Abstract
Escherichia coli is a zoonotic bacterium that is important to both public health and livestock economics. To date, most studies of zoonotic E. coli transmission have been conducted in developed nations with industrialized agricultural economies. In this study, E. coli bacteria were collected from people and livestock in two communities in rural western Uganda in order to investigate patterns of interspecific bacterial transmission in a developing rural economy characterized by very close human-livestock associations. Six hundred seventy-two E. coli isolates were genotyped using repetitive element-PCR (Rep-PCR) fingerprinting, and genetic distances between populations of bacteria from different hosts and locations were calculated. Genetic distances between human and livestock bacteria were generally very low, indicating high rates of bacterial gene flow among host species. Bacteria from humans and livestock in the same communities were virtually indistinguishable genetically. Data from surveys administered at the time of sample collection showed that people who did not regularly wash their hands before eating harbored bacteria approximately twice as similar genetically to bacteria of their livestock as did people who regularly washed their hands before eating. These results suggest that both rates of human-livestock interactions and patterns of human hygiene affect human-livestock bacterial transmission in this setting. This conclusion has implications not only for human and livestock health in subsistence-based agricultural economies but also for the emergence of zoonotic diseases out of such areas as a result of increasing globalization.
Infectious agents transmitted between humans and their livestock are important to both public health and livestock economics. Taylor et al. (30) previously estimated that 75% of emerging human infectious diseases are zoonotic or have recent zoonotic origins, with livestock serving as important reservoirs of infection. Escherichia coli is of special concern as a livestock-associated bacterial zoonosis (2, 6). E. coli can range in virulence from a benign commensal to highly virulent enteropathogenic forms, such as the O157:H7 serovar (7, 31). Although all forms of the bacterium are zoonotic, few cause clinical disease in infected animals (10) despite the potential of some for high virulence in people (7, 35). Also, E. coli shed by animals can persist in soil, water, manure, and feed, where it can spread to other uninfected animals (15) and to humans (7).
Despite significant advances in our understanding of E. coli transmission in industrialized nations, little is known about the transmission of the bacterium in the developing world. Zoonotic transmission of E. coli and similar pathogens may in fact be very common in rural, subsistence-based agricultural economies. In rural Africa, for example, people traditionally keep livestock in close proximity to the homestead or even inside the domicile. In such situations, humans and livestock come into exceptionally close contact both directly and through cross-contamination of the shared environment. Such contact may increase the risks of pathogen transmission, especially for microbes such as E. coli that are transmitted via the fecal-oral route.
The goal of this study was to investigate patterns of E. coli transmission between humans and their livestock in a developing rural economy characterized by very close human-livestock associations. The study targeted populations of humans and their livestock in western Uganda, where people live in close association with goats, sheep, and cattle. We hypothesized that this close association might lead to high rates of human-livestock E. coli transmission. We further hypothesized that specific human behaviors related to demographics, animal husbandry, and hygiene might affect bacterial transmission rates within this setting. Improving our understanding of human-livestock bacterial transmission in rural western Uganda may help prevent the transmission of livestock pathogens to people in this and similar developing rural economies, where zoonotic bacterial disease is probably underdiagnosed.
MATERIALS AND METHODS
Study areas.
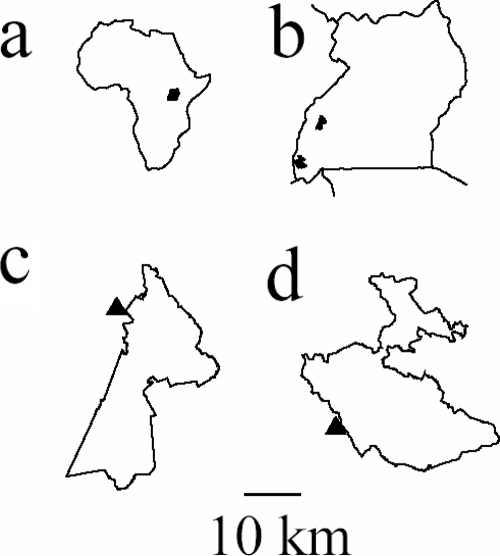
This study was carried out in two communities in rural western Uganda, near Kibale and Bwindi Impenetrable National Parks (Fig. 1). The human population density is high in this region, averaging 220 people per km2 near Bwindi (E. Gubelman, J. Schoorl, and I. Ochoka, unpublished data) and 272 people per km2 near Kibale (25) in the 1990s, with a population growth rate of approximately 2.7% per year (Gubelman et al., unpublished). People in the region are primarily of the Bakiga or Batooro ethnic group and are predominantly subsistence farmers practicing mixed-crop agriculture and rearing cattle, goats, and sheep.
FIG. 1.
Maps showing the locations of study sites. (a) Map of Africa showing the location of Uganda. (b) Map of Uganda showing the locations of Kibale and Bwindi Impenetrable National Parks to the north and south, respectively. (c and d) Maps of Kibale National Park and Bwindi Impenetrable National Park, with triangles representing the locations of the study communities.
These locations were chosen for several reasons. First, subsistence agricultural communities neighboring Ugandan national parks tend to be exceptionally economically impoverished due to crop losses from wildlife (24). This poverty is associated with poor housing, crowding, lack of access to clean water or sanitation, and frequent cohabitation with livestock. Second, despite endemic poverty, these locations lie near popular and economically profitable tourist destinations, which attract a steady influx of international travelers (3). Risks of global transport of zoonoses from such areas are therefore high. Finally, the health of such populations and their zoonotic disease transmission potential have been implicated as important factors determining the long-term sustainability of local wildlife populations, notably great apes (19, 21).
Sampling.
Samples from humans and their livestock were collected between May and August 2005. A total of 26 households from two communities were included in the study. These households represented those that were willing to participate in the study after invitations were made to all households in each community. Each household was sampled only once during the study period. Between three and four livestock per household were sampled. If a household had all species of livestock (cattle, goats, and sheep), we sampled one goat, one sheep, and two cattle. If a household had two or fewer species of livestock, we sampled up to four animals. Because households had eight animals on average, this sampling scheme captured a representative proportion of species and numbers of animals per household. Where possible, livestock representing a range of ages and both sexes were included. Samples were collected directly from the rectum using a sterile glove; otherwise, environmental contamination was avoided by collecting only freshly defecated fecal material that had not contacted the ground.
Human volunteers were given self-contained, sterile bacterial transport systems containing Cary-Blair agar (BD CultureSwab; Becton Dickinson and Company, Franklin, NJ) and were instructed on the proper method of administering a rectal swab. Swabs were collected no later than 24 h after distribution. At the time of swab distribution, a short survey was administered. The survey focused on demographics, tending of animals, personal hygiene, and gastrointestinal symptoms. All questions referred to the 4-week period prior to sampling. The survey was administered in the local languages using trained field assistants from the local communities.
All animal and human protocols were approved by the University of Illinois Institutional Animal Care and Use Committee and Institutional Review Board, respectively, prior to initiation of the study.
Microbiology.
Fecal samples and swabs were streaked onto MacConkey agar plates for the isolation of E. coli, and the plates were incubated at 37°C for 24 h. Up to four putative E. coli colonies were transferred from each sample into tubes containing 0.1 ml tryptic soy agar, which were stored at room temperature up to 4 weeks before transportation to the United States. In the United States, bacteria were reisolated on MacConkey agar, and isolates were confirmed to be E. coli using standard biochemical tests (22). The isolates were then stored in 20% glycerol at −80°C prior to further analysis.
To characterize isolates genetically, repetitive element-PCR (Rep-PCR) was used. Rep-PCR is a molecular fingerprinting technique that targets repetitive sequences dispersed throughout bacterial chromosomes and that is useful for inferring relationships among bacterial isolates (33). Procedures for the Rep-PCR protocols used were described in detail elsewhere previously (12). Fingerprints were stored in a database in the computer program BioNumerics, version 4.0 (Applied Maths, