Abstract
A retrospective study was designed to evaluate the results of closed reduction and percutaneous pinning using threaded pins as a treatment option for fractures of the humeral head. Patients who suffered two- and three-part fractures of the proximal humerus treated by this method of fixation were included. Fifty patients (32 females and 18 males) with an average age of 50 years were clinically evaluated at an average of 2.5 years after this procedure (range 1–4 years). The Constant score was used to evaluate the clinical outcome. Preoperative and postoperative X-rays were also assessed. Out of 50 patients, 18 (36%) obtained excellent results, 17 (34%) good results, eight (16%) fair results and seven (14%) achieved only poor results. The average Constant score was 81 (range 60–100). Fractures confined to the surgical or anatomical neck generally did better than those associated with a greater tuberosity fragment (average score 86 versus 78). Patients who required shaft stabilisation and in addition to reduction and fixation of the greater tuberosity showed a lower average score (68). There were no cases of avascular necrosis, neurovascular complications or deep infections. A significant loss of fracture position due to failure of internal fixation occurred in seven cases, three of these patients underwent revision surgery. Closed reduction and percutaneous pinning offers a good fracture position and stability with minimal soft tissue damage. We recommend that displaced two- and three- part fractures of the humeral head should be treated in this manner. However these patients should be monitored closely for a period of four weeks, since secondary displacement and failure of fixation can occur in this period. Careful patient selection may minimise these complications.
Résumé
Etude retrospective de la réduction à foyer fermé et de la fixation percutanée avec des broches filetées des fractures à deux et trois fragments de l’extrémité supérieure de l’humérus. Method : 50 patients, d’âge moyen 50 ans, ont été évalués cliniquement à un délai moyen de 2,5 ans après l’opération.Le score de Constant ainsi que les radiographies pré et post opératoires ont été utilisés pour l’appréciation. ResultsSur 50 patients 18 obtenaient un excellent résultat, 17 un bon résultat, 8 un résultat moyen et 7 un mauvais résultat. Le score de Constant moyen était de 81 (de 60 à 100). Les fractures isolées du col anatomique ou chirurgical avaient un meilleure évolution que celles associées à une fracture de la grosse tubérosité ( score de 86 au lieu de 78).Les patients qui ont nécessité une réduction et une fixation de la grosse tubérosité en plus de la stabilisation diaphysaire avaient un score moyen plus bas (68). Il n’y avait pas de nécrose, d’infection profonde ni de trouble neurovasculaire. Une perte de réduction est survenu dans 7 cas avec nécessité de reprise chirurgicale 3 fois. Conclusions : la réduction fermée avec fixation par broches percutanées permet une bonne stabilisation de la fracture avec un minimum de dommages aux parties molles. Nous préconisons ce traitement pour les fractures à 2 et 3 fragments de la tête humérale en recommandant une surveillance étroite pendant les 4 premières semaines car le déplacement secondaire et l’échec de la fixation représente un écueil sérieux de la méthode.
Introduction
The incidence of fractures of the proximal humerus has increased significantly in the last decade. Hagino in 1995 reported an incidence of 17 and 45 cases per 100,000 general population for men and women respectively [1]. This type of fracture is especially frequent among the elderly [2].
Neer’s four-fragment classification is one of the accepted systems to describe these fractures [3]. Non-displaced or minimally displaced fractures can be treated conservatively with success [4]. On the other hand, unstable displaced two- and three-part fractures should be reduced and stabilised. Hemiarthroplasty is currently indicated in cases of four-part fractures in older patients, in head-splitting fractures or in severe articular surface damage caused by impaction or depression [5, 6].
Many methods of fixation for these fractures have been described in the literature, such as the use of plates, intramedullary nails [7], wiring [8] and external fixation. In the past few years the trend has changed from open reduction and massive internal fixation towards closed reduction and minimal fixation [9], which is a less invasive method associated with less damage to the soft tissue and a low rate of avascular necrosis of the humeral head.
