Abstract
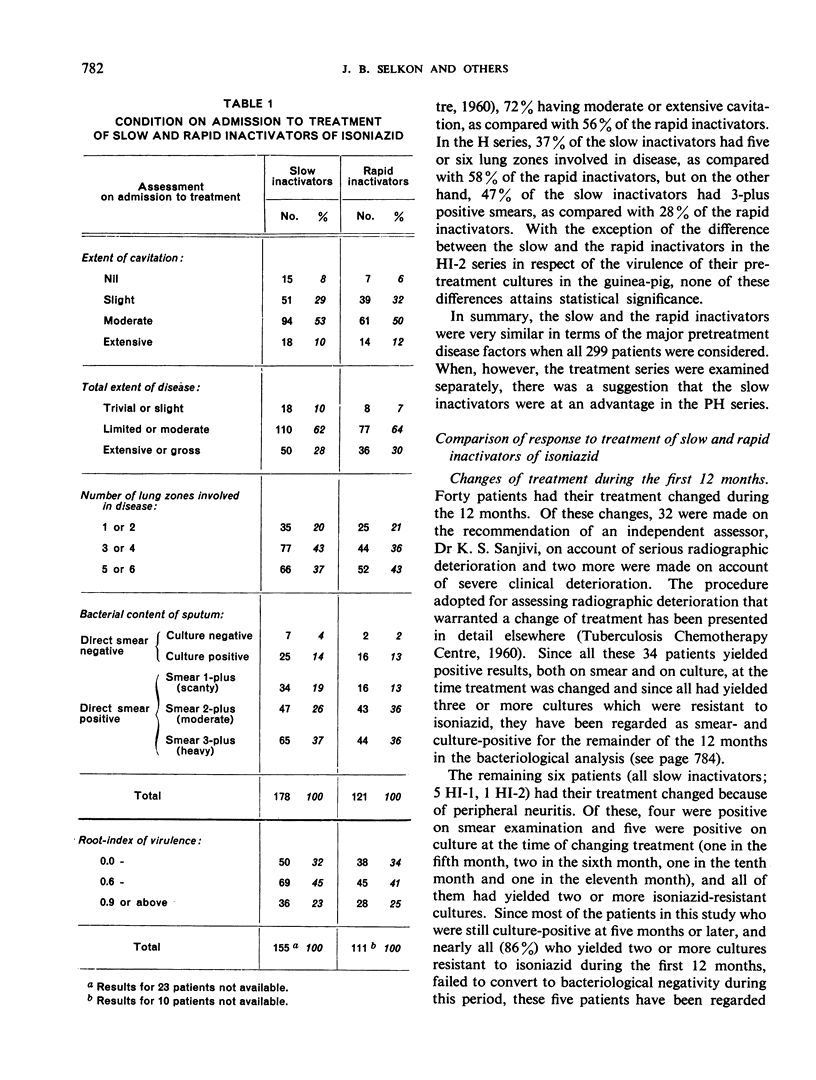
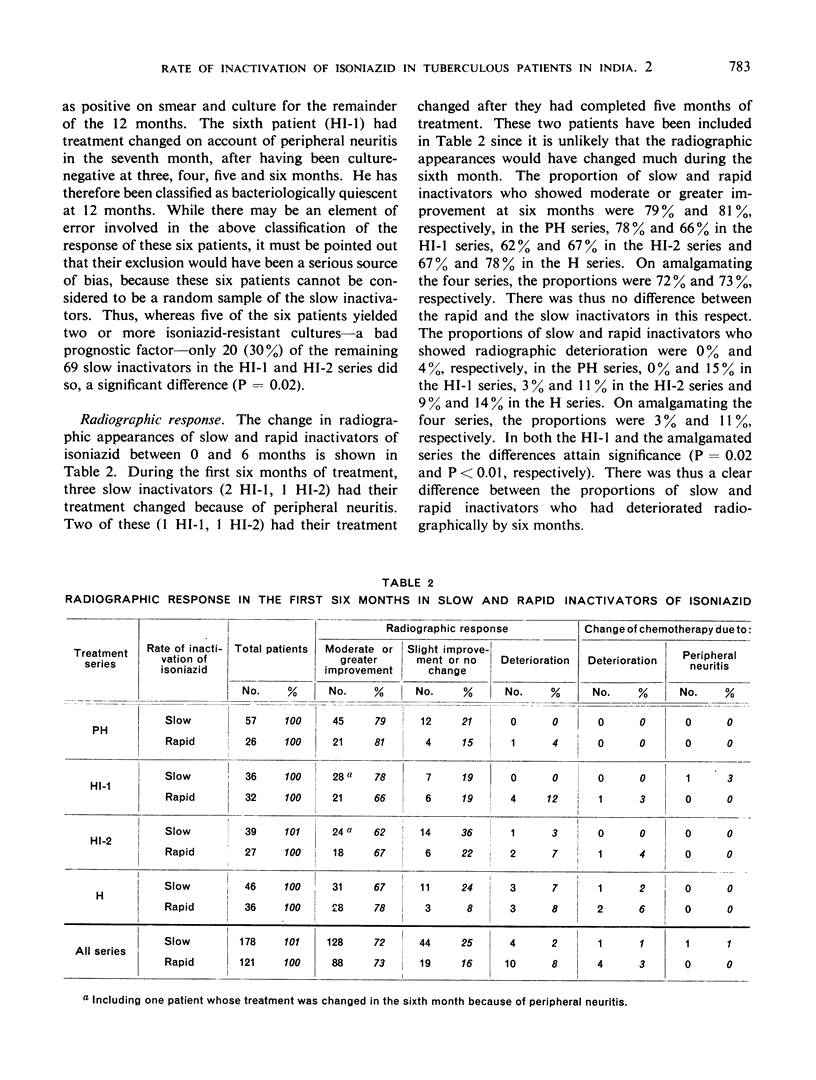
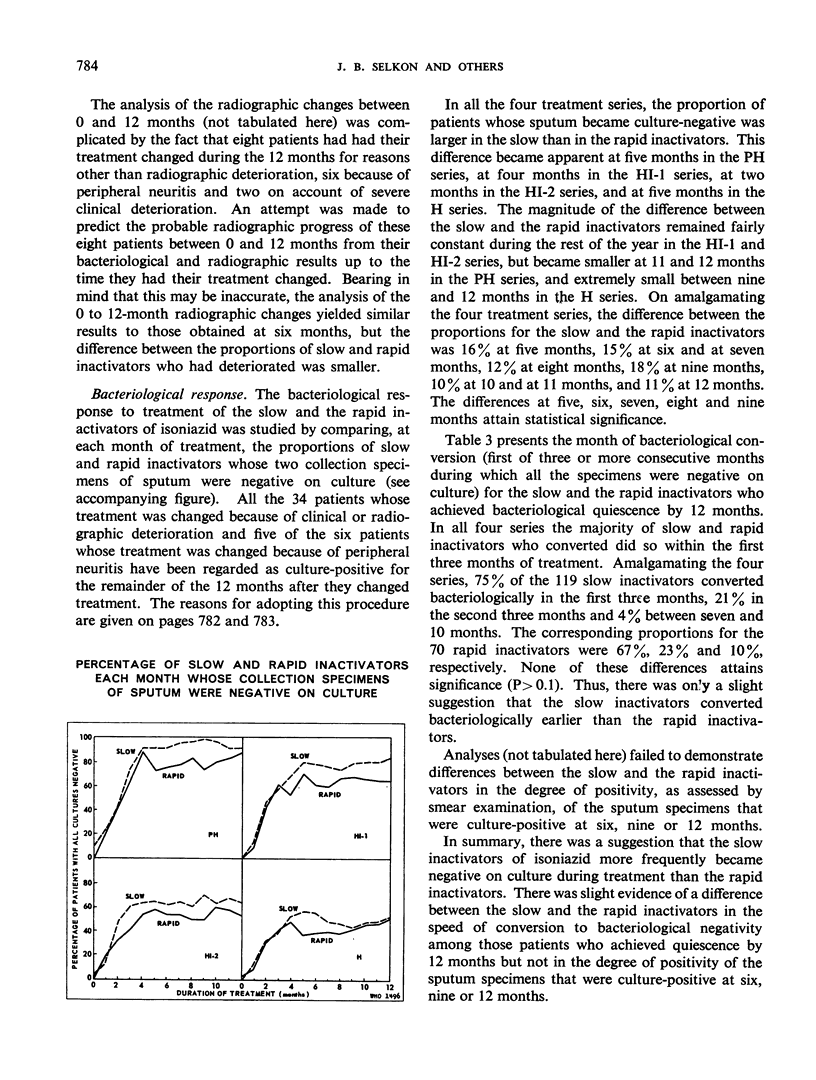
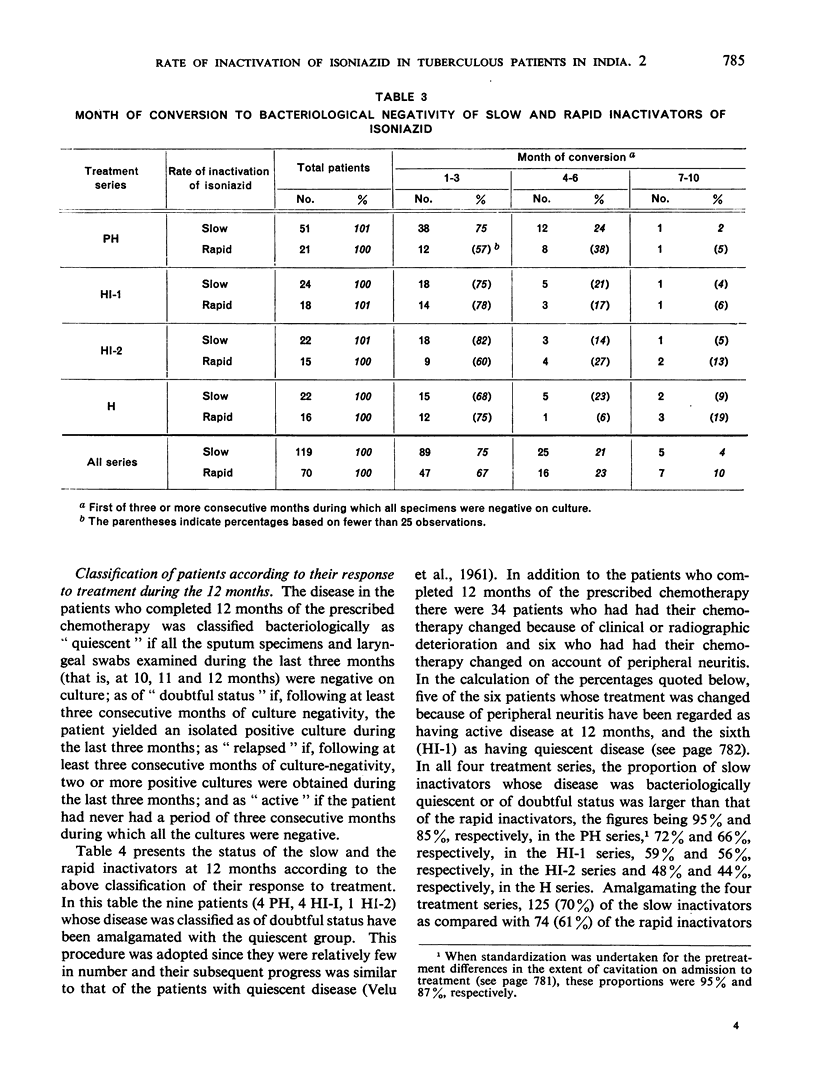
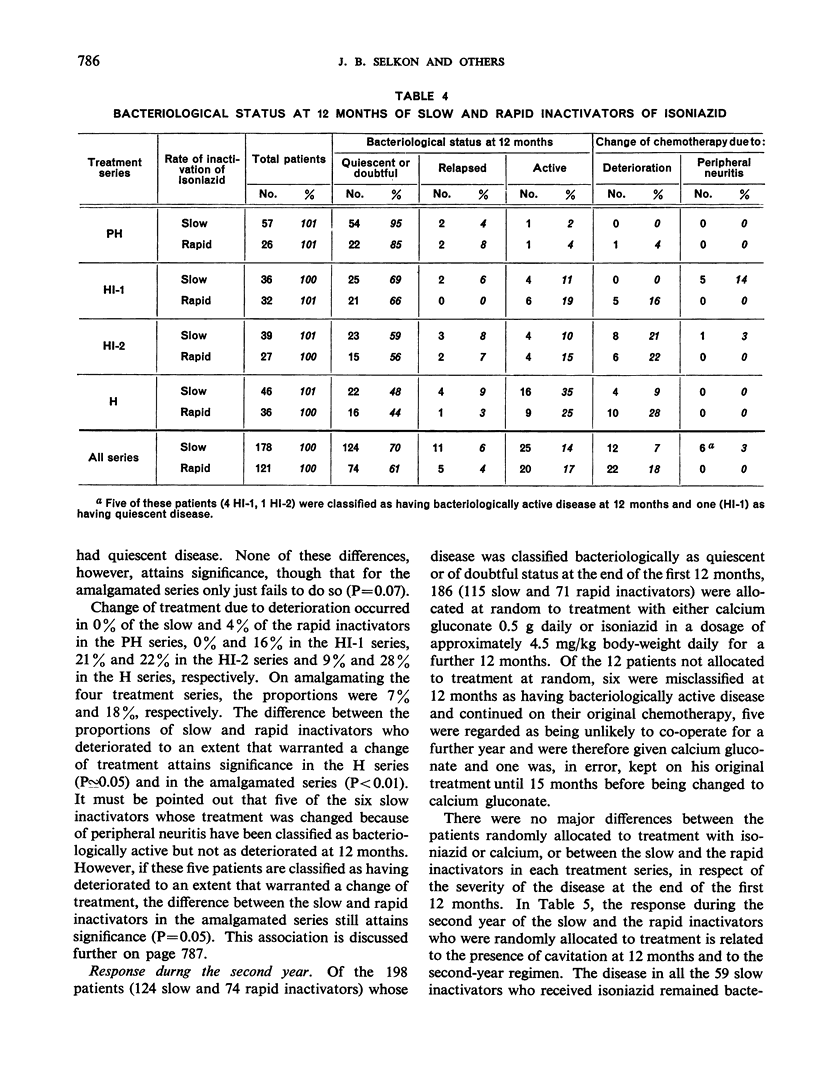
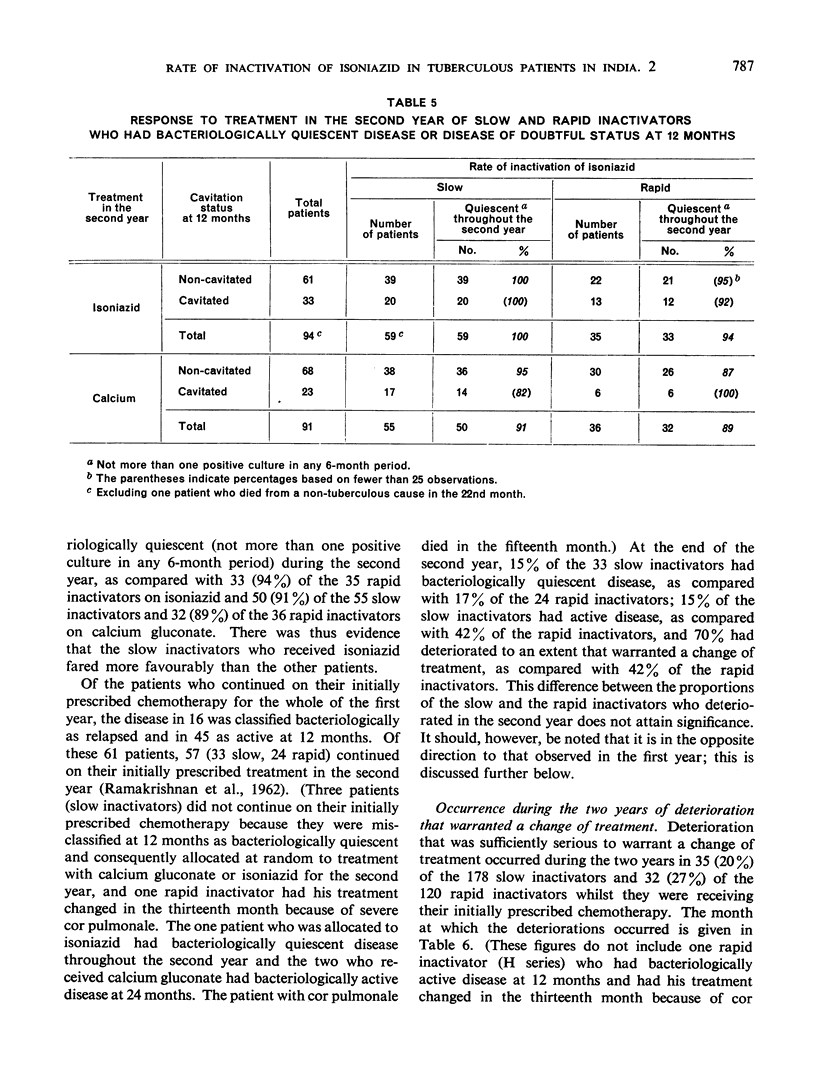
A series of studies on the rate of inactivation of isoniazid in Indian patients with pulmonary tuberculosis undergoing domiciliary chemotherapy with isoniazid, alone or in combination with p-aminosalicylic acid, has recently been undertaken by the Tuberculosis Chemotherapy Centre, Madras. In the first study, the serum isoniazid levels of the patients were determined four-and-a-half hours after intramuscular administration of a standard dose of 3 mg/kg body-weight of isoniazid and, according to whether the serum level was 0.58 μg/ml or above, or less than 0.58 μg/ml, the patient was classified as a slow or as a rapid inactivator. The present paper describes the second of these studies, in which the response to treatment of the slow and the rapid inactivators was compared. The results of this investigation suggested that there might be an association between response to treatment and rate of inactivation of isoniazid, since the slow inactivators were more often culture-negative during treatment and showed a higher proportion of individuals with bacteriologically quiescent disease at 12 months and a lower proportion with radiographic deterioration at six months than the rapid inactivators, while the slow inactivators who deteriorated radiographically or clinically to an extent warranting a change of treatment during the two years did so later than the corresponding rapid inactivators. There was slight evidence that the slow and the rapid inactivators differed in the speed of conversion to bacteriological negativity of those patients whose disease was bacteriologically quiescent at 12 months, but no evidence that they differed in the degree of positivity of sputum specimens that were positive on culture at six, nine or 12 months, or in the frequency with which the patients showed moderate or greater radiographic improvement at six months.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- COHN M. L., KOVITZ C., ODA U., MIDDLEBROOK G. Studies on isoniazid and tubercle bacilli. II. The growth requirements, catalase activities, and pathogenic properties of isoniazid-resistant mutants. Am Rev Tuberc. 1954 Oct;70(4):641–664. doi: 10.1164/art.1954.70.4.641. [DOI] [PubMed] [Google Scholar]
- COHN M. L., MANDEL W., MIDDLEBROOK G., RUSSELL W. F., Jr Serum isoniazid levels and catalase activities of tubercle bacilli from isoniazid-treated patients. Am J Med Sci. 1957 Jan;233(1):66–68. doi: 10.1097/00000441-195701000-00011. [DOI] [PubMed] [Google Scholar]
- DEVADATTA S., GANGADHARAM P. R., ANDREWS R. H., FOX W., RAMAKRISHNAN C. V., SELKON J. B., VELU S. Peripheral neuritis due to isoniazid. Bull World Health Organ. 1960;23:587–598. [PMC free article] [PubMed] [Google Scholar]
- EVANS D. A., MANLEY K. A., McKUSICK V. A. Genetic control of isoniazid metabolism in man. Br Med J. 1960 Aug 13;2(5197):485–491. doi: 10.1136/bmj.2.5197.485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GANGADHARAM P. R., BHATIA A. L., RADHAKRISHNA S., SELKON J. B. Rate of inactivation of isoniazid in South Indian patients with pulmonary tuberculosis. Bull World Health Organ. 1961;25:765–777. [PMC free article] [PubMed] [Google Scholar]
- HOLST E., MITCHISON D. A., RADHAKRISHNA S. Examination of smears for tubercle bacilli by fluorescence microscopy. Indian J Med Res. 1959 Sep;47:495–499. [PubMed] [Google Scholar]
- MITCHELL R. S., BELL J. C. Clinical implications of isoniazid blood levels in pulmonary tuberculosis. N Engl J Med. 1957 Nov 28;257(22):1066–1070. doi: 10.1056/NEJM195711282572202. [DOI] [PubMed] [Google Scholar]
- MITCHISON D. A., BHATIA A. L., RADHAKRISHNA S., SELKON J. B., SUBBAIAH T. V., WALLACE J. G. The virulence in the guinea-pig of tubercle bacilli isolated before treatment from South Indian patients with pulmonary tuberculosis. I. Homogeneity of the investigation and a critique of the virulence test. Bull World Health Organ. 1961;25:285–312. [PMC free article] [PubMed] [Google Scholar]
- OESTREICHER R., DRESSLER S. H., RUSSELL W. F., Jr, GROW J. B., MIDDLEBROOK G. Observations on the pathogenicity of isoniazid-resistant mutants of tubercle bacilli for tuberculous patients. Am Rev Tuberc. 1955 Mar;71(3 Pt 1):390–405. doi: 10.1164/artpd.1955.71.3-1.390. [DOI] [PubMed] [Google Scholar]
- VELU S., ANDREWS R. H., ANGEL J. H., DEVADATTA S., FOX W., GANGADHARAM P. R., NARAYANA A. S., RAMAKRISHNAN C. V., SELKON J. B., SOMASUNDARAM P. R. Progress in the second year of patients with quiescent pulmonary tuberculosis after a year of domiciliary chemotherapy, and influence of further chemotherapy on the relapse rate. Bull World Health Organ. 1961;25:409–429. [PMC free article] [PubMed] [Google Scholar]


