Abstract
The purpose of this study was to determine the efficacy of providing (i) tailored injury prevention information (T-IPI) to parents and (ii) concurrent T-IPI to parents and providers to promote parent adoption of safety practices. During well-child visits, parents of children ages 4 and younger completed a computer assessment and were randomized to receive generic injury prevention information, T-IPI or T-IPI supplemented with a tailored summary for providers. Follow-up assessments were completed by telephone 1 month later. Parents receiving T-IPI alone or with supplementary provider information were more likely to report adopting a new injury prevention behavior than those receiving generic information (49 and 45%, respectively, compared with 32%; odds ratio = 2.0 and 1.9, respectively), and these effects were greatest among the least educated parents. In addition, more complicated behavior changes were reported by those receiving tailored information. Provider receipt of feedback did not result in significantly different provider–parent communication or change in parents' safety practices. Providing parents with individually tailored pediatric injury prevention information may be an effective method for delivering injury prevention anticipatory guidance. Tailoring may have particular utility for more complicated behaviors and for communication with less educated parents.
Introduction
Unintentional injury is the leading cause of preventable morbidity and mortality among US children and an important cause globally [1]. In 2002, the US mortality rate for unintentional injury in infants was 23.5 per 100 000 and 10.5 per 100 000 for children under age 4 [2], making it the sixth leading cause of infant mortality [2] and the number one cause of death among children between 1 and 4 years of age [3]. Furthermore, nonfatal unintentional injury causes a substantial rate of child morbidity [4].
Over 90% of all unintentional injuries in children <5 years old occur at home [5]; however, the types of injuries vary with developmental changes in children [6–8]. Preventing pediatric unintentional injury requires an understanding of the risk factors associated with each stage of development as well as appropriate risk-reducing actions. For example, the appropriate car restraint device varies with child age and weight, while home safety practices such as the use of stair gates and cabinet locks are prompted by anticipating a child's mobility and ability to access potentially dangerous places. Behaviors and devices for preventing unintentional injury in children at each stage are well-known; however, they are used at less than optimal rates [9–11].
Health care provider counseling at well-child visits is a potentially effective way to increase parental awareness of the risk of unintentional injury and to promote the use of appropriate injury prevention strategies. Parents consistently report a desire for provider recommendations [12, 13], and studies have demonstrated the effectiveness of such anticipatory guidance [14–19]. However, the frequency with which parents receive such guidance is inconsistent and below optimal levels [20, 21]. Reasons cited by clinicians for not providing injury prevention guidance are time constraints, competing demands and a lack of knowledge about how to approach the topic [22–24].
The use of educational materials delivered within the primary care setting combined with verbal guidance from a clinician may help circumvent these barriers. Such educational materials have traditionally been standard print media developed for a homogenous audience. When the educational needs of the audience are fairly similar, these materials may be sufficient to promote learning, teach skills or motivate behavior change. However, parents are likely to vary considerably in terms of awareness, knowledge, beliefs about child injuries and their child's risk of injury and safety behaviors performed. Educational materials tailored to such individual characteristics of parents and children have been shown to be more effective than nontailored information [25–29]. Tailored health communications use individual assessment data to customize the message to the needs and characteristics of the recipient. In a randomized study, Nansel et al. [11] provided tailored injury prevention information (T-IPI) or nontailored injury prevention information to parents before well-child visits. Participants receiving T-IPI reported greater behavior changes than did those receiving nontailored messages. Furthermore, although only one-fifth of parents reported they had discussed the materials with their provider, those parents demonstrated the greatest behavior change. However, this study was conducted at a single clinic and included only parents of children between the ages of 6 and 20 months. Moreover, feedback was not offered to the provider. Further research is needed to determine the applicability of these results to parents of children in a wider age range and to investigate the effects of systematic provider involvement.
The purpose of this study was to determine the efficacy of delivering (i) T-IPI to parents and (ii) concurrent T-IPI to parents and physicians on adoption of safety practices. The safety practices addressed in this study included age-appropriate behaviors and devices recommended by the American Academy of Pediatrics. We hypothesized that parents receiving tailored feedback would demonstrate greater adoption of injury prevention behaviors than those receiving generic feedback, and that tailored summary information provided to the physician would be associated with greater provider–parent discussion of unintentional injury prevention behavior and behavior change than those whose providers do not receive patient-specific prompts. We further hypothesized that there would be differences in the effectiveness of tailored information by demographic characteristics of the parent.
Method
Participants, setting and procedures
Parents of children age 4 and younger attending a well-child visit at one of three Midwestern pediatric clinics were invited to participate in the study. The patient population of two of the clinics is primarily low-income African-American children and parents; the third serves primarily low- to middle-income Caucasian children and parents. Based on data from our pilot study [11], we estimated a 20% difference in adoption rates of injury prevention behavior between groups and a follow-up rate of 75%. As a sample size of 150 participants per group resulted in >90% power to detect this difference, our targeted enrollment was 600. Participants were assigned to one of three study groups: (i) generic injury prevention information (G-IPI) provided to the parent, (ii) T-IPI provided to the parent or (iii) T-IPI provided to the parent plus supplementary tailored provider information (T-IPI + P). Participants were randomly assigned by computer to the first two intervention conditions until two-thirds of the planned number of participants had been recruited. All subsequent participants were then assigned to the third intervention condition. This design was selected to avoid contamination between conditions due to the provider's involvement in the third condition. That is, because the same physicians saw patients in each study group, it was important to delay the physician training and implementation of the third study condition until enrollment for the first two conditions was complete. Otherwise, the training and use of the physician-tailored feedback could have influenced physician interaction across all three study groups. Although this procedure for assigning parents to study groups was not strictly random, it was judged to be more important to control for this potential contamination between groups than to benefit from random assignment.
Parents were invited to participate by a trained research assistant when they arrived at the pediatric clinic for a well-child visit. Written consent was obtained from each participating parent, and participants completed the baseline assessment using a computer kiosk located in the clinic waiting room. Questions were presented on the computer screen, and programmed skip patterns were used so that parents answered only questions relevant to their child's age. Parents were provided with their printed injury prevention information from the kiosk immediately after completion of the assessment and attended their well-child visit per clinic routine.
For participants in the third intervention condition, the supplementary tailored provider information was printed from the kiosk at the same time as the parents' information and clipped to front of the patient's chart. Participants were informed that their provider would read a summary of the injury prevention information the parent received. Providers had received instruction regarding use of the tailored information during a staff meeting that occurred immediately before the third intervention condition began. They were informed about how the tailored summary was generated and what information was provided to parents and were encouraged to reinforce the information provided and discuss parents' questions or concerns.
One month following the clinic visit, participants completed a follow-up telephone assessment, completed by interviewers blind to treatment group allocation. To facilitate retention, both primary and alternate phone numbers were collected, consent for medical record review to identify updated phone numbers was obtained and on-line telephone directories were used. Following completion of the study, providers were also contacted by telephone to complete a brief questionnaire regarding their perceptions of the utility of the intervention. The study was approved by both the National Institute of Child Health and Human Development and the Saint Louis University Institutional Review Boards.
Measures
Baseline measures included participants' current injury prevention behaviors, injury prevention beliefs and demographic items. Injury prevention behaviors included 35 age-appropriate practices by parents to reduce the risk of injury in six areas: motor vehicle injuries, burns, falls, poisoning, airway obstruction and drowning. (Each parent received the subset of injury prevention practices relevant to the child's age.) Injury prevention beliefs included parents' perception of the importance of injury prevention and other child health issues to their provider, as well as specific beliefs that may inhibit injury prevention behaviors including perceived lack of control over injury, using supervision rather than injury prevention measures, teaching the child to obey rather than using injury prevention measures and the perceived normalcy of minor injuries.
During the follow-up assessment, participants were queried about their perceptions regarding the injury prevention information they received, including whether they had read the information and whether they had discussed it with family, friends or their health care provider. They were also asked a nine-item scale (alpha = 0.97) assessing the persuasiveness of the intervention materials, for example, the extent to which it helped them know what safety measures to take and encouraged them to take safety precautions. Each of these items was rated on a 1–10 scale ranging from ‘not at all’ to ‘a lot’, and an overall persuasiveness score was calculated as the mean of items. Finally, participants were asked to identify any new injury prevention behavior they took as a result of the information they received. Their responses were coded into the categories of injury prevention practices addressed in the intervention.
Following completion of the study, providers completed a brief telephone survey regarding their experience with and reactions to the intervention. They were queried regarding the extent to which they read and discussed the provider summary information sheet and were asked to respond on a four-point ‘strongly disagree’ to ‘strongly agree’ scale to eight questions regarding the usefulness of the summary information (e.g. the extent to which the feedback reminded them to talk about injury prevention; helped them decide what to talk about). Open-ended feedback regarding their perceptions of the usefulness of the program was also solicited.
Intervention conditions
In order to focus their attention on high priority areas for change, participants assigned to tailored conditions received tailored information on two priority safety practices. To select these two priority areas, each injury prevention behavior assessed was assigned a numerical value corresponding to the severity and prevalence of associated risk. These values were based on a review of the literature [e.g., 30, 31] and consensus of the project team. For each participant, the two injury areas with the highest scores were selected. The layout and message library for the tailored information were stored in a database file, and upon completion of the questionnaire, the appropriate messages were printed on the feedback form to generate the tailored information.
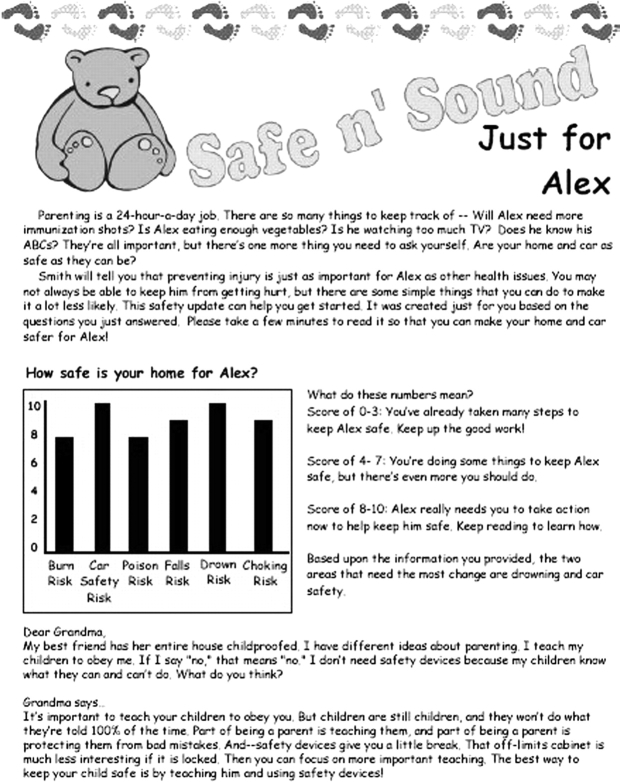
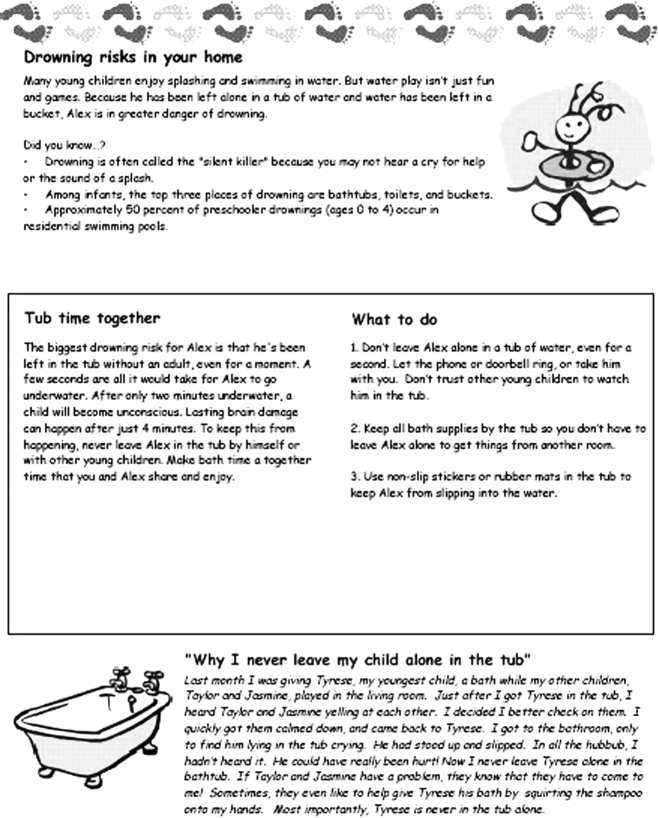
The T-IPI consisted of three pages printed on two-color stationary with child-oriented graphics and personalized with the child's name. The front page (Fig. 1) included a bar graph of the participant's injury risk score for each of the six risk areas, explanation of these scores and tailored motivational messages regarding safety practices. Pages two and three (Fig. 2) provided detailed information about the child's two priority areas. Each page included sections on the importance and relevance of the injury area, specific behaviors contributing to the child's risk for injury, specific steps the parent should take to reduce risk and a parent testimonial describing why and how she/he decided to use the specific safety practice being recommended. The messages were designed to address relevant social cognitive determinants of behavior. For example, the introductory message nested injury prevention within the context of the many important responsibilities associated with parenting to increase expectancies regarding injury prevention behaviors, and parent-reported beliefs inhibiting injury prevention behaviors were addressed in a tailored advice column. Specific information about benefits of the target behavior was designed to increase positive outcome expectations, and parent testimonials regarding each behavioral recommendation then provided an opportunity for observational learning, potentially influencing both perceived social norms and self-efficacy for injury prevention behaviors.
Fig. 1.
Example page 1 of tailored injury prevention information.
Fig. 2.
Example page 2 and 3 of tailored injury prevention information.
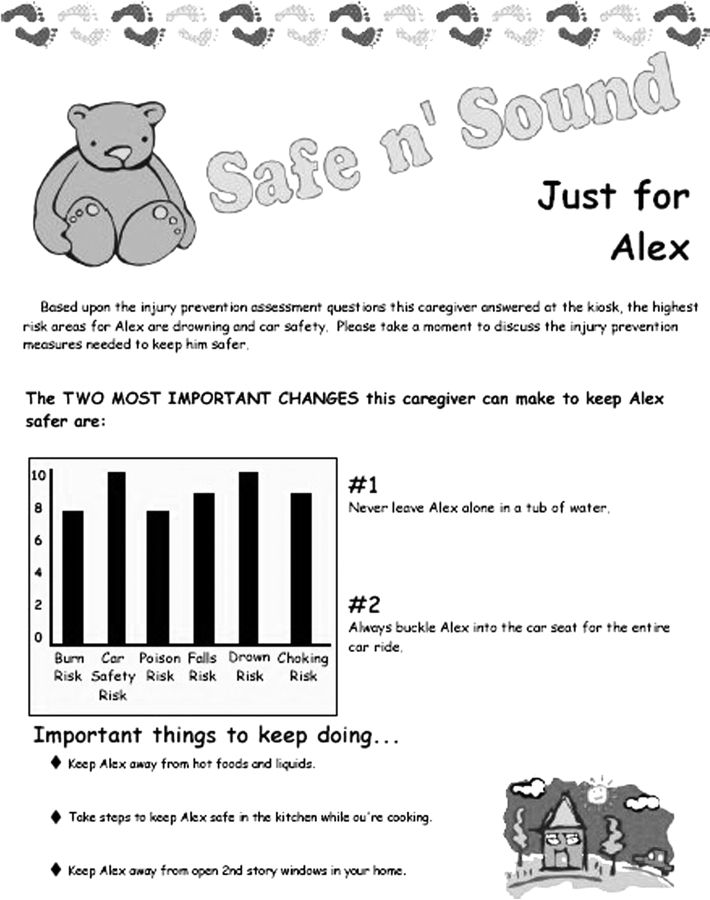
The tailored information for providers (Fig. 3) consisted of a one-page summary including the bar graph of injury risk score for each of the six risk areas and a listing of the two priority behavior changes. Providers were encouraged to reinforce the importance of the behavior changes listed and address any questions or concerns the parent may have regarding their implementation.
Fig. 3.
Example tailored provider information.
The G-IPI (control condition) contained general information about injury risks to children, along with age-appropriate behavioral recommendations for safety practices. It contained information and a recommendation on all the injury areas assessed in this study and was designed to be similar to educational materials frequently used in clinical practice. It was printed on the same stationary as the tailored materials. Both tailored and generic materials were written at a sixth to eighth grade level; terminology specific to injury prevention practices was the primary determinant of differences in reading level.
Analysis
The primary outcomes for this study were provider–parent communication and parental adoption of injury prevention behaviors. Secondary outcomes were participant reactions to the information, including reading of the information, perceived persuasiveness of the information and discussing the information with friends or family. Descriptive analyses, multinomial logistic regression, chi-square analyses and analysis of variance were used to answer the research questions. While analysis of baseline data revealed no significant differences between treatment groups, potential confounders (e.g. ethnic group) were included in the analyses as control variables.
Results
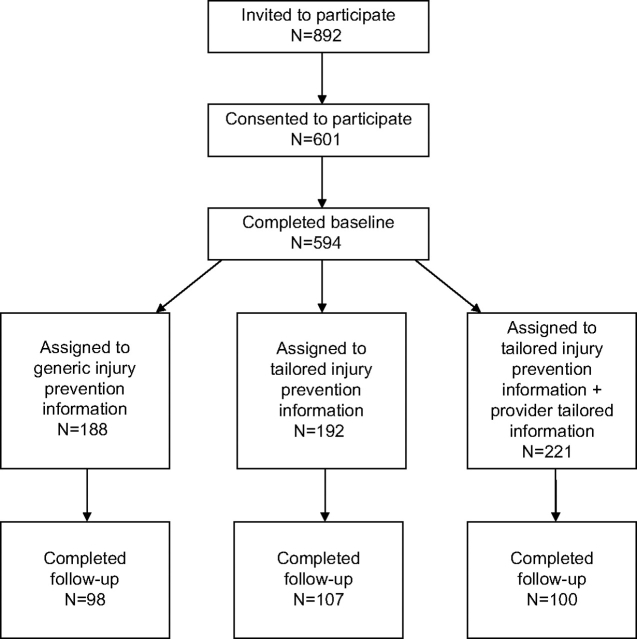
Flow of participants through the study is presented in Fig. 4. Of those invited to participate, 69% consented. Of those completing the baseline assessment, 51% competed the follow-up assessment. Reasons for participants being lost to follow-up included participant refusal (35%), no longer at number or number no longer in service (34%), unable to reach after repeated (mean of 10.4) attempts (27%) and use of a telephone service that blocks calls from all phone numbers not previously identified by the user (4%). There were no differences between treatment groups in follow-up rates. Parents who owned their own homes (60% versus 48%, χ2 = 6.29, df1; P = 0.01) and those with a college education (57% versus 48%, χ2 = 4.52, df1; P = 0.03) were more likely to complete follow-up. Non-African-American minorities, accounting for 10% of the sample, were less likely to complete follow-up (37% versus 54% African-Americans and 51% Caucasians, χ2 = 6.01, df2; P = .05). There were no significant differences in demographic characteristics or baseline rates of injury prevention behaviors between treatment groups. Sample characteristics are provided in Table I. Baseline rates of injury prevention behaviors are reported elsewhere [32]. Adherence to each of the 35 injury prevention behaviors assessed ranged from 39 to 98%.
Fig. 4.
Flow of participant through study.
Table I.
Participant demographics
| G-IPI n = 98, n (%) | T-IPI n = 107, n (%) | T-IPI + P n = 100, n (%) | |
| Age | |||
| 20 and under | 25 (25.8) | 29 (27.4) | 19 (19.0) |
| 21–25 | 29 (29.9) | 39 (36.8) | 40 (40.0) |
| 26–30 | 21 (21.6) | 15 (14.2) | 17 (17.0) |
| 31–35 | 8 (8.2) | 12 (11.3) | 10 (10.0) |
| >35 | 14 (14.4) | 11 (10.4) | 14 (14.0) |
| Race/ethnicity | |||
| Caucasian | 28 (28.9) | 31 (29.2) | 44 (44.0) |
| African-American | 64 (66.0) | 67 (63.2) | 47 (47.0) |
| Other | 5 (5.1) | 8 (7.5) | 9 (9.0) |
| Education | |||
| Less than high school degree | 11 (11.3) | 11 (10.4) | 19 (19.0) |
| High school degree or equivalent | 47 (48.5) | 52 (49.1) | 36 (36.0) |
| Any college | 39 (40.2) | 43 (40.5) | 45 (45.0) |
| Relationship to child | |||
| Mother/stepmother | 79 (80.6) | 97 (90.7) | 84 (84.0) |
| Father/stepfather | 10 (10.2) | 3 (2.8) | 5 (5.0) |
| Grandparent/other | 9 (9.2) | 7 (6.5) | 11 (11.0) |
| Age of child | |||
| 0–6 months | 25 (25.5) | 35 (32.7) | 33 (33.0) |
| 7–11 months | 14 (14.3) | 13 (12.1) | 10 (10.0) |
| 12–23 months | 24 (24.5) | 25 (23.4) | 20 (20.0) |
| 2 years | 15 (15.3) | 16 (15.0) | 21 (21.0) |
| 3 years | 13 (13.3) | 12 (11.2) | 9 (9.0) |
| 4 years | 7 (7.1) | 6 (5.6) | 7 (7.0) |
| Sex of child | |||
| Male | 47 (48.0) | 54 (50.5) | 59 (59.0) |
| Female | 51 (52.0) | 53 (49.5) | 41 (41.0) |
| Household income | |||
| Less than $10 000 | 43 (44.3) | 40 (38.5) | 40 (40.8) |
| $10 000–$14 999 | 17 (17.5) | 18 (17.3) | 17 (17.3) |
| $15 000–$24 999 | 17 (17.5) | 19 (18.3) | 12 (12.2) |
| $25 000–$49 999 | 11 (11.3) | 21 (20.2) | 21 (21.4) |
| $50 000 and over | 9 (9.3) | 6 (5.8) | 8 (8.1) |
| Own or rent home | |||
| Own | 24 (24.5) | 33 (30.8) | 34 (34.0) |
| Rent | 74 (75.5) | 74 (69.2) | 69 (69.0) |
All groups rated the information high on its persuasiveness, with no differences observed between treatment conditions (mean = 8.0 G-IPI, 8.4 T-IPI and 8.5 T-IPI + P; F = 1.31; df2; P = 0.27). Treatment group differences in study outcomes are shown in Table II. The treatment groups showed significantly different rates of reading the injury prevention information, with 33.7% of those receiving G-IPI reporting reading all of the material, compared with 49.5% of those receiving tailored information (T-IPI) and 57% of those receiving tailored + provider injury prevention information (T-IPI + P). There were no differences between groups in the frequency with which parents discussed the information with their provider or others.
Table II.
Treatment group differences on study outcomes
| Outcome | G-IPI n = 98 | T-IPI n = 107 | T-IPI + P n = 100 | |||
| n (%) | OR (95% CI)a | n (%) | OR (95% CI)a | n (%) | OR (95% CI)a | |
| Read all information | 33 (33.7) | [Referent] | 53 (49.5) | 2.0 (1.1–3.5)* | 57 (57.0) | 2.6 (1.4–4.7)** |
| Discussed information with friends or family | 60 (61.2) | [Referent] | 76 (71.0) | 1.5 (0.9–2.8) | 63 (63.0) | 1.1 (0.6–1.9) |
| Discussed information with provider | 32 (32.7) | [Referent] | 37 (34.6) | 1.2 (0.6–2.1) | 28 (28.0) | 0.9 (0.5–1.6) |
| Adopted new injury prevention behavior | 31 (31.6) | [Referent] | 52 (48.6) | 2.0 (1.1–3.6)* | 45 (45.0) | 1.9 (1.0–3.4)* |
OR, odds ratio; CI, confidence interval.
ORs adjusted for parent age, race, education level and home ownership.
*P < 0.05, **P < 0.01
A significantly greater proportion of participants receiving tailored information reported adopting a new injury prevention behavior as a result of the information they received (Table II). Among those receiving tailored information, 48.6% (T-IPI) and 45.0% (T-IPI + P) reported adopting a new behavior compared with 31.6% of those receiving generic information (G-IPI). Post hoc analyses indicated that that tailored groups were not significantly different from each other (χ2 = 0.27; df1; P = 0.60) but were significantly different from the generic group (χ2 = 6.33; df1; P = 0.01). Thus, the tailored study groups were combined for subsequent analyses.
Across treatment groups, there were no differences in adoption of injury prevention behaviors based on participant age, race, education, income or home ownership. However, the effect of generic versus tailored information differed significantly by education level (Breslow-Day χ2 = 5.91; df2; P = 0.05), with greater differences between the effect of tailored versus generic information for those with less education (Table III). Among participants with less than a high school degree, and among those with a high school degree or equivalent, tailored materials were significantly more effective than generic material in affecting behavior change (χ2 = 6.22; df1; P = 0.01 and χ2 = 5.68; df1; P =0.02, respectively); however, there were no differences in effectiveness for those with any college education (χ2 = 0.10; df1; P = 0.75).
Table III.
Respondents reporting adoption of a new injury prevention behavior by education and tailored status
| n adopting/total n (% adopting) | |||
| Generic | Tailored | Total | |
| <High school degree | 0/11 (0.0) | 12/30 (40.0) | 12/41 (29.3) |
| High school degree/equivalency | 13/47 (27.7) | 43/88 (48.9) | 56/135 (41.5) |
| Any college | 17/39 (43.6) | 41/88 (46.6) | 58/127 (45.7) |
Across study groups, the most common behavior changes reported were those pertaining to the prevention of burns, poisoning and airway obstruction. While there were no significant differences between study groups in the use of any safety practice at baseline (data not shown), there were several notable differences at follow-up in the specific practices adopted. One notable difference between groups was that among the tailored groups, 15% of those reporting adoption of a new injury prevention behavior had made a change in car seat use, while none of the participants in the G-IPI condition reported adopting any new behavior related to car seat use. Additional behaviors adopted by those reporting behavior changes in the tailored groups but not by any of those receiving generic information included avoiding certain choking risk foods (10%) and no longer leaving their child alone in the tub (4%). Conversely, adoption of outlet covers was more common among those receiving generic information. Among those reporting a behavior change, 31% of those in the generic information group reported getting outlet covers, compared with 16% of those receiving tailored information.
Health care providers involved in the study included five physicians and one nurse practitioner. Four of the six providers reported that they always discussed at least one of the injury prevention behaviors listed on their feedback sheet; one discussed it most of the time and one about half the time. The providers all believed the information was useful and assisted them in providing injury prevention anticipatory guidance. Providers commented that the information was especially useful because it both served as a reminder to them and allowed them to focus their discussion specifically on the behaviors the patient needed to change rather than giving advice on practices the parent had already adopted. They also believed that the process engaged parents in a more active way than typical provision of educational information.
Discussion
Parents frequently receive a great deal of information on various health-related topics, and providers must address numerous health-related concerns during the course of a brief well-child visit. Concerns about injury prevention may become secondary to more immediate and apparent issues such as immunizations or nutrition. Moreover, parent recall of anticipatory guidance decreases as the number of topics addressed increases [33]. Thus, an intervention that could efficiently and effectively provide injury prevention information could have considerable utility in pediatric practice. Findings from this study support the efficacy of individually tailored injury prevention information for promoting adoption of injury prevention measures by parents of young children. Those receiving tailored information were more likely to adopt an injury prevention behavior than those receiving generic information. This effect was observed specifically among those with a lower education level. As health promotion interventions are often more effective with higher educated populations, a program that is effective for those with less education may be of particular value.
Those receiving tailored information were also more likely to adopt a higher impact behavior, such as consistently using the car seat or not leaving a child alone in the tub. This suggests that for simple behaviors (e.g. using outlet covers, a low-cost one-time behavior), generic information may be sufficient, whereas more complicated behaviors (e.g. installing and using car seats, a higher-cost and ongoing behavior) benefit from a tailored approach. Thus, the use of individually tailored injury prevention information may be a useful method to enhance the provision of effective injury prevention education in the pediatric primary care environment.
This study adds to a growing body of evidence that tailoring can be effective in promoting health-related behaviors for a range of issues among parents of young children, including immunization [34], nutrition [35] and injury prevention [11, 36]. One explanation for effects of tailored health communication, based on the Elaboration Likelihood Model [37], suggests that individuals are more motivated and likely to process information when they perceive it to be personally relevant. In support of this explanation, studies have shown that tailored information stimulates greater cognitive activity about the health topic of interest than nontailored information [38]. This in-depth processing, or ‘elaboration', is thought to lead to greater and more lasting changes in attitudes, which in turn may facilitate changes in behavior [39, 40]. Although this study did not assess parents’ processing of the injury prevention information, the finding that tailored materials were more likely to be read is consistent with this explanation. In models of communication and persuasion effects, paying attention to a stimulus is an important prerequisite to understanding [41]. Another explanation of tailoring effects is that the expectation of customization—for example, simply telling an individual they will be receiving individualized information—leads to more positive evaluations of the materials [42]. However, the lack of differences between the perceived persuasiveness of the tailored and generic materials does not support this explanation.
Contrary to expectations, the addition of provider-directed tailored feedback did not enhance intervention effectiveness. Previous research has indicated positive outcomes associated with provider recommendations for behavior change [14, 43, 44]. However, the provision of provider tailored feedback in this study did not result in greater provider discussion of injury prevention recommendations, according to parent reports. The lack of effect observed in this study may indicate a need for more extensive training regarding use of the program or may suggest that programs need to be integrated more fully or differently into standard office protocols. While the providers reported discussing the tailored information with most parents, few parents recalled such discussion. This discrepancy is common when comparing patient and provider reports of communication [45] and could be the result of a social desirability reporting bias among the health care providers or could reflect parents' not remembering these discussions. Thus, it cannot be determined from this study whether increased or systematic provider–parent interaction would result in greater behavior change.
A notable strength of this study is that it was conducted with a lower socioeconomic status sample. Injury prevention and other health promotion interventions may be especially challenging with this population, given the degree of environmental stressors and competing priorities that are often present. These populations are more difficult to reach, especially through traditional print media. By providing highly relevant and targeted information, a tailored approach may be more successful in overcoming impediments to the effectiveness of print health-related information. For practices serving lower income and less educated populations, an effective, low-cost, low-intensity intervention that can be integrated into the existing health care system could have particular appeal and utility.
The selection of this study population resulted in a low follow-up response rate, however. During the time in which the study was conducted, the population served by the participating clinics consisted of 28–50% families with young children living below the poverty level [46]. While this suggests that public health programs are very much needed, this population is also harder to follow-up since participants are less likely to have regular access to phones and may often change housing. The low follow-up rate is also a function of many advances in telephone capabilities. With caller ID, call blocking and other phone options, there has been a decrease in the response percentages of telephone surveys. The 2000 Summary Data Quality Report of the Behavioral Risk Factor Surveillance System [47] shows that median response rates have declined steadily from 63.2% in 1996 to 48.9% in 2000. In 2003, the overall response rate for the Behavioral Risk Factor Surveillance System in Missouri was 54.2%, modestly higher than our follow-up response rate of 51%. This response rate is an important limitation of this study, adversely affecting power and of concern for internal validity. However, the treatment groups did not differ in follow-up rates and very minimal demographic differences between responders and nonresponders were observed. Moreover, the differences observed would have more likely created a bias in the direction of not observing a treatment effect, as those with a college education showed the least treatment effect. As such, we conclude that the response rate is not a significant threat to the internal validity of this study.
The rates of injury prevention adoption in this sample were lower than in our pilot study [11], likely affected by the nature of the current study population. This along with the lower follow-up rate reduced the statistical power of this study, limiting more extensive analyses. As multiple outcomes were assessed, analyses included the use of multiple significance tests. However, between-group findings regarding reading of the information and adoption of injury prevention behavior demonstrated similar patterns, suggesting that results are likely attributable to differences in the information rather than chance.
The use of T-IPI integrated within the pediatric primary care environment may be an effective and efficient way to enhance the provision of injury prevention anticipatory guidance and increase the use of safety practices by parents of young children. However, despite the demonstrated efficacy of tailored information compared with generic, adoption of injury prevention behaviors as a result of the information occurred in less than half of the recipients. Greater rates of behavior change will likely require more intensive efforts than unsolicited provision of information. Future work in this area should continue to explore avenues by which the health care provider could increase parent activation and further enhance the effectiveness of this form of print media.
Funding
Intramural Research Program of the National Institutes of Health, National Institute of Child Health and Human Development.
Conflict of interest statement
None declared
References
- 1.Krug E. Injury: A Leading Cause of the Global Burden of Disease. Geneva: World Health Organization; 1999. [Google Scholar]
- 2.Kochanek KD, Murphy SL, Anderson RN, et al. Deaths: final data for 2002. Natl Vital Stat Rep. 2004;53:1–116. [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Injury Fact Book. 2006. Available at: http://www.cdc.gov/ncipc/fact_book/factbook.htm. Accessed: 14 September, 2007. [Google Scholar]
- 4.Baker SP, O'Neill B, Ginsburg MJ, et al. The Injury Fact Book. New York: Oxford University Press; 1991. [Google Scholar]
- 5.Rivara FP, Calonge N, Thompson RS. Population-based study of unintentional injury incidence and impact during childhood. Am J Public Health. 1989;79:990–4. doi: 10.2105/ajph.79.8.990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bass JL, Mehta KA. Developmentally-oriented safety surveys. Clin Pediatr. 1980;19:350–6. doi: 10.1177/000992288001900508. [DOI] [PubMed] [Google Scholar]
- 7.Rivara FP. Developmental and behavioral issues in childhood injury prevention. J Dev Behav Pediatr. 1995;16:362–70. [PubMed] [Google Scholar]
- 8.Rivara FP, Mueller BA. The epidemiology and causes of childhood injuries. J Soc Issues. 1987;43:13–31. [Google Scholar]
- 9.Gielen AC, Wilson M, Faden R, et al. In-home injury prevention practices for infants and toddlers: the role of parental beliefs, barriers, and housing quality. Health Educ Q. 1995;22:85–95. doi: 10.1177/109019819502200108. [DOI] [PubMed] [Google Scholar]
- 10.Glik DC, Greaves PE, Kronenfeld JJ, et al. Safety hazards in households with young children. J Pediatr Psychol. 1993;18:115–31. doi: 10.1093/jpepsy/18.1.115. [DOI] [PubMed] [Google Scholar]
- 11.Nansel TR, Weaver N, Donlin M, et al. Be safe: the effect of tailored communications for pediatric injury prevention provided in a primary care setting. Patient Educ Couns. 2002;46:175–90. doi: 10.1016/s0738-3991(01)00211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eichelberger MR, Gotschall CS, Feely HB, et al. Parental attitudes and knowledge of child safety. Child Safety. 1990;144:714–20. doi: 10.1001/archpedi.1990.02150300112029. [DOI] [PubMed] [Google Scholar]
- 13.Schuster MA, Duan N, Regalado M, et al. Anticipatory guidance: what information do parents receive? What information do they want? Arch Pediatr Adolesc Med. 2000;154:1191–8. doi: 10.1001/archpedi.154.12.1191. [DOI] [PubMed] [Google Scholar]
- 14.Bass JL, Christoffel KK, Widome M, et al. Childhood injury prevention counseling in primary care settings: a critical review of the literature. Pediatrics. 1993;92:544–50. [PubMed] [Google Scholar]
- 15.DiGuiseppi C, Roberts IG. Individual-level injury prevention strategies in the clinical setting. Future Child. 2000;10:53–82. [PubMed] [Google Scholar]
- 16.Jordan EA, Duggan AK, Hardy JB. Injuries in children of adolescent mothers: home safety education associated with decreased injury risk. Pediatrics. 1993;91:481–7. [PubMed] [Google Scholar]
- 17.Mock C, Arreola-Risa C, Trevino-Perez R, et al. Injury prevention counseling to improve safety practices by parents in Mexico. Bull World Health Organ. 2003;81:591–8. [PMC free article] [PubMed] [Google Scholar]
- 18.Nelson CS, Wissow LS, Cheng TL. Effectiveness of anticipatory guidance: recent developments. Curr Opin Pediatr. 2003;15:630–5. doi: 10.1097/00008480-200312000-00015. [DOI] [PubMed] [Google Scholar]
- 19.Posner JC, Hawkins LA, Garcia-Espana F, et al. A randomized, clinical trial of a home safety intervention based in an emergency department setting. Pediatrics. 2004;113:1603–8. doi: 10.1542/peds.113.6.1603. [DOI] [PubMed] [Google Scholar]
- 20.Gielen AC, McDonald EM, Forrest CB, et al. Injury prevention counseling in an urban pediatric clinic. Arch Pediatr Adolesc Med. 1997;151:146–51. doi: 10.1001/archpedi.1997.02170390036007. [DOI] [PubMed] [Google Scholar]
- 21.Morrongiello BA, Hillier L, Bass M. What I said versus what you heard: a comparison of physicians and parents reporting of anticipatory guidance on child safety issues. Inj Prev. 1995;1:223–7. doi: 10.1136/ip.1.4.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Butler RN, Todd KH, Kellerman AL, et al. Injury-control education in six U.S. medical schools. Acad Med. 1998;73:524–8. doi: 10.1097/00001888-199805000-00020. [DOI] [PubMed] [Google Scholar]
- 23.Cohen LR, Runyan CW. Barriers to pediatric injury prevention counseling. Inj Prev. 1999;5:36–40. doi: 10.1136/ip.5.1.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jaen CR, Stange KC, Nutting PA. Competing demands of primary care: a model for the delivery of clinical prevention services. J Fam Pract. 1994;38:166–71. [PubMed] [Google Scholar]
- 25.Brug J, Campbell M, Van Assema P. The application and impact of computer-generated personalized nutrition education: a review of the literature. Patient Educ Couns. 1999;36:145–56. doi: 10.1016/s0738-3991(98)00131-1. [DOI] [PubMed] [Google Scholar]
- 26.Kreuter M, Oswald DL, Bull FC, et al. Are tailored health education materials always more effective than non-tailored materials? Health Educ. 2000;15:305–15. doi: 10.1093/her/15.3.305. [DOI] [PubMed] [Google Scholar]
- 27.Kreuter MW, Strecher VJ, Glassman B. One size does not fit all: the case for tailored print materials. Ann Behav Med. 1999;21:276–83. doi: 10.1007/BF02895958. [DOI] [PubMed] [Google Scholar]
- 28.Skinner C, Campbell M, Bimer B, et al. How effective is tailored print communication. Ann Behav Med. 1999;21:290–8. doi: 10.1007/BF02895960. [DOI] [PubMed] [Google Scholar]
- 29.Strecher VJ. Computer-tailored smoking cessation materials: a review and discussion. Patient Educ Couns. 1999;36:107–17. doi: 10.1016/s0738-3991(98)00128-1. [DOI] [PubMed] [Google Scholar]
- 30.Cohen LR, Runyan CW, Downs SM, et al. Pediatric injury prevention counseling priorities. Pediatrics. 1997;99:704–10. doi: 10.1542/peds.99.5.704. [DOI] [PubMed] [Google Scholar]
- 31.Grossman DC. The history of injury control and the epidemiology of child and adolescent injuries. Future Child. 2000;10:23–52. [PubMed] [Google Scholar]
- 32.Vladutiu CJ, Nansel TR, Kreuter MW, et al. Differential strength of association of child injuryprevention attitudes and beliefs on practices: a case for audience segmentation. Inj Prev. 2006;12:35–40. doi: 10.1136/ip.2004.007153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Barkin SL, Scheindlin B, Brown C, et al. Anticipatory guidance topics: are more better? Ambul Pedicatr. 2005;5:372–6. doi: 10.1367/A04-2131R1.1. [DOI] [PubMed] [Google Scholar]
- 34.Kreuter M, Caburnay C, Chen J, et al. Effectiveness of individually tailored calendars in promoting childhood immunization in urban public health centers. Am J Public Health. 2004;94:122–7. doi: 10.2105/ajph.94.1.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Campbell MK, Carbone E, Honess-Morreale L, et al. Randomized trial of a tailored nutrition educaiton CD-ROM program for women receiving food assistance. J Nutr Educ Behav. 2004;36:58–66. doi: 10.1016/s1499-4046(06)60134-6. [DOI] [PubMed] [Google Scholar]
- 36.McDonald E, Solomon B, Shields W, et al. Evaluation of kiosk-based tailoring to promote household safety behaviors in an urban pediatric primary care practice. Patient Educ Couns. 2006;58(2):168–81. doi: 10.1016/j.pec.2004.08.015. [DOI] [PubMed] [Google Scholar]
- 37.Petty R, Cacioppo J. Attitudes and Persuasion: Classic and Contemporary Approaches. Dubuque: WC Brown; 1981. [Google Scholar]
- 38.Kreuter M, Bull F, Clark E, et al. Understanding how people process health information: a comparison of tailored and untailored weight loss materials. Health Psychol. 1999;18:487–94. doi: 10.1037//0278-6133.18.5.487. [DOI] [PubMed] [Google Scholar]
- 39.Kreuter M, Jacobsen H, Gielen A, et al. Developing computerized tailored health messages. In: Bensley R, Fisher J, editors. Community Health Education Methods and Strategies: A Practitioner's Guide. Sudbury, MA: Jones and Bartlet Publishers; 2003. pp. 255–89. [Google Scholar]
- 40.Kreuter MW, Wray RJ. Tailored and targeted health communication: strategies for enhancing information relevance. Am J Health Behav. 2003;27(Suppl. 3):S227–32. doi: 10.5993/ajhb.27.1.s3.6. [DOI] [PubMed] [Google Scholar]
- 41.McGuire W. Theoretical foundations of campaigns. In: Rice R, Atkin C, editors. Public Communication Campaigns. Newbury Park: Sage; 1989. pp. 43–65. [Google Scholar]
- 42.Webb M, Simmons N, Brandon T. Tailored interventions for motivating smoking cessation: using placebo-tailoring to examine the influence of personalization and expectancies. Health Psychol. 2005;24:179–88. doi: 10.1037/0278-6133.24.2.179. [DOI] [PubMed] [Google Scholar]
- 43.Demars RY, Neale AV, Adams R, et al. The impact of physicians' brief smoking cessation counseling: a MIRNET study. J Fam Pract. 1990;31:625–9. [PubMed] [Google Scholar]
- 44.Fleming MF, Barry KL, Manwell LB, et al. Brief physical advice for problem alcohol drinkers: a randomized controlled trail in community based primary care practices. JAMA. 1997;277:1039–945. [PubMed] [Google Scholar]
- 45.Kreuter M, Scharff D, Brennan L, et al. Physician recommendations for diet and physical activity: which patients get advised to change? Prev Med. 1997;26:825–33. doi: 10.1006/pmed.1997.0216. [DOI] [PubMed] [Google Scholar]
- 46.US Census. Searchable Database. Available at: http://www.census.gov/main/www/cen2000.html. Accessed: 14 September, 2007. [Google Scholar]
- 47.Centers for Disease Control and Prevention. 2000. Summary Data Quality Report of the Behavioral Risk Factor Surveillance System (BRFSS) Available at: http://www.cdc.gov/brfss/technical_infodata/quality.htm. Accessed: 14 September, 2007. [Google Scholar]