Abstract
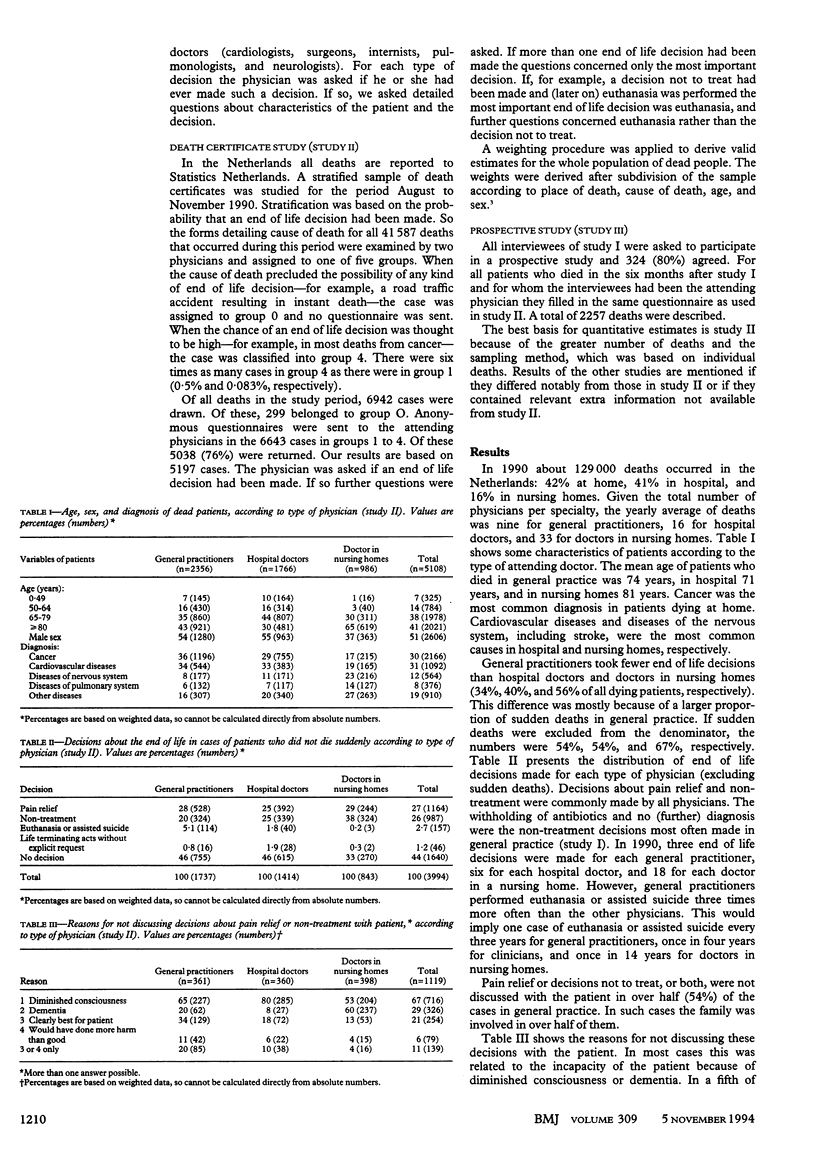
OBJECTIVE--To gain insight into decisions made in general practice about the end of life. DESIGN--Study I: interviews with 405 physicians. Study II: analysis of death certificates with data obtained on 5197 cases in which decisions about the end of life may have been made. Study III: prospective study with doctors from study I: questionnaires used to collect information about 2257 deaths. The information was representative for all deaths in the Netherlands. RESULTS--Over two fifths of all patients in the Netherlands die at home. General practitioners took fewer decisions about the end of life than hospital doctors and doctors in nursing homes (34%, 40%, and 56% of all dying patients, respectively). Specifically, decisions to withhold or withdraw treatment to prolong life were taken less often. Euthanasia or assisted suicide, however, was performed in 3.2% of all deaths in general practice compared with 1.4% in hospital practice. In over half of the cases concerning pain relief or non-treatment general practitioners did not discuss the decision with the patient, mostly because of incapacity of the patient, but in 20% of cases for "paternalistic" reasons. Older general practitioners discussed such decisions less often with their patients. Colleagues were consulted more often if the general practitioner worked in group practice. CONCLUSION--Differences in work situation between general practitioners and hospital doctors and differences between the group of general practitioners contribute to differences in the number and type of decisions about the end of life as well as in the decision making process.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Emanuel E. J., Emanuel L. L. Four models of the physician-patient relationship. JAMA. 1992 Apr 22;267(16):2221–2226. [PubMed] [Google Scholar]
- Hoffmaster C. B., Stewart M. A., Christie R. J. Ethical decision making by family doctors in Canada, Britain and the United States. Soc Sci Med. 1991;33(6):647–653. doi: 10.1016/0277-9536(91)90018-8. [DOI] [PubMed] [Google Scholar]
- Netherlands State Commission on Euthanasia Final report of the Netherlands State Commission on Euthanasia: an English summary. Bioethics. 1987 Apr;1(2):163–174. doi: 10.1111/j.1467-8519.1987.tb00025.x. [DOI] [PubMed] [Google Scholar]
- Orr R. D., Paris J. J., Siegler M. Caring for the terminally ill: resolving conflicting objectives between patient, physician, family, and institution. J Fam Pract. 1991 Nov;33(5):500–504. [PubMed] [Google Scholar]
- Pijnenborg L., van der Maas P. J., van Delden J. J., Looman C. W. Life-terminating acts without explicit request of patient. Lancet. 1993 May 8;341(8854):1196–1199. doi: 10.1016/0140-6736(93)91014-d. [DOI] [PubMed] [Google Scholar]
- Siegler M. The progression of medicine. From physician paternalism to patient autonomy to bureaucratic parsimony. Arch Intern Med. 1985 Apr;145(4):713–715. doi: 10.1001/archinte.145.4.713. [DOI] [PubMed] [Google Scholar]
- Van Der Maas P. J., Van Delden J. J., Pijnenborg L., Looman C. W. Euthanasia and other medical decisions concerning the end of life. Lancet. 1991 Sep 14;338(8768):669–674. doi: 10.1016/0140-6736(91)91241-l. [DOI] [PubMed] [Google Scholar]
- van der Wal G., Dillmann R. J. Euthanasia in The Netherlands. BMJ. 1994 May 21;308(6940):1346–1349. doi: 10.1136/bmj.308.6940.1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Wal G., van Eijk J. T., Leenen H. J., Spreeuwenberg C. Euthanasia and assisted suicide. I. How often is it practised by family doctors in The Netherlands? Fam Pract. 1992 Jun;9(2):130–134. doi: 10.1093/fampra/9.2.130. [DOI] [PubMed] [Google Scholar]


