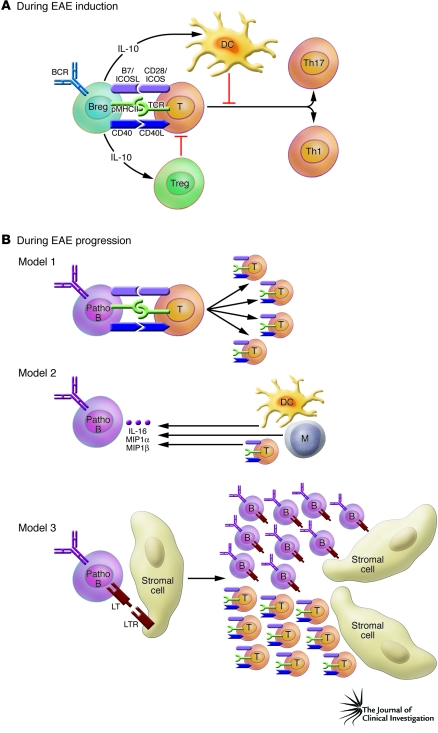
Figure 1. Potential mechanisms of pro- and antiinflammatory effects of B cells.
(A) In this issue of the JCI, Matsushita et al. (7) show the importance of the antiinflammatory role of CD1dhiCD5+ regulatory B cells during EAE initiation. In the initiation phase of EAE, antigen-specific CD1dhiCD5+ B cells (Breg) produce IL-10, which limits DC function and/or augments Treg function. Consequently, these DCs and Tregs could inhibit the differentiation of Th17 and Th1 T cells. (B) During the progression phase of EAE, three potential models for the mechanism of action of B cells can be envisaged. In the first model, pathogenic B cells (Patho B) can function as antigen-presenting cells and enhance the proliferation of pathogenic T cells and their differentiation. In the second model, antigen-activated pathogenic B cells produce IL-16, macrophage inflammatory protein 1α (MIP1α), and MIP1β, which can modulate the migration and function of DCs, monocytes (M), and pathogenic T cells. In the third model, interactions between B cells and stromal cells via TNF/TNF receptor family networks (such as interaction of lymphotoxin [LT] with the LT receptor [LTR]) induce lymphoid-like follicle formation in the CNS, which might provide the optimal site for expansion of pathogenic T cells. B, B cell; BCR, B cell receptor; CD40L, CD40 ligand; ICOSL, ICOS ligand; pMHCII, peptide–MHC class II; T, T cell.