The purpose of this study was to evaluate this mode of treatment.
Materials and methods
Over a period of four years 56 patients with displaced two- and three-part fractures according to Neer’s classification underwent closed reduction and percutaneous pinning. Fifty (32 females and 18 males) out of these 56 were available for evaluation both radiographically and clinically with an average follow-up of 2.5 years (range one to four years). Six patients were not included in the study since they were not available for evaluation. The average age of the patients was 50 years (range 21–78 years). Out of 50 fractures, 24 were two-part and 26 were three-part fractures. Out of the 24 two-part fractures, 22 involved the surgical neck and 2 the anatomical neck of the proximal humerus. Out of the 26 three-part fractures, 25 involved the surgical neck and one the anatomical neck, plus the greater tuberosity.
All patients were operated on within six days of the injury.
The operation was performed with the patient in a half-sitting position. Under general anesthesia closed manipulation under fluoroscopic control was performed to achieve good head–shaft contact and position. The image intensifier was located cranially with the C-arm at right angles to the axis of the head of the humerus. The pins were inserted directly beneath the insertion of the deltoid into the humerus towards the humeral head. Size 0.3 partially threaded K-wires were used for fixation. Three to five pins were inserted in each case, reaching the subchondral bone of the humeral head, until stable fixation was evident on fluoroscopic examination. After insertion the pins were cut and left under the skin to prevent pin-tract infection.
Post-operatively the shoulder was immobilized in a shoulder immobilizer for a period of six weeks. After which the pins were removed under local anesthesia and a gradual sequence of shoulder rehabilitation began. The patients were examined in the outpatient clinic three weeks, six weeks, three months, one year and two to four years after surgery. AP, axial-scapular and lateral-scapular X-rays were obtained at each visit to assess alignment, union and signs of avascular necrosis. We used the Constant score for clinical evaluation. The Constant score is a 100-point scoring system composed of the following parameters: pain (15 points), activities of daily living (20 points), range of motion (40 points) and power (25 points). The power of the shoulder was measured using the method described by Mosely, with scoring based on the number of pounds of pull the patient can resist in abduction, up to a maximum of 90 deg. Only active range of motion was considered, including forward, abduction, internal and external rotation. The range of motion was assessed and compared with that of the opposite shoulder.
Results
Eighteen patients (36%) had excellent results, 17 (34%) had good, eight (16%) had fair and seven (14%) had poor results. The average Constant score was 81 (range 60–100).
The average age of patients with two-part fractureswas 45 years, compared with 57 years for three- part fractures.
The two-part fractures had better results than the three-part fractures, with an average Constant score, adjusted for age and gender, of 86 (range 78–100) and 78 (range 48–100), respectively.
Thirteen of the 24 patients with two-part fracture had no pain at all, 19 no limitation of daily activities and 13 enjoyed some form of recreational sport. There was no significant limitation of abduction associated with the two-part fractures: 19 of the 24 patients had forward flexion and abduction greater than 150 deg. With regard to internal rotation, 16 could touch their shoulder blades with the back of their hand, three reached the T12 vertebra, and five could reach the lumbar spine only. Sixteen of 24 patients were very satisfied or satisfied with the outcome.
There was no medialisation of the shaft or significant angulations of the humeral head on X-ray in this group.
Patients with three-part fractures had an average Constant score, adjusted for age and gender, of 78 (range 48–100). Fifteen of the 26 patients had no pain at all, forward flexion and abduction greater than 150 deg, no limitation in daily activities and enjoyed some form of recreational sport. With regard to internal rotation, 14 patients could touch their shoulder blades with the back of their hand, six reached the T12 vertebra, five reached the lumbar spine and one patient reached only the sacro-iliac joint. Sixteen of the 26 patients were very satisfied or satisfied with the outcome.
In nine patients with three-part fractures, reduction and stabilisation of the greater tuberosity was needed in addition to pinning of the surgical neck because of superior migration of more than 5 mm: in three cases this was done by closed percutaneous screw fixation using 3.5 cannulated screws, and in six cases by open reduction and suturing the greater tuberosity with absorbable PDS sutures through a minimal trans-deltoid approach (Fig. 1).
Fig. 1.
A three-part fracture treated by closed reduction, percutaneous pinning and open reduction and PDS-suture fixation of the greater tuberosity
In three of the six patients with PDS sutures, cranial migration of the greater tuberosity of 5-mm or more was seen on follow-up X-ray, despite the fixation.
In 17 patients with three- part fractures the greater tuberosity was left untreated since the primary displacement was less than 5 mm. In six out of the 17 (35%), secondary cranial migration greater than 5 mm of the greater tuberosity was seen on follow-up X-ray.
The average Constant score of the patients with three- part fractures who underwent reduction and fixation of the greater tuberosity in addition to pinning was 68, compared with the average score of 78 for the whole group of three- part fractures.
In seven of 50 cases (14%) significant secondary displacement due to failure of fixation occurred. All these patients had three-part fractures. The average age of the seven patients was high (72 years in comparison with 57 years for the entire three-part fracture group). Three of them had secondary proximal migration of the greater tuberosity of 5 mm or more (sutured primarily with PDS as discussed above), and four of them had a significant loss of head–shaft alignment. Three of the four patients with loss of head–shaft alignment underwent revision surgery: closed pinning was repeated in two cases, and in one open reduction and fixation with pins was carried out. The two patients who underwent closed reduction and repinning had poor final outcome despite good X-ray alignment, and the patient who underwent open reduction and repinning eventually needed an hemiarthroplasty due to failure of the second procedure.
The fourth case of significant head–shaft displacement was allowed to heal in the displaced position (because of the patient’s general condition and low level of activity) and the final outcome was poor.
There was no case of non-union, avascular necrosis, deep infection or neurovascular injury. In five cases there was superficial wound infection at the site of pin insertion which resolved after pin removal.
Discussion
The incidence of fracture of the proximal humerus is increasing. Conservative treatment in a sling followed by functional rehabilitation under supervision yields satisfactory results in minimally displaced fractures. On the other hand, displaced two- and three-part fractures need to be reduced and stabilised [10]. Reduction and fixation is unsuitable for four-part fractures in elderly patients where the preferred treatment is hemiarthroplasty, which generally provides good pain relief [11].
Recent trends are away from open reduction and massive internal fixation towards closed reduction and percutaneous fixation as this method is less invasive and causes less soft tissue damage. Another complication associated with open reduction and massive fixation is the risk for avascular necrosis of the humeral head, which causes significant functional impairment. Percutaneous pinning seems to be a suitable alternative to other operative techniques such as intramedullary nailing or open/mini-open reduction and internal fixation using wires or plates [12, 13].
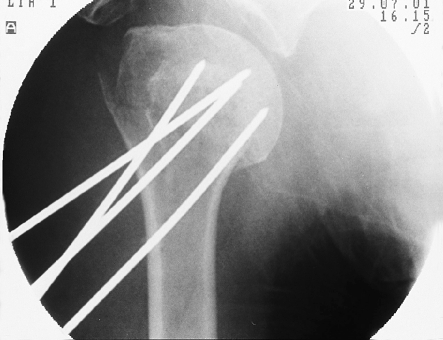
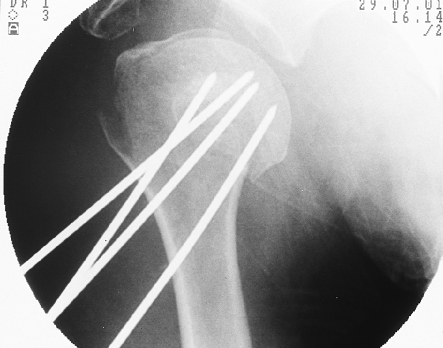
In most two-part surgical neck fractures, anatomical reduction and stable fixation can be achieved in a closed manner (Figs. 2 and 3).
Fig. 2.
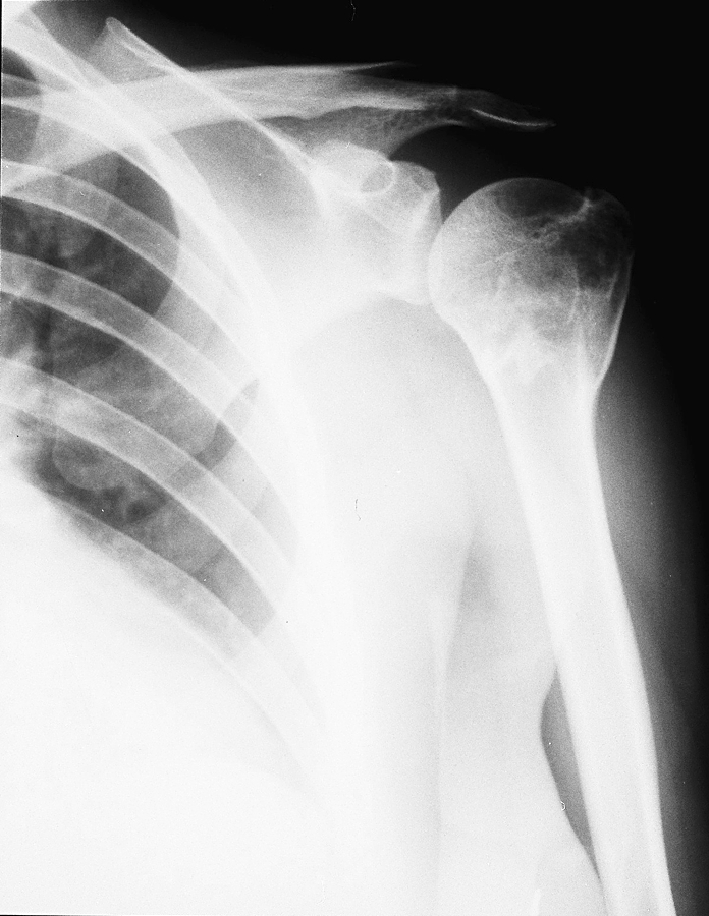
Two years after closed reduction and percutaneous pinning of a two-part fracture. Healing in an anatomical position
Fig. 3.
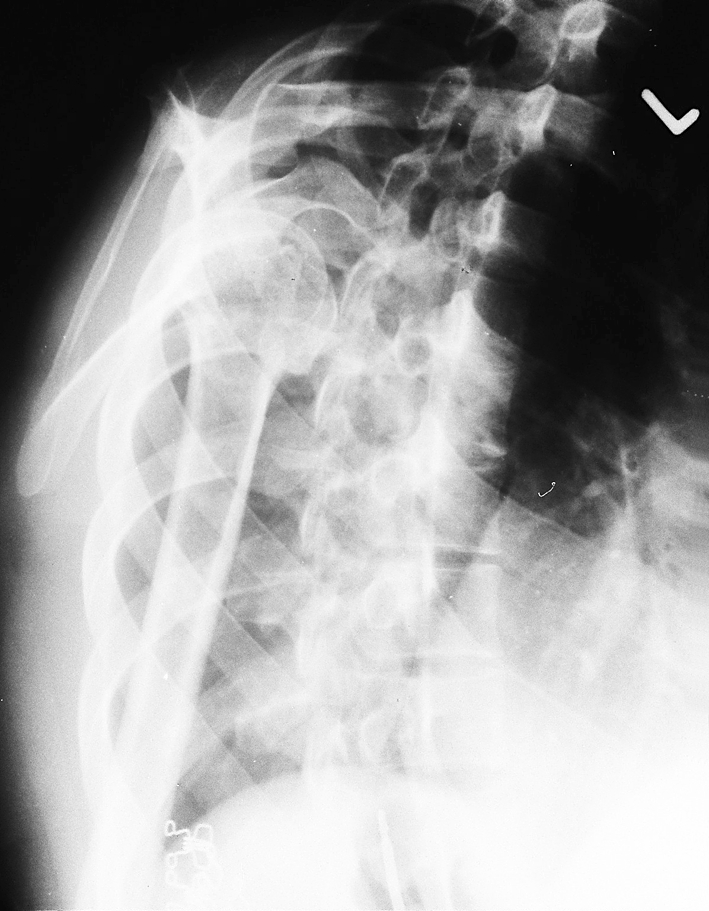
Two years after closed reduction and percutaneous pinning of a two-part fracture. Healing in an anatomical position
In our study no complications were associated with the treatment of these fractures, and the threaded pins provided satisfactory reduction of the shaft to the head without secondary loss of fixation.
When dealing with three-part fractures with an additional displacement of the greater tuberosity, reduction of the main fragments may also reduce the greater tuberosity to a nearly anatomical position. The question is whether additional stabilisation is needed. In our study, in six of 17 cases (35%) a secondary proximal migration of the unfixed greater tuberosity greater than 5 mm was observed. On the other hand, an anatomical reduction does not necessarily correlate with the functional outcome, and secondary migration of the unfixed fragment did not interfere significantly with the final outcome.
Significant primary displacement of the greater tuberosity should be corrected, otherwise it can cause limitation of motion and loss of rotator cuff strength. We reduced and held the greater tuberosity primarily in nine of 26 cases when the displacement was greater than 5 mm. Use of PDS sutures was associated with a 50% rate of secondary loss of reduction, so it seems that those sutures are not strong enough.
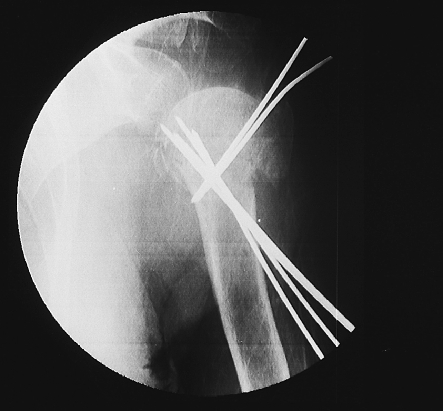
Our survey indicates that cases of displaced two- and three-part fracture could be treated by closed reduction and percutaneous pinning achieving good fracture positioning and adequate temporary stabilisation (Figs. 4, 5, 6). No major complications such as avascular necrosis, non-union, deep infection or neurovascular deficit were associated with this method of treatment.
Fig. 4.
A three-part fracture treated with closed reduction and percutaneous pinning, with a stable good position
Fig. 5.
A three-part fracture treated with closed reductionand percutaneous pinning, with a stable good position
Fig. 6.
A three-part fracture treated with closed reductionand percutaneous pinning, with a stable good position
The only major complication was significant secondary displacement due to failure of fixation in seven out of 50 cases (14%). All of these cases were three-part fractures. Out of the seven, four lost the head–shaft reduction and three lost the greater tuberosity reduction.
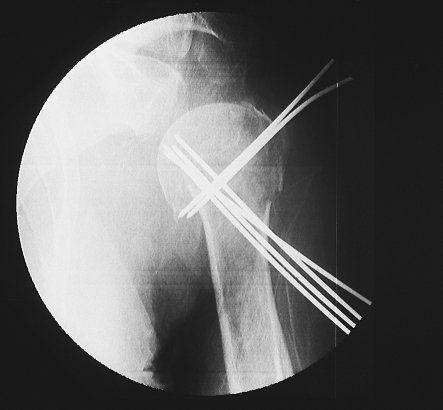
We believe that age and osteoporosis are the main reasons for the failure of the pins to hold the reduction. Other authors have described a combination of pins with other forms of internal fixation, such as screws, to overcome this problem [14]. Recently we have added two additional antegrade pins from the greater tuberosity into the medial cortex in order to improve stability (Figs. 7 and 8). These pins are left outside the skin, a fact that could increase the rate of infection.
Fig. 7.
A three-part fracture in an osteoporotic bone, treated with closed reduction and antegrade and retrograde pin fixation
Fig. 8.
A three-part fracture in an osteoporotic bone, treated with closed reduction and antegrade and retrograde pin fixation
Our findings are in line with previous studies advocating minimal pin fixation as a useful alternative for the treatment of Neer’s two- and three-part fractures of the proximal humerus.
References
- 1.Hagino H, Yamamoto K (1999) Changing incidence of hip distal radius and proximal humerus fractures in Tottori prefecture, Japan. Bone 24(3):265–270 [DOI] [PubMed]
- 2.Baron JA, Karagas M, Barett J, Kniffin W, Mlenka D, Mayor M, Keller RB (1996) Basic epidemiology of fractures of the upper and lower limb among Americans over 65 years of age. Epidemiology 7(6):612–618 [DOI] [PubMed]
- 3.Neer CS 2nd (1970) Displaced proximal humeral fractures. Classification and evaluation. J Bone Joint Surg Am 52:1077–1089 [PubMed]
- 4.Koval KJ, Gallagher MA (1997) Functional outcome after minimally displaced fractures of the proximal part of the humerus. J Bone Joint Surg Am 79(2):203–207 [DOI] [PubMed]
- 5.Wretenberg P, Ekelund A (1997) Acute hemiarthroplasty after proximal humerus fracture in old patients. A retrospective evaluation of 18 patients followed for 2–7 years. Acta Orthop Scand 68(2):121–123 [DOI] [PubMed]
- 6.Skutek M, Fremerey RW (1998) Level of physical activity in elderly patients after hemiarthroplasty for 3 and 4 parts fractures of the proximal humerus. Arch Orthop Trauma Surg 117(4–5):252–255 [DOI] [PubMed]
- 7.Wachtl SW, Marti CB, Hoogewoud HM, Jacob RP, Goutier E (2000) Treatment of proximal humerus fractures using multiple intramedullary flexible nails. Arch Orthop Trauma Surg 120(3):171–175 [DOI] [PubMed]
- 8.Bungaro P, Pascarella R, Rollo G, Di Ginnaro GL, Ercolani C (1998) Osteosynthesis with percutaneous wiring in fractures of the proximal humerus. Chir Organi Nov 83 (4):381–386 [PubMed]
- 9.Szyszkowitz R, Schippinger G (1999) Fracture of the proximal humerus. Unfallchirurg 102(6):422–428 [DOI] [PubMed]
- 10.Williams GR, Wong KL (2000) Two part and three part fractures: open reduction and internal fixation versus closed reduction and percutaneous pinning. Orthop Clin North Am 31(1):1–21 [DOI] [PubMed]
- 11.Naranja RJ, Iannoti JP (2000) Displaced 3 and 4 parts proximal humerus fractures: evaluation and management. J Am Acad Surg 8(6):373–382 [DOI] [PubMed]
- 12.Chen CY, Chao EK (1998) Closed management and percutaneous fixation of unstable proximal humerus fractures. J Trauma 45(6):1039–1045 [DOI] [PubMed]
- 13.Soete PJ, Clayson PE (1999) Transitory percutaneous pinning in fractures of the proximal humerus. J Shoulder Elbow Surg 8(6):569–573 [DOI] [PubMed]
- 14.Resch H (1997) Percutaneous fixation of three and four parts fractures of the proximal humerus. J Bone Joint Surg Br 79(2):295–300 [DOI] [PubMed]
- 15.Constant CR, Murley AH (1987) A clinical method of functional assessment of the shoulder. Clin Orthop 214:160–164 [PubMed]