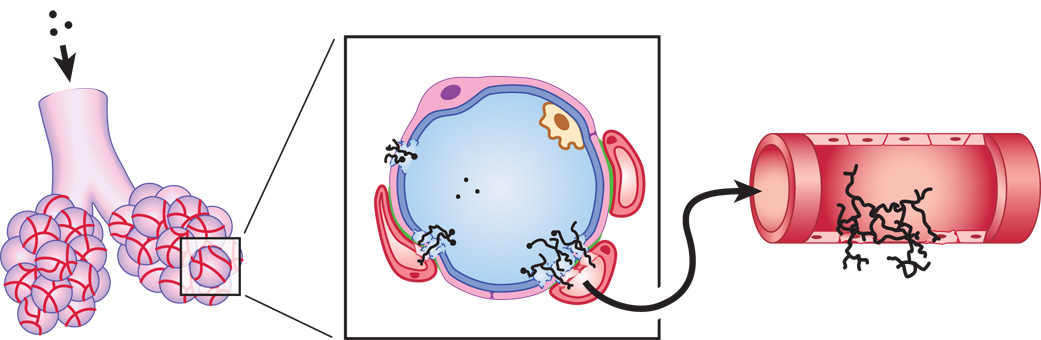
Fig. 1.
Schematic illustration of the pathogenesis of invasive aspergillosis (not drawn to scale). A. fumigatus conidia are small enough (2-3 µm in diameter) to reach the distal airways when inhaled (left). A cross section of the alveolar space is enlarged in the center panel, showing the close proximity of adjacent blood vessels in the interalveolar septum. In a susceptible host, the conidia are able to germinate and damage the blood-air interface. This barrier is comprised of a surfactant layer (blue), a type I pulmonary epithelial cell (pink), and an underlying microvascular endothelial cell (red). Loose interstitial tissue can sometimes be found between the epithelial and endothelial cells, but when the two cells are closely apposed the basal laminae fuse (green), making the barrier only 0.1 – 1.5 µm in thickness. The growing hyphae eventually penetrate this barrier and hyphal fragments are released into the blood, providing access to other organs by extravascular invasion (right panel).