particular to the child, such as gender and age, interact with familial and societal characteristics to influence development. To summarise, according to EST, development occurs as a result of interactions within and among these contexts; that is, characteristics of the child interact with processes in the family and the school, which themselves are influenced by characteristics of the community and society at large. The application of EST to predictors of childhood overweight is illustrated in Fig. 1.
Figure 1.
Ecological model of predictors of childhood overweight. ✽=Child risk factors (shown in upper case lettering) refer to child behaviours associated with the development of overweight. Characteristics of the child (shown in italic lettering) interact with child risk factors and contextual factors to influence the development of overweight (i.e. moderator variables). This review is organized around child risk factors and the influence of child family, and community characteristics is discussed for each child risk factor.
Predictors of childhood overweight
Figure 1 presents a model of the development of childhood overweight based on the results of research assessing predictors of childhood overweight in combination with EST. According to this model, child behavioural patterns such as dietary intake, physical activity, and sedentary behaviour (such as TV viewing) can place a child at risk of overweight (shown in upper case lettering in Fig. 1); these factors will be referred to as ‘child risk factors’. The impact of child risk factors on the development of overweight is moderated by child characteristics including age, gender, and susceptibility to weight gain (shown in italic lettering in Fig. 1). The development of child risk factors is shaped by parenting styles and family characteristics, such as parents’ dietary intake and activity patterns, nutritional knowledge, child feeding practices, and peer and sibling interactions. Characteristics of the school environment, such as structured periods for activity and the dietary quality of school lunches, and community, demographic, and larger environmental factors, such as parent work-related demands (i.e. work hours and leisure time), ethnic background and the availability and accessibility of recreational facilities, influence child weight status as a result of their influence on parenting practices and children’s daily eating and activity behaviours.
The model outlined in Fig. 1 is similar to a widely used theoretical model established by United Nations Children’s Fund (UNICEF) that describes causes of childhood malnutrition (11). In the UNICEF model, malnutrition occurs as a result of a compilation of factors including inadequate dietary intake by the child, which is due to household or family level factors such as insufficient access to food and poor water sanitation, which themselves occur as a result of societal level factors such as a lack of potential resources and limits in technology. The main difference between these two models is that EST outlines bi-directional, rather than uni-directional, relationships among the different levels of influence and considers how factors at one level moderate the influence of factors from another level.
Research relating to the model of childhood overweight presented in Fig. 1 is reviewed below. Specifically, research relating to each of the child risk factors (i.e. dietary intake, activity patterns, and sedentary behaviour) is reviewed in turn and the influence of (a) child characteristics (b) parenting styles and family characteristics, including peers, and (c) community and demographic characteristics, including the schooling system, are considered for each child risk factor. The primary goal of this review is to highlight the necessity of addressing characteristics of the child and the familial and societal contexts in which the child is embedded in order to understand the process by which childhood overweight develops. As a point of clarification, the term ‘weight status’ will be used as a collective term to refer to all measures of body composition.
Children’s dietary patterns
Children’s dietary patterns are central in the development of overweight as excess caloric intake, relative to energy expenditure, will result in the storage of energy as fat, eventually leading to excessive levels of fat in the body. In addition, high levels of fat may facilitate fat storage, as ingested fat is readily stored as fat in comparison to other macronutrients such as carbohydrate or protein (12). Children’s preference for fat, although less well understood, may also place children at risk of overweight as it may predispose children to consume high levels of fat. Research has identified links between children’s weight status and total energy intake, percentage of intake as fat, and fat preference. The consistency of results, however, varies by the predictor of interest.
Research has shown cross sectional links between total daily energy intake and child weight-for-length (13), skin-fold thickness (14) and obese vs. non-obese group status (15), with higher intake being associated with higher weight status. In addition, higher caloric intake has been associated with greater increases in children’s skinfold thickness across a period of a year (16) and greater increases in caloric intake have been associated with greater increases in children’s body mass index (BMI) (17). There is also a notable body of evidence that has failed to identify an association between energy intake and child weight status (18–20), or has found that children with higher weight status consume fewer calories relative to their weight (21). Discrepancies in the reported relationship between energy intake and weight status may be due to differences in the measurement of weight status and/or dietary intake and differences in the extent to which the energy needs of children were taken into consideration (i.e. bigger children have greater energy needs). Inconsistencies inherent in the results may also be explained by child characteristics such as age and gender, which are discussed below.
Cross sectional and longitudinal research provides more convincing evidence of a relationship between children’s percent fat intake and weight status. Higher percent fat intake among children has been concurrently associated with higher percentage body fat (18,21,22), fat mass (23), and skinfold thickness (18,24). Moreover, higher percent fat intake has been prospectively associated with greater increases in children’s skinfold thickness across a period of a year (16) and greater increases in BMI over 2 years (25). Finally, increases in children’s percent fat intake have been associated with greater increases in their BMI (25). Only one study among those identified failed to identify an association between children’s percent fat intake and weight status (19).
Relatively few studies have assessed the relationship between food preferences, food intake, and weight status among children. A preference for energy dense foods may serve as a risk factor in the development of overweight if consumption of these foods leads to excessive fat and energy intake. Conversely, a preference for fruits and vegetables may serve as a protective factor for the development of overweight. Fisher & Birch (26) and Ricketts (27) found that children with greater tricep skinfold thickness displayed a higher preference for fat and children’s preference for high fat foods was positively associated with fat intake. Similarly, Resnicow and co-workers (28) found that children’s consumption of fruit and vegetables was positively associated with their preference for fruit and vegetables. Unfortunately, the relationship between preference for fruits and vegetables and children’s weight status was not assessed in this study.
In summary, research illustrates cross sectional and longitudinal links between children’s dietary patterns and weight status, although findings are more consistent for children’s percent fat intake and preference for fat than for total energy intake. Inconsistencies in relationships identified may be explained by the difficulty in assessing children’s dietary intake patterns. In addition to problems noted in measuring dietary intake among adults (e.g. the inability to remember and accurately report all foods consumed, the restricted list of foods provided, and self-report biases), reports of children’s dietary intake are also limited by the fact that they are generally based upon reports from a third person – usually a parent (29). Inconsistencies in research to date may also be explained by the fact that research has rarely considered child characteristics that moderate the relationship between dietary patterns and weight status, the contexts in which children’s eating patterns emerge, and the processes by which such patterns emerge.
Child characteristics
The relationship between children’s dietary patterns and weight status is likely to differ as a function of children’s familial susceptibility to weight gain (i.e. number of overweight parents), rate of growth, and gender. Research in adults has shown that there is a large degree of interindividual variability in tolerance to overfeeding. In a study assessing responses to long-term overfeeding in humans, marked variability in weight gain was observed; some participants gained over 12 kilograms in body weight, whereas, others showed little change in body weight (30). In accordance with this, research has shown links between percent fat intake and increases in BMI among women predisposed to obesity (i.e. already overweight with ≥1 obese parent), but not among women without such an inclination (31). Although there is a virtual absence of research assessing the moderating effect of susceptibility to weight gain on the relationship between dietary intake and weight status among children, results from related areas of research suggest a similar pattern (32). In a dietary intervention study designed to reduce cholesterol levels in children, large individual differences were noted in the effectiveness of the programme. Specifically, children with a family history of heart disease were resistant to dietary intervention efforts to reduce their lipid levels in comparison to children with no family history of heart disease. These results suggest that children who are predisposed to obesity may be more susceptible to the effects of excessive energy and fat intake, with respect to weight gain, than children with no familial history of obesity.
Children’s energy needs differ as a function of their rate of growth and the timing of growth spurts differs for girls and boys (particularly during adolescence). Hence, rate of growth and gender are likely to interact with energy intake, and possibly percent fat intake, in influencing children’s weight status. This interaction may make results from studies that include children from a broad age range and combine results for girls and boys difficult to interpret and may explain the lack of consistency in research assessing the relationship between energy intake and weight status. Although research assessing links between children’s dietary patterns and weight status has often included measures of familial risk of overweight (i.e. parent weight status), gender, and age, these variables have generally been considered nuisance variables and their effects have been controlled for in analyses, rather than being directly examined.
Parenting styles and family characteristics
Children’s dietary patterns evolve within the context of the family. Not surprisingly, consistent similarities have been noted in child and parent patterns of dietary intake (33–37) and positive moderate associations have been found between the food preferences of children and parents (38). Although these studies highlight links between parent and child dietary patterns, they provide no information about the mechanisms by which these behaviours are linked. Similarities in parent–child dietary patterns may reflect genetic similarity in taste perception, food preferences, and hunger and satiety cues. Research, however, does not support a genetic explanation of familial dietary patterns; correlations in dietary patterns exist among individuals in the same household irrespective of whether or not they are genetically related (33,36). Therefore, parent–child intake patterns and preferences are likely to reflect environmental factors. There are numerous pathways by which parents may shape children’s dietary practices including parent nutritional knowledge, the types of foods parents make available to children, parental modelling of particular eating behaviours, and parent child-feeding practices (shown in the middle circle of Fig. 1).
Mothers’ nutritional knowledge and concern for disease prevention are positively associated with children’s fruit and vegetable intake (39) and negatively associated with children’s total energy and fat intake (40). Parents’ nutritional knowledge and health concerns may influence children’s eating patterns in a number of ways. Lack of knowledge of appropriate serving sizes may lead parents to overfeed children; research shows that serving children larger sized portion is associated with greater food intake (41). A focus on health may lead parents to purchase more healthful foods (i.e. fruits and vegetables) and make them more readily accessible in the home, which are both important determinants of children’s preference for (42) and intake of (43) such foods. It is likely that the reverse pattern is also true such that low nutritional knowledge is associated with greater accessibility to energy dense foods, which promotes the consumption of such foods, thereby increasing the risk of overweight.
Parents are likely social referents, or role models, for children’s eating behaviour. That is, it is probable that children will want to eat, and through repeated exposure, learn to like foods that they see their parents eating (42). Unfortunately, little research has comprehensively assessed the influence of parental modelling on children’s dietary patterns. Associations have been identified, however, between mothers’ and girls’ milk and soft drink intake (44) and between parents’ and girls’ fruit and vegetable intake (45).
Parents also shape children’s dietary patterns as a result of interactions that take place during feeding occasions. Infants are capable of regulating their caloric intake based on their physiological needs (46). Research suggests, however, that child feeding practices that are not responsive to children’s hunger needs may reduce this regulatory ability, possibly leading to excessive caloric intake. A lack of responsiveness to infant signals of distress, such as feeding a child every time he/she cries, may teach infants to associate eating with distress. Among children, excessive parental control of when, what, and how much children eat may teach children to ignore their feelings of hunger and may lead to increased levels of intake (46). Research has identified a positive association between parents’ control of children’s food intake, specifically restricting access to food, and children’s percentage of energy intake as fat (14). Parental restriction has also been linked to higher weight status among children (47). Encouragement to eat in the absence of hunger is an additional form of control in child feeding. Research shows that encouragement to eat is positively associated with children’s energy intake (48). Likewise, encouragement to eat is associated with the time children spend eating, which in turn is positively associated with their degree of fatness (49). Unfortunately, the directionality of the relationship between parental restriction and encouragement to eat and child weight status cannot be determined as all studies reviewed are based on cross-sectional data.
Control in the feeding domain may also promote children’s preference for particular foods. That is, parents may inadvertently promote children’s liking for energy-dense foods as a result of restricting access to such foods and using them to shape children’s behaviour. Research shows that restricting children’s access to particular foods increases children’s preference for and consumption of such foods when restriction is removed (47,50). In addition, pre-school children’s preference for a snack food has been found to increase when used as a reward for positive behaviour or when simply paired with adult attention (51). When one considers that practices of restriction and reward are most likely to involve energy dense snack foods, these parenting behaviours may increase children’s risk of overweight by increasing the likelihood of over-consumption of such foods.
Each of the parenting factors outlined above is likely to reflect parents’ weight status. That is, overweight parents may be more likely to adopt practices that place their child at risk of overweight, thereby perpetuating the familial lineage of overweight. Research shows that mothers with higher weight status are more likely to give their children snacks of low nutrient density (i.e. high energy density) (52). Similarly, children with overweight mothers are likely to consume more fat as a proportion of food intake in comparison to children of non-overweight mothers (23). Finally, according to Costanzo & Woody (53), parents who are themselves overweight are more likely to use controlling feeding practices due to increased investment in the child’s weight status. These associations highlight the cyclical relationships among parent weight status, parenting practices, children’s eating behaviours, and children’s weight status.
Finally, children’s food preferences and dietary patterns may be shaped by interactions with peers and siblings. In one of the few studies that have assessed this possibility, Birch (54) found that children aged 2–5 years changed their food preferences, and consumed more of a non-preferred food, when repeatedly exposed to children with preferences differing from their own. That is, children changed their preferences to coincide with those of their peers. The effect of peers on children’s food preferences was still evident 1–8 weeks after the procedure, thus suggesting long-term changes in preferences. Research, however, has rarely considered the impact of siblings on children’s food preferences and dietary patterns and how this might differ from the effect of same age peers.
Community, demographic and societal characteristics
Parent child-feeding practices shape children’s dietary practices and are in turn influenced by larger community, demographic, and societal characteristics such as work demands, ethnicity, socioeconomic status (SES), and the availability of convenience foods (shown in the outer circle in Fig. 1). In addition, children’s dietary patterns are influenced by systems outside the family that do not directly influence parenting styles, such as school or childcare facilities.
The types of foods parents feed children are likely to reflect the time that parents have available for food preparation (in addition to factors previously outlined such as nutritional knowledge). Time available for food preparation has been greatly reduced due to increases in the number of hours that mothers and fathers work. Decreases in leisure time, coupled with the lack of a desire to spend what free time is available preparing food, have resulted in major shifts in dietary practices. There has been a shift away from the consumption of fruit, vegetables, and grains and a large increase in the use of pre-made and convenience foods (including eating out), which are generally high in fat (55,56). Frequent exposure to convenience foods has been associated with higher weight status among adults (57), and is likely to show a similar relationship among children. The types of food parents provide for children may also reflect foods available in supermarkets; the relative availability of healthful and non-healthful foods in supermarkets has been linked to individual diet quality (58).
Ethnic and SES differences have been noted in children’s dietary patterns. Results from the 1987–88 Nationwide Food Consumption Survey showed that African-American children had higher levels of fat intake than children of other ethnic groups (59). In addition, research shows that children from lower SES groups have less diverse diets than children from upper SES groups (60); similarly, lower educational status among fathers has been associated with higher fat intake among children (18). Dietary differences among children from different SES and ethnic groups may reflect differences in parents’ attitudes and beliefs, which in turn shape their feeding practices. Research consistently shows that African-American women, and African-American women of low SES, choose larger ideal body shapes and have less strict criteria for perceived fatness in comparison to white women (61–63). Similarly, mothers’ of low SES are more likely to rate chubbier babies as ideal in comparison to high SES mothers (64). These differences are likely to influence mothers’ feeding practices and their perceptions of their child’s weight status. In a sample of African-American mothers, only 44% perceived their child’s weight to be a potential problem, although 57% of children were obese and 12% were superobese (65). Research from a focus group of low-income and ethnic minority mothers (66) showed that mothers considered a fat baby a healthy baby and a thin baby a reflection of neglectful parenting. In addition, convenience was important for mothers when preparing foods for their children, and mothers believed that it cost less to purchase convenience foods.
Finally, the school environment is an important context in the development of children’s dietary practices as children consume a substantial proportion of their daily intake at school; one study found that school lunches provided approximately 40% of children’s basic food group consumption for the day and 40% of the different foods eaten in a day were eaten at school (60). Most of the research assessing the relationship between school lunch programmes and children’s dietary practices is from intervention studies. Results from intervention research suggest that children’s daily fat intake is influenced by the fat content of school diets (67) and that daily intake of fruits and vegetables varies based on their availability in school lunch programmes (43).
Children’s activity patterns
In addition to children’s dietary intake, children’s physical activity may be associated with risk of overweight (shown in capitals in Fig. 1). High levels of physical activity could compensate for excessive caloric or fat intake, thereby allowing the maintenance of a healthy weight status. Yet marked reductions have been noted in levels of physical activity among adults and children. In a recent survey assessing children’s activity levels, only 36% of children met the year 2000 goal for strenuous activity (68). Consequently, it is frequently postulated that changes in levels of physical activity partially explain increases in the prevalence of overweight among children.
Research shows that lower levels of physical activity and habitual exercise among children are associated with higher BMI (24), greater skinfold thickness (24,69), greater fat mass (70), and obese status (71,72). Similarly, lower levels of fitness have been associated with an increased likelihood of being overweight (73). In addition to concurrent associations between physical activity and weight status, research shows that physical activity and habitual exercise among children are associated with decreased BMI, taking growth into consideration (17,25,74), and decreased body fat (75). Only two studies of those identified failed to find an association between physical activity and weight status in children or adolescents (21,76). A recent review by Sallis and co-workers (77) concluded that there is an indeterminate relationship between weight status and physical activity among children and adolescents, however, physical activity was the outcome measure of interest in their review rather than the predictor variable of interest (as was the case in the studies reviewed above).
The relative consistency of the relationship between physical activity and weight status, where weight status is the outcome measure, is surprising considering the validity and reliability problems noted in measures assessing physical activity among children, particularly self-report measures (29,78). Consequently, the relationships identified are likely to underestimate the true relationship between activity and weight status and the importance of activity in reducing rates of overweight among children. Children’s activity patterns are shaped by a combination of child characteristics, and parent and peer activity patterns, which are in turn shaped by broader contextual factors such as SES, the availability of recreational facilities, and school physical education programmes. Each of these domains of influence will be reviewed in turn.
Child characteristics
Child characteristics such as gender and age influence the likelihood of participating in physical activity and sport and may differentially influence the benefits of physical activity on the maintenance of a healthy weight status (shown in italics in Fig. 1). Research provides overwhelming evidence of sex differences in physical activity; boys are in general more physically active, and more physically fit, than girls (77,79–83). In addition, there appears to be a developmental decline from childhood to adolescence in participation in sports and exercise (82) and this decline is greater for girls (81). Decreases in physical activity with increasing age may reflect developmental decreases in arousal levels and increases in alternative interests and demands on time. In addition, age-related decreases in activity may be explained by the onset of puberty and its associated physical, emotional, and social changes (80). Pubertal development, in combination with an increase in self-awareness, may make adolescents reluctant to put themselves in situations where physical changes may be noticeable. Finally, gender differences in activity participation and developmental increases in such differences may be explained by the perception among girls that sports and physical activity are unfeminine (84), and a strengthening of this belief as girls approach puberty (81).
Parenting styles and family characteristics
As with dietary patterns, children’s activity patterns and activity preferences are shaped within the context of the family. Parent participation in physical activity is positively related to activity among children and adolescents (83,85–88). This relationship is also evident when parent and child activity are measured using accelerometers (89,90), rather than self-report questionnaires. Links between parent and child activity patterns may reflect the importance of parents as social models for children’s preferences and behavioural patterns. Parent–child associations in activity may also reflect the fact that parents who are active are more likely to enjoy activity and believe in the positive health and emotional benefits of activity (91, Davison & Birch, unpublished data). Parents with such beliefs may be more likely to create an environment that promotes activity by encouraging their children to be active and by enrolling their children in sporting events and driving them to and from such activities, both of which have been linked to increased levels of activity among children (48,93).
Parent participation in activity may be most influential on activity patterns among ‘high risk’ groups who show relatively low levels of activity and are at greater risk of weight gain. A number of studies suggest that parent activity has a greater influence on the activity patterns of girls in comparison to boys (84,85,87). Parents may be particularly influential in shaping girls’ activity patterns because girls are exposed to fewer role models outside the family in comparison to boys. Likewise, research shows that children of overweight parents benefit most from parent participation in sport. In a study by Klesges and co-workers (94), parent participation in activity had a large positive effect on activity levels for children with two overweight parents and little effect for children with no overweight parents.
Activity patterns among peers may also shape children’s inclination toward, and participation in, physical activity. In a study including children from nine European nations, sport participation by best friends was more strongly associated with subjects’ sport participation than sport participation of family members (88). It is also likely that the influence of peers, in particular same sex peers, may be greater among adolescents than younger children due to the increased importance of peer relations during adolescence (83,95) and increased sport or activity-related friendships. Research, however, has rarely assessed age differences in the influence of peers on activity.
Community, demographic, and societal characteristics
Children’s activity is influenced by the encouragement and support that they receive from their parents and their parents’ own activity patterns, which are in turn influenced by the time parents have available for such pursuits, the accessibility of recreational facilities, the availability of safe activity areas, ethnicity, and SES. In addition, children’s activity patterns are influenced by the structure of school physical education programmes (refer to the outer circle of Fig. 1).
A lack of time is consistently noted as a barrier to being active (92). Due to increases in the number of hours that parents work outside the home, parents have less time available for their own physical activity and to support their children’s activity. Likewise, the ability for parents to use sport as a form of family recreation has declined. Access to walking and bicycling paths, parks, and general recreational facilities has decreased due to urban sprawl and greater distances of such facilities from the home. Consequently, it is often not possible for families to be active without considerable effort.
Ethnicity and SES influence the likelihood of activity among children. Higher levels of activity have been observed among non-Hispanic white children in comparison to Asian, Hispanic, and African-American children (68,77,87,96,97). Lower levels of activity among ethnic minorities may be explained by less of a desire to be thin and less of a belief that exercise can aid weight loss or weight maintenance (98). Ethnic differences in exercise patterns may also be explained by differences in SES. Higher levels of activity have consistently been noted among high SES groups relative to lower SES groups (79,83,87,99). Research suggests that ethnic differences in activity, but not fitness, are no longer apparent when SES is held constant (80). Physical activity may be lower among children from low SES families due to parent characteristics such as less leisure time, less knowledge of the benefits of exercise as a result of lower levels of education (100), and fewer financial resources to support children’s sporting activities. Finally, ethnic and SES differences in physical activity may be explained by differences in neighbourhood safety, with fewer safe recreation areas being available in neighbourhoods with a large proportion of low SES and ethnic minority families.
Schools provide a rich opportunity to expose children to a variety of physical activities. Changes in the school system, however, have negatively impacted upon the provision of such opportunities. Physical education often receives a low priority in school budgets. As a result, many schools no longer provide physical education during the school day (55); in 1997 only 27.4% of children attended physical education class daily (101). This rate is likely to be even lower today. In addition, lunch and recess breaks have been reduced in many schools due to time demands and greater pressure for higher academic grades. Research shows that children who report no physical education class during school have less physical activity overall (82). Likewise, participation in daily physical education classes is associated with higher levels of moderate to vigorous physical activity among adolescents (96). School-based intervention programmes (including Sports, Play and Active Recreation for Children (SPARK) and Child and Adolescent Trial for Cardiovascular Health (CATCH)) designed to increase physical activity levels among children have had no effect on children’s weight status, although they have been successful in increasing levels of activity (67,102). There are a number of possible explanations for these findings. Activity may lead to an increase in lean body mass and a decrease in fat mass, resulting in unchanged weight. Periods of physical activity may be offset by periods of inactivity. Finally, activity patterns both inside and outside of school may be important in influencing children’s weight status.
Children’s sedentary behaviour
The final child risk factor to be reviewed is children’s sedentary behaviour (shown in capitals in Fig. 1). In contrast to high levels of activity, which may protect children from the development of overweight, sedentary behaviours such as TV viewing, may place children at risk of overweight. US children and adolescents watch approximately 3 hours of television a day (103). Possible reasons for such high rates of TV viewing include the ready accessibility of televisions, the increasingly child-centred nature of programmes, a lack of monitoring by parents, a lack of outdoor play areas, unsafe neighbourhoods, and the planned use of television by parents as an electronic baby-sitter. Due to the co-occurrence of population-level increases in TV viewing and childhood obesity, concern has been voiced that TV viewing, and other sedentary behaviours such as watching videos and playing computer games, may explain increases in childhood overweight.
Recent research provides a persuasive body of evidence linking sedentary behaviour and children’s weight status. Among children, a greater number of hours spent in sedentary pursuits has been associated with a higher prevalence of overweight (72,73,104,105), higher BMI (19,24,106), and greater skinfold thickness (24,106). Likewise, higher levels of sedentary behaviour have been associated with greater increases in BMI across a period of a year (17). In a randomized controlled school-based intervention study designed to reduce risk factors associated with overweight, decreases in sedentary behaviour among children were associated with decreases in BMI, controlling for natural growth (107). Similarly, in a treatment study for obese children, decreases in sedentary behaviour were associated with decreases in percent overweight and percent body fat (108). In most instances outlined above, relationships between sedentary behaviour and weight status were independent of SES. In addition, effects were often evident independent of levels of physical activity, suggesting that the influence of TV viewing on children’s weight status is not simply the result of the displacement of physical activity. Two studies among those identified failed to find an association between sedentary behaviour and weight status among children (71,109).
There are a number of reasons why TV viewing, and sedentary behaviour in general, are associated with increased risk of overweight among children. It has been shown that food advertisements during ‘child-viewing-hours’ comprise 63% of all advertisements and, of these advertisements, 60% are for sugar-coated breakfast cereals (110). TV viewing may therefore lead to requests by children for parents to purchase such foods and consequently influence children’s dietary patterns. In support of these ideas, research shows that weekly viewing hours correlate significantly and positively with (a) requests by children and purchases by parents of foods advertised on television (111) (b) children’s total caloric intake (111) and (c) children’s percent intake as fat (14). In addition, TV viewing of more than 1 hour per day has been associated with a high consumption of fast foods, sweets, chips, and pizza, and lower consumption of fruits and vegetables (112). Sedentary behaviour may also be linked to risk of overweight due to its effect on the displacement of physical activity. Time spent watching television is time that could have been spent involved in more energy demanding activities. Indeed research shows a negative relationship between TV viewing and physical activity among children and adolescents (77,83). However, as noted above, the relationship between TV viewing and weight status is independent of the displacement of physical activity, thus physical inactivity is only one of a number of routes by which sedentary behaviour influences children’s weight status.
Child characteristics
Rates of sedentary behaviour (specifically TV viewing) tend to be higher for girls than boys and increase for both girls and boys with increasing grade levels in school (82). It is unknown whether there are sex differences in the extent to which sedentary behaviour is associated with risk of overweight. It is possible that girls are affected to a greater extent than boys, as they are less likely to compensate for rates of sedentary behaviour with bouts of activity. In support of this possibility, Gortmaker and co-workers (113) in a school-based obesity prevention programme found that reductions in TV viewing were associated with a reduction in the incidence of obesity among girls but not boys, although boys also reported reduced levels of TV viewing. In addition, research has seldom assessed whether there are age differences in the effect of sedentary behaviour on risk of overweight. Due to decreases in rates of activity with increasing age, it is possible that older children are more affected by high rates of sedentary behaviour than younger children. Additional research is required to assess these possibilities.
Parenting styles and family characteristics
Parents are key sources of influence for children’s television practices and sedentary behaviour due to the ability they have to control and guide such practices. In comparison to research assessing the influence of parents on children’s dietary intake and physical activity, little research exists on the influence of parents on children’s sedentary behaviour. What research is available, however, suggests that parents shape children’s behaviour by their own TV viewing and sedentary practices (66) and by monitoring their children’s TV and video hours or failing to monitor such hours (114). It is unknown whether parenting styles relating to sedentary behaviour differ for children of different ages and for girls in comparison to boys. Finally, research has rarely considered the influence of peers and siblings on children’s sedentary behaviours.
Community, demographic and societal characteristics
Parenting styles related to children’s sedentary behaviour may be influenced by SES and ethnicity. Lower SES is associated with higher levels of sedentary behaviour among children (96). In addition, non-Hispanic black and Hispanic children report higher rates of sedentary behaviour than non-Hispanic white children (82,96). Higher rates of sedentary behaviour among low SES and ethnic minority groups may be due to lower parental monitoring of children’s TV viewing (114), a lack of knowledge of the benefits of exercise (99), the relatively inexpensive nature of television, videos, and computer games as a form of entertainment, and higher rates of crime in low SES and ethnic minority neighbourhoods. In neighbourhoods with high rates of crime, parents may view indoor activities as a proactive means of avoiding danger.
Summary and conclusions
The development of childhood overweight involves a complex set of factors from multiple contexts that interact with each other to place a child at risk of overweight. This system can be effectively conceptualized using Ecological Systems Theory, as illustrated in Fig. 1. Beginning at the level of the child, behavioural patterns such as a preference for fat, high percent fat intake, low levels of physical activity, and high levels of sedentary behaviour place a child at risk for the development of overweight. These factors are not considered risk or protective factors in isolation of each other, rather they work together to determine the risk of the development of overweight. For example, high fat intake may not necessarily be associated with higher weight status when it is compensated for with high levels of physical activity. Furthermore, child characteristics such as gender, age, and familial susceptibility to weight gain interact with each of these factors to determine the extent to which they act as risk or protective factors. For example, high energy or fat intake may differentially result in excessive weight gain depending upon a child’s susceptibility to weight gain and a child’s rate of growth and associated energy needs.
Research from fields that contribute to our understanding of energy balance and obesity highlights the importance of parents in shaping children’s dietary, activity, and sedentary behaviour patterns. Research shows that parents mould children’s behavioural patterns by their own behaviours (i.e. social modelling) and by parenting practices such as the types and quantities of foods parents present to children, their support of children’s extracurricular sporting activities, and their monitoring of children’s access to television, videos, and computer games. Parenting practices are also influenced by characteristics of the child, such as a child’s age, gender, and weight status; that is, parenting reflects bi–directional interactions between the parent and the child (115). This reveals that, although it is important to address parenting practices, we cannot assume that all children in the same family are exposed to the same environment. For example, we cannot assume that a brother and sister are exposed to the same child-feeding practices (or an overweight child and non-overweight child within the same family). Siblings experience both shared and non-shared environments. In addition to child characteristics such as age and gender, parenting practices relating to childhood overweight are influenced by the time parents have available for food preparation or to take their children to sporting events, parents’ nutritional knowledge and beliefs regarding healthful eating and activity patterns, and the availability of financial resources to enable healthful living.
This review provides important information for practitioners involved in the treatment of childhood overweight and the development of prevention and treatment programmes. As argued above, all risk factors for the development of childhood overweight have their initial beginnings in the family of origin. Therefore, an overweight child cannot be effectively treated in isolation of the family. Surprisingly few intervention programmes include multiple family members. Yet research shows that programmes that encourage weight loss among children and their parents have greater long-term success rates than programmes focusing solely on child weight reduction (116,117). In attempting to remedy the problem of childhood overweight, factors such as parents’ dietary and activity practices, parents’ child-feeding practices and nutritional knowledge, the extent to which parents encourage and enable their children to be active, parents’ TV viewing practices, and parents’ monitoring of their children’s TV viewing need to be taken into consideration. In addition, in order to effectively change parenting practices associated with increased risk of childhood overweight, factors that promote such practices must also be addressed (e.g. the time parents have available to prepare healthful meals and to create opportunities for the family to be physically active). Effective advice will include recommendations on how to work around constraints imposed on parents in order to promote a healthy lifestyle for all family members.
Finally, this review highlights the fact that research assessing predictors of childhood overweight has generally adopted approaches that do not reflect the contextual complexity and dynamic systems within which risk factors for childhood overweight emerge. That is, research in general has focused primarily on child and parent characteristics and has not considered the family system or the multileveled context in which child risk factors emerge. It is our contention that future research needs to adopt a broader contextual approach in developing and testing models of the development of childhood overweight. Specifically, in addition to child and parent characteristics, information on parenting practices, the school environment, and larger demographic factors influencing parenting practices needs to be obtained and assessed in a manner that reflects hypothesized processes leading to the development of overweight among children.
Acknowledgments
This research was supported by the National Institutes of Health grant #RO1 HD 32973.
The authors would like to thank Dr William Dietz for his valuable feedback on the initial version of this review.
References
- 1.Troiano RP, Flegal KM. Overweight children and adolescents: description, epidemiology, and demographics. Pediatrics. 1998;101:497–504. [PubMed] [Google Scholar]
- 2.Ogden CL, Troiano RP, Briefel RR, Kuczmarski RJ, Flegal KM, Johnson CL. Prevalence of overweight among preschool children in the United States. Pediatrics. 1997 April;99:E1. doi: 10.1542/peds.99.4.e1. [DOI] [PubMed] [Google Scholar]
- 3.Dietz WH. Health consequences of obesity in youth: childhood predictors of adult disease. Pediatrics. 1998;101:518–525. [PubMed] [Google Scholar]
- 4.Wallace WJ, Sheslow D, Hassink S. Obesity in children: A risk for depression. In: Williams CL, Kimm SYS, editors. Annals of the New York Academy of Science, 699: Prevention and treatment of childhood obesity. The New York Academy of Sciences; New York: 1993. pp. 301–302. [DOI] [PubMed] [Google Scholar]
- 5.Hill AJ, Draper E, Stack J. A weight on children’s minds: body shape dissatisfactions at 9-years old. Int J Obes. 1994;18:383–389. [PubMed] [Google Scholar]
- 6.Mendelson BK, White DR. Relation between body-esteem and self-esteem of obese and normal children. Percept Mot Skills. 1982;54:899–905. doi: 10.2466/pms.1982.54.3.899. [DOI] [PubMed] [Google Scholar]
- 7.Banis HT, Varni JW, Wallander JL, Korsch BM, Jay SM, Adler R, Garcia-Temple E, Negrete V. Psychological and social adjustment of obese children and their families. Child Care Health Dev. 1988;14:157–173. doi: 10.1111/j.1365-2214.1988.tb00572.x. [DOI] [PubMed] [Google Scholar]
- 8.Kimm SYS, Sweeney CG, Janosky JE, MacMillan JP. Self-concept measures and childhood obesity. A descriptive analysis. Dev Behav Pediatr. 1991;12:19–24. [PubMed] [Google Scholar]
- 9.Bronfenbrenner U. Ecology of the family as a context for human development: Research perspectives. Dev Psych. 1986;22:723–742. [Google Scholar]
- 10.Bronfenbrenner U, Morris PA. The ecology of human developmental processes. In: Damon W, Eisenberg N, editors. The handbook of child psychology. 3. John Wiley & Sons; New York: 1988. pp. 993–1027. [Google Scholar]
- 11.United Nations Children’s Fund. The State of the World’s Children. Oxford University Press; Oxford: 1998. [Google Scholar]
- 12.Bray GA, Popkin BM. Dietary fat does affect obesity. Am J Clin Nutr. 1998;68:1157–1173. doi: 10.1093/ajcn/68.6.1157. [DOI] [PubMed] [Google Scholar]
- 13.Stunkard AJ, Berkowitz RI, Stallings VA, Schoeller DA. Energy intake, not energy output, is a determinant of body size in infants. Am J Clin Nutr. 1999;69:524–530. doi: 10.1093/ajcn/69.3.524. [DOI] [PubMed] [Google Scholar]
- 14.Zive MM, Frank-Spopher GC, Sallis JF, McKenzie TL, Elder JP, Berry CC, Broyles SL, Nader PR. Determinants of dietary intake in a sample of white and Mexican-American children. J Am Diet Assoc. 1998;98:1282–1289. doi: 10.1016/S0002-8223(98)00288-0. [DOI] [PubMed] [Google Scholar]
- 15.Waxman M, Stunkard AJ. Caloric intake and expenditure of obese boys. J Pediatr. 1980;96:187–119. doi: 10.1016/s0022-3476(80)80800-6. [DOI] [PubMed] [Google Scholar]
- 16.Robertson SM, Cullen KW, Baranowski J, Baranowski T, Shaohua H, de Moor C. Factors related to adiposity among children aged 3–7 years. J Am Diet Assoc. 1999;99:938–943. doi: 10.1016/S0002-8223(99)00224-2. [DOI] [PubMed] [Google Scholar]
- 17.Berkey CS, Rockett HR, Field AE, Gillman MW, Frazier AL, Camargo CA, Colditz GA. Activity, dietary intake, and weight changes in a longitudinal study of preadolescent and adolescent boys and girls. Pediatrics. 2000;105:e56. doi: 10.1542/peds.105.4.e56. [DOI] [PubMed] [Google Scholar]
- 18.Guillaume M, Lapidus L, Lambert A. Obesity and nutrition in children. The Belgium Luxemburg Child Study IV. Eur J Clin Nutr. 1998;52:323–328. doi: 10.1038/sj.ejcn.1600532. [DOI] [PubMed] [Google Scholar]
- 19.Maffeis C, Talamini G, Tat L. Influence of diet, physical activity and parents’ obesity on children’s adiposity: a four year longitudinal study. Int J Obes. 1998;22:758–764. doi: 10.1038/sj.ijo.0800655. [DOI] [PubMed] [Google Scholar]
- 20.Rolland-Cachera MF, Deheeger M, Akrout M, Bellisle F. Influence of macronutrients on adiposity development: a follow up study of nutrition and growth from 10 months to 8 years of age. Int J Obes. 1995;19:573–578. [PubMed] [Google Scholar]
- 21.Gazzaniga JM, Burns TL. Relationship between diet composition and body fatness, with adjustment for resting energy expenditure and physical activity, in preschool children. Am J Clin Nutr. 1993;58:21–28. doi: 10.1093/ajcn/58.1.21. [DOI] [PubMed] [Google Scholar]
- 22.Tucker LA, Seljaas GT, Hager RL. Body fat percentage of children varies according to their diet composition. J Am Diet Assoc. 1997;97:981–986. doi: 10.1016/S0002-8223(97)00237-X. [DOI] [PubMed] [Google Scholar]
- 23.Nguyen VT, Larson DE, Johnson RK, Goran MI. Fat intake and adiposity in children of lean and obese parents. Am J Clin Nutr. 1996;63:507–513. doi: 10.1093/ajcn/63.4.507. [DOI] [PubMed] [Google Scholar]
- 24.Obarzanek E, Schreiber GB, Crawford PB, Goldman SR, Barrier PM, Frederick MM, Lakatos E. Energy intake and physical activity in relation to indexes of body fat: the National Heart, Lung and Blood Institute Growth and Health Study. Am J Clin Nutr. 1994;60:15–22. doi: 10.1093/ajcn/60.1.15. [DOI] [PubMed] [Google Scholar]
- 25.Klesges RC, Klesges LM, Eck LH, Shelton ML. A longitudinal analysis of accelerated weight gain in preschool children. Pediatrics. 1995;95:126–130. [PubMed] [Google Scholar]
- 26.Fisher JO, Birch LL. 3- to 5-year-old children’s fat preferences and fat consumption are related to parental adiposity. J Am Diet Assoc. 1995;95:759–764. doi: 10.1016/S0002-8223(95)00212-X. [DOI] [PubMed] [Google Scholar]
- 27.Ricketts CD. Fat preferences, dietary fat intake and body composition in children. Eur J Clin Nutr. 1997;51:778–781. doi: 10.1038/sj.ejcn.1600487. [DOI] [PubMed] [Google Scholar]
- 28.Resnicow K, Davis-Hearn M, Smith M, Baranowski T, Lin LS, Baronowski J, Doyle C, Wang DT. Social-cognitive predictors of fruit and vegetable intake in children. Health Psychol. 1997;16:272–276. doi: 10.1037//0278-6133.16.3.272. [DOI] [PubMed] [Google Scholar]
- 29.Goran MI. Measurement issues related to studies of childhood obesity: Assessment of body composition, body fat distribution, physical activity, and food intake. Pediatrics. 1998;101:505–518. [PubMed] [Google Scholar]
- 30.Bouchard C, Tremblay A, Després JP, Nadeau A, Lupien PJ, Thériault G, Dussault J, Moorjani S, Pinault S, Fournier G. The response to long term overfeeding in identical twins. N Engl J Med. 1990;322:1477–1482. doi: 10.1056/NEJM199005243222101. [DOI] [PubMed] [Google Scholar]
- 31.Heitmann BL, Lissner L, Sörenson TIA, Bengtsson C. Dietary fat intake and weight gain in women genetically predisposed for obesity. Am J Clin Nutr. 1995;61:1213–1217. doi: 10.1093/ajcn/61.6.1213. [DOI] [PubMed] [Google Scholar]
- 32.Pérusse L, Bouchard C. Role of genetic factors in childhood obesity and in susceptibility to dietary variations. Ann Med. 1999;31:19–25. doi: 10.1080/07853890.1999.11904395. [DOI] [PubMed] [Google Scholar]
- 33.Pérusse L, Tremblay A, Leblanc C, Cloninger CR, Reich T, Rice J, Bouchard C. Familial resemblance in energy intake: Contribution of genetic and environmental factors. Am J Clin Nutr. 1988;47:629–635. doi: 10.1093/ajcn/47.4.629. [DOI] [PubMed] [Google Scholar]
- 34.Laskarzewski P, Morrison JA, Khoury P, Kelly K, Glatfelter L, Larsen R, Glueck CJ. Parent-child nutrient intake relationships in school children ages 6–19: The Princeton School District Study. Am J Clin Nutr. 1980;33:2350–2355. doi: 10.1093/ajcn/33.11.2350. [DOI] [PubMed] [Google Scholar]
- 35.Patterson TL, Rupp JW, Sallis JF, Atkins CJ, Nader PR. Aggregation of dietary calories, fats, and sodium in Mexican-American and Anglo Families. Am J Prev Med. 1988;4:75–82. [PubMed] [Google Scholar]
- 36.Vauthier J, Lluch A, Lecomte E, Artur Y, Herberth B. Family resemblance in energy and macronutrient intakes. The Stanislas Family Study. Int J Epidemiol. 1996;25:1030–1037. doi: 10.1093/ije/25.5.1030. [DOI] [PubMed] [Google Scholar]
- 37.Oliveria SA, Ellison RC, Moore LL, Gillman MW, Garrahie EJ, Singer MR. Parent-child relationships in nutrient intake: The Framingham children’s study. Am J Clin Nutr. 1992;56:593–598. doi: 10.1093/ajcn/56.3.593. [DOI] [PubMed] [Google Scholar]
- 38.Borah-Giddens J, Falciglia GA. A meta-analysis of the relationship in food preferences between parents and children. J Nutr Educ. 1993;25:102–107. [Google Scholar]
- 39.Gibson EL, Wardle J, Watts CJ. Fruit and vegetable consumption, nutritional knowledge and beliefs in mothers and children. Appetite. 1998;31:205–228. doi: 10.1006/appe.1998.0180. [DOI] [PubMed] [Google Scholar]
- 40.Contento IR, Basch C, Shea S, Gutin B, Zybert P, Michela JL, Ripps J. Relationship of mothers’ food choice criteria to food intake of preschool children: Identification of family subgroups. Health Educ Q. 1993;20:243–259. doi: 10.1177/109019819302000215. [DOI] [PubMed] [Google Scholar]
- 41.Rolls BJ, Engell D, Birch LL. Serving portion size influences 5-year-old but not 3-year old children’s food intake. J Am Diet Assoc. 2000;100:232–23. doi: 10.1016/S0002-8223(00)00070-5. [DOI] [PubMed] [Google Scholar]
- 42.Birch LL, Marlin DW. I don’t like it; I never tried it: Effects of exposure on two–year–old children’s food preferences. Appetite. 1982;3:353–360. doi: 10.1016/s0195-6663(82)80053-6. [DOI] [PubMed] [Google Scholar]
- 43.Hearn MD, Baranowski T, Baranowski J, Doyle C, Smith M, Lin L, Resnicow K. Environmental influences on dietary behavior among children: Availability and accessibility of fruits and vegetables enable consumption. J Health Educ. 1998;29:26–32. [Google Scholar]
- 44.Fisher JO, Mitchell DC, Smiciklas–Wright H, Birch LL. Maternal milk consumption predicts the tradeoff between milk and soft drinks in young girls’ diets. J Nut. 2001;131:246–250. doi: 10.1093/jn/131.2.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fisher JO, Mitchell DC, Smicklas–Wright H, Birch L. Parental influence in young girls fruit and vegetable micronutrient and fat intakes. Journal of the American Dietetic Association. doi: 10.1016/s0002-8223(02)90017-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Birch LL. Obesity and eating disorders: a developmental perspective. Bull Psychonomic Soc. 1991;29:265–272. [Google Scholar]
- 47.Fisher JO, Birch LL. Restricting access to foods and children’s eating. Appetite. 1999a;32:405–419. doi: 10.1006/appe.1999.0231. [DOI] [PubMed] [Google Scholar]
- 48.Koivisto U, Fellenius J, Sjödén P. Relations between parental mealtime practices and children’s food intake. Appetite. 1994;22:245–257. doi: 10.1006/appe.1994.1023. [DOI] [PubMed] [Google Scholar]
- 49.Klesges RC, Malott JM, Boschee PF, Weber JM. The effects of parental influences on children’s food intake, physical activity, and relative weight. Int J Eat Disord. 1986;5:335–346. [Google Scholar]
- 50.Fisher JO, Birch LL. Restricting access to a palatable food affects children’s behavioral response, food selection, and intake. Am J Clin Nutr. 1999b;69:1264–1272. doi: 10.1093/ajcn/69.6.1264. [DOI] [PubMed] [Google Scholar]
- 51.Birch LL, Zimmerman S, Hind H. The influence of social–affective context on preschool children’s food preferences. Child Dev. 1980;51:856–861. [Google Scholar]
- 52.Sherman JB, Alexander MA, Clark L, Dean A, Welter L. Instruments measuring maternal factors in obese preschool children. West J Nurs Res. 1992;14:555–575. doi: 10.1177/019394599201400502. [DOI] [PubMed] [Google Scholar]
- 53.Costanzo PR, Woody EZ. Domain–specific parenting styles and their impact on the child’s development of particular deviance: the example of obesity proneness. J Soc Clin Psychol. 1985;1:425–445. [Google Scholar]
- 54.Birch LL. Effects of peer models’ food choices and eating behaviors on preschoolers’ food preferences. Child Dev. 1980;51:489–496. [Google Scholar]
- 55.Hill JO, Peters JC. Environmental contributions to the obesity epidemic. Science. 1998;280:1371–1374. doi: 10.1126/science.280.5368.1371. [DOI] [PubMed] [Google Scholar]
- 56.Popkin BM, Doak CM. The obesity epidemic is a worldwide phenomenon. Nutr Rev. 1998;56:106–114. doi: 10.1111/j.1753-4887.1998.tb01722.x. [DOI] [PubMed] [Google Scholar]
- 57.McCrory MA, Fuss PJ, Hays NP, Vinken AG, Greenberg AS, Roberts SB. Overeating in America: Association between restaurant food consumption and body fatness in healthy adult men and women ages 19–80. Obes Res. 1999;7:564–571. doi: 10.1002/j.1550-8528.1999.tb00715.x. [DOI] [PubMed] [Google Scholar]
- 58.Cheadle A, Psaty BM, Curry S, Wagner E, Diehr P, Koepsell T, Kristal A. Community–level comparisons between the grocery store environment and individual dietary practices. Prev Med. 1991;20:250–261. doi: 10.1016/0091-7435(91)90024-x. [DOI] [PubMed] [Google Scholar]
- 59.Johnson RK, Guthrie H, Smiciklas–Wright H, Wang MQ. Characterizing nutrient intakes of children by sociodemographic characteristics. Public Health Rep. 1994;109:414–420. [PMC free article] [PubMed] [Google Scholar]
- 60.Wolfe W, Campbell CC. Food pattern, diet quality, and related characteristics of schoolchildren in New York State. J Am Diet Assoc. 1993;93:1280–1284. doi: 10.1016/0002-8223(93)91955-p. [DOI] [PubMed] [Google Scholar]
- 61.Allan JD, Mayo K, Mitchel Y. Body size values of White and Black women. Res Nurs Health. 1993;16:323–33. doi: 10.1002/nur.4770160503. [DOI] [PubMed] [Google Scholar]
- 62.Powell AD, Kahn AS. Racial differences in women’s desires to be thin. Int J Eating Disor. 1995;17:191–195. doi: 10.1002/1098-108x(199503)17:2<191::aid-eat2260170213>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 63.Rucker CE, Cash TF. Body images, body–size perceptions, and eating behaviors among African–American and White college students. Int J Eating Disor. 1992;12:291–299. [Google Scholar]
- 64.Kramer MS, Barr RG, Leduc DG, Boisjoly C, Pless B. Maternal psychological determinants of infant obesity. J Chronic Dis. 1983;36:329–335. doi: 10.1016/0021-9681(83)90118-2. [DOI] [PubMed] [Google Scholar]
- 65.Young–Hyman D, Herman LJ, Scott DL, Schlundt DG. Care giver perception of children’s obesity–related health risk: a study of African–American families. Obes Res. 2000;8:241–248. doi: 10.1038/oby.2000.28. [DOI] [PubMed] [Google Scholar]
- 66.Baughcum AE, Burlow KA, Deeks CM, Powers SW, Whitaker RC. Maternal feeding practices and childhood obesity: a focus group study of low–income mothers. Arch Pediatr Adol Med. 1998;152:1010–1014. doi: 10.1001/archpedi.152.10.1010. [DOI] [PubMed] [Google Scholar]
- 67.Luepker RV, Perry CL, McKinlay SM, Nader PR, Parcel GS, Stone EJ, Webber LS, Elder JP, Feldman HA, Johnson CC, Kelder SH, Wu M. Outcomes of a field trial to improve children’s dietary patterns and physical activity. The Child and Adolescent Trial for Cardiovascular Health (CATCH) J Am Med Assoc. 1996;275:768–776. doi: 10.1001/jama.1996.03530340032026. [DOI] [PubMed] [Google Scholar]
- 68.Wolf AM, Gortmaker SL, Cheung L, Gray HM, Herzog DB, Colditz GA. Activity, inactivity, and obesity: Racial, ethnic, and age differences among schoolgirls. Am J Public Health. 1993;83:1625–1627. doi: 10.2105/ajph.83.11.1625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sunnegardh J, Bratteby LE, Hagman U, Samuelson G, Sjolin S. Physical activity in relation to energy intake and body fat in 8–and 13–year–old children in Sweden. Acta Paediatr Scand. 1986;75:955–963. doi: 10.1111/j.1651-2227.1986.tb10323.x. [DOI] [PubMed] [Google Scholar]
- 70.Goran MI, Hunter G, Nagy TR, Johnson R. Physical activity related energy expenditure and fat mass in young children. Int J Obes Relat Metabol Disor. 1997;21:171–178. doi: 10.1038/sj.ijo.0800383. [DOI] [PubMed] [Google Scholar]
- 71.Fogelholm M, Nuutinen O, Pasanen M, Myöhänen E, Säätelä T. Parent–child relationship of physical activity patterns and obesity. Int J Obes. 1999;23:1262–1268. doi: 10.1038/sj.ijo.0801061. [DOI] [PubMed] [Google Scholar]
- 72.Hernández B, Gortmaker SL, Colditz GA, Peterson KE, Laird NM, Parra–Cabrera S. Association of obesity with physical activity, television programs and other forms of video viewing among children in Mexico City. Int J Obes. 1999;23:845–854. doi: 10.1038/sj.ijo.0800962. [DOI] [PubMed] [Google Scholar]
- 73.Hanley AJ, Harris SB, Gittelsohn J, Wolever TM, Saksvig B, Zinman B. Overweight among children and adolescents in a Native Canadian community: prevalence and associated factors. Am J Clin Nutr. 2000;71:693–700. doi: 10.1093/ajcn/71.3.693. [DOI] [PubMed] [Google Scholar]
- 74.Epstein LH, Wing RR, Koeske R, Valoski A. A comparison of lifestyle exercise, aerobic exercise, and calisthenics on weight loss in obese children. Behav Therap. 1985;16:345–356. [Google Scholar]
- 75.Gutin B, Owens S, Okuyama T, Riggs S, Ferguson M, Litaker M. Effect of physical training and its cessation on percent body fat and bone density of children with obesity. Obes Res. 1999;7:208–214. doi: 10.1002/j.1550-8528.1999.tb00703.x. [DOI] [PubMed] [Google Scholar]
- 76.Treuth MS, Figueroa–Colon R, Hunter GR, Weinsier RL, Butte NF, Goran MI. Energy expenditure and physical fitness in overweight vs. non–overweight pre–pubertal girls. Int J Obes. 1998;22:440–447. doi: 10.1038/sj.ijo.0800605. [DOI] [PubMed] [Google Scholar]
- 77.Sallis JF, Prochaska JJ, Taylor WC. A review of correlates of physical activity of children and adolescents. Med Sci Sports Exerc. 2000;32:963–975. doi: 10.1097/00005768-200005000-00014. [DOI] [PubMed] [Google Scholar]
- 78.Sallis JF, Saelens BE. Assessment of physical activity by self-report: Status, limitations and future directions. Res Q Exerc Sport. 2000;71:1–14. doi: 10.1080/02701367.2000.11082780. [DOI] [PubMed] [Google Scholar]
- 79.Antshel KM, Andermann EM. Social influences on sports participation during adolescence. J Res Dev Educ. 2000;33:85–94. [Google Scholar]
- 80.Lindquist CH, Reynolds KD, Goran MI. Sociocultural determinants of physical activity among children. Prev Med. 1999;29:305–312. doi: 10.1006/pmed.1999.0546. [DOI] [PubMed] [Google Scholar]
- 81.Goran MI, Gower BA, Nagy TR, Johnson RK. Developmental changes in energy expenditure and physical activity in children: Evidence for a decline in physical activity in girls before puberty. Pediatrics. 1998;101:887–891. doi: 10.1542/peds.101.5.887. [DOI] [PubMed] [Google Scholar]
- 82.Myers L, Strikmiller PK, Webber LS, Berenson GS. Physical and sedentary activity in school children grades 5–8: The Bogalusa Heart Study. Med Sci Sports Exerc. 1996;28:852–859. doi: 10.1097/00005768-199607000-00012. [DOI] [PubMed] [Google Scholar]
- 83.Vilhjalmsson R, Thorlindsson T. Factors related to physical activity: a study of adolescents. Soc Sci Med. 1998;47:665–675. doi: 10.1016/s0277-9536(98)00143-9. [DOI] [PubMed] [Google Scholar]
- 84.Gregson JF, Colley A. Concomitants of sport participation in male and female adolescents. Int J Sport Psychol. 1986;17:10–22. [Google Scholar]
- 85.Anderssen N, Wold B. Parental and peer influences on leisure-time physical activity in young adolescents. Res Q Exerc Sport. 1992;63:341–348. doi: 10.1080/02701367.1992.10608754. [DOI] [PubMed] [Google Scholar]
- 86.Sallis JF, Patterson TL, McKenzie TL, Nader PR. Family variables and physical activity in preschool children. J Dev Behav Pediatr. 1988;2:57–61. [PubMed] [Google Scholar]
- 87.Gottlieb NH, Chen M. Sociocultural correlates of childhood sporting activities: Their implications for heart health. Soc Sci Med. 1985;21:533–539. doi: 10.1016/0277-9536(85)90037-1. [DOI] [PubMed] [Google Scholar]
- 88.Wold B, Anderssen N. Health promotion aspects of family and peer influences on sport participation. Int J Sport Psychol. 1992;23:343–359. [Google Scholar]
- 89.Freedson PS, Evenson S. Familial aggregation in physical activity. Res Q Exerc Sport. 1991;62:384–389. doi: 10.1080/02701367.1991.10607538. [DOI] [PubMed] [Google Scholar]
- 90.Moore LL, Lombardi DA, White MJ, Campbell JL, Oliveria SA, Ellison RC. Influences of parents’ physical activity levels on activity levels of young children. J Pediatr. 1991;118:215–219. doi: 10.1016/s0022-3476(05)80485-8. [DOI] [PubMed] [Google Scholar]
- 91.Davison KK, Birch LL. Child and parent characteristics as predictors of girls’ change in Body Mass Index. doi: 10.1038/sj.ijo.0801835. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Dishman RK, Sallis JF, Orenstein DR. The determinants of physical activity and exercise. Public Health Rep. 1985;100:158–171. [PMC free article] [PubMed] [Google Scholar]
- 93.Sallis JF, Alcaraz JE, McKenzie TL, Hovell MF. Predictors of change in children’s physical activity over 20 months: Variations by gender and level of adiposity. Am J Prev Med. 1999;16:222–229. doi: 10.1016/s0749-3797(98)00154-8. [DOI] [PubMed] [Google Scholar]
- 94.Klesges RC, Eck LH, Hanson CL, Haddock CK, Klesges LM. Effects of obesity, social interactions, and physical environment on physical activity in preschoolers. Health Psychol. 1990;9:435–449. doi: 10.1037//0278-6133.9.4.435. [DOI] [PubMed] [Google Scholar]
- 95.Savin-Williams RC, Berndt TJ. Friendship and peer relations. In: Feldman SS, Elliot GR, editors. At the Threshold: the Developing Adolescent. Harvard University Press; Massachusetts: 1990. pp. 277–307. [Google Scholar]
- 96.Gordon-Larsen P, McMurray RG, Popkin BM. Determinants of adolescent physical activity and inactivity patterns. Pediatrics. 2000;105:E83. doi: 10.1542/peds.105.6.e83. [DOI] [PubMed] [Google Scholar]
- 97.McKenzie TL, Sallis JF, Nader PR, Broyles SL, Nelson JA. Anglo- and Mexican-American preschoolers at home and at recess: Activity patterns and environmental influences. J Dev Behav Pediatr. 1992;13:173–180. [PubMed] [Google Scholar]
- 98.Harris MB, Koehler KM. Eating and exercise behaviors and attitudes of Southwestern Anglos and Hispanics. Psychol Health. 1992;7:165–174. [Google Scholar]
- 99.Tuinstra J, Groothoff JW, Van Den Heuvel WJA, Post D. Socioeconomic differences in health risk behavior in adolescence: do they exist? Soc Sci Med. 1998;47:67–74. doi: 10.1016/s0277-9536(98)00034-3. [DOI] [PubMed] [Google Scholar]
- 100.Sobal J, Stunkard AJ. Socioeconomic status and obesity: a review of the literature. Psychol Bull. 1989;105:260–275. doi: 10.1037/0033-2909.105.2.260. [DOI] [PubMed] [Google Scholar]
- 101.Centers for Disease Control. Youth Behavior Risk Surveillance – United States. Morbidity and Mortality Weekly Report. 1998;47:SS-03. [PubMed] [Google Scholar]
- 102.Sallis JF, McKenzie TL, Alcaraz JE, Kolody B, Hovell MF, Nader PR . Project SPARKS. Effects of physical education on adiposity in children. In: Williams CL, Kimm SYS, editors. Annals of the New York Academy of Science, 699 Prevention and Treatment of Childhood Obesity. The New York Academy of Sciences; New York: 1993. pp. 127–136. [DOI] [PubMed] [Google Scholar]
- 103.Huston AC, Donnerstein E, Fairchild H, Feshbach N, Katz P, Murray J, Rubinstein E, Wilcox B, Zuckerman D. Big World, Small Screen: the Role of Television in American Society. University of Nebraska Press; Lincoln: 1992. [Google Scholar]
- 104.Dietz WH, Gortmaker SL. Do we fatten our children at the television set? Obesity and television viewing in children and adolescents. Pediatrics. 1985;75:807–812. [PubMed] [Google Scholar]
- 105.McMurray RG, Harrell JS, Deng S, Bradley CB, Cox LM, Bangiwala SI. The influence of physical activity, socioeconomic status, and ethnicity on the weight status of adolescents. Obes Res. 2000;8:130–139. doi: 10.1038/oby.2000.14. [DOI] [PubMed] [Google Scholar]
- 106.Andersen RE, Crespo CJ, Bartlett SJ, Cheskin LJ, Pratt M. Relationship of physical activity and television watching with body weight and level of fatness among children: Results from the third national health and nutrition examination survey. J Am Med Assoc. 1998;279:938–942. doi: 10.1001/jama.279.12.938. [DOI] [PubMed] [Google Scholar]
- 107.Robinson TN. Reducing children’s television to prevent obesity: a randomized controlled trial. J Am Med Assoc. 1999;282:1561–1567. doi: 10.1001/jama.282.16.1561. [DOI] [PubMed] [Google Scholar]
- 108.Epstein LH, Paluch RA, Gordy CC, Dorn J. Decreasing sedentary behaviors in treating pediatric obesity. Arch Pediatr Adol Med. 2000;154:220–226. doi: 10.1001/archpedi.154.3.220. [DOI] [PubMed] [Google Scholar]
- 109.Robinson TN, Hammer LD, Killen JD, Kraemer HC, Wilson DM, Hayward C, Taylor CB. Does television viewing increase obesity and reduce physical activity? Cross-sectional and longitudinal analyses among adolescent girls. Pediatrics. 1993;91:273–280. [PubMed] [Google Scholar]
- 110.Lewis MK, Hill AJ. Food advertising on British children’s television: a content analysis and experimental study with nine-year-olds. Int J Obes. 1998;22:206–214. doi: 10.1038/sj.ijo.0800568. [DOI] [PubMed] [Google Scholar]
- 111.Taras HL, Sallis JF, Patterson TL, Nader PR, Nelson JA. Television’s influence on children’s diet and physical activity. J Dev Behav Pediatr. 1989;10:176–180. [PubMed] [Google Scholar]
- 112.Muller MJ, Koertringer I, Mast M, Languix K, Frunch A. Physical Activity and Diet in 5–7 Years Old Children. Public Health Nutr. 1999;2:443–444. doi: 10.1017/s1368980099000609. [DOI] [PubMed] [Google Scholar]
- 113.Gortmaker SL, Peterson K, Wiecha J, Sobol AM, Dixit S, Fox MK, Laird N. Reducing obesity via a school-based interdisciplinary intervention among youth. Arch Pediatr Adol Med. 1999;153:409–418. doi: 10.1001/archpedi.153.4.409. [DOI] [PubMed] [Google Scholar]
- 114.Valerio M, Amodio P, Dal Zio M, Vianello A, Zacchello GP. The use of television in 2- to 8-year old children and the attitude of parents about such use. Arch Pediatr Adol Med. 1997;151:22–26. doi: 10.1001/archpedi.1997.02170380026004. [DOI] [PubMed] [Google Scholar]
- 115.Magnusson DH, Håkan S. Person–context interaction theories. In: Damon W, Eisenberg N, editors. The Handbook of Child Psychology. 3. John Wiley & Sons; New York: 1998. pp. 685–740. [Google Scholar]
- 116.Brownell KD, Kelman JH, Stunkard AJ. Treatment of obese children with and without their mothers: changes in weight and blood pressure. Pediatrics. 1983;71:515–523. [PubMed] [Google Scholar]
- 117.Epstein LH, Valoski A, Wing R, McCurley J. Ten-year follow-up of behavioral, family-based treatment for obese children. J Am Med Assoc. 1990;264:2519–2523. [PubMed] [Google Scholar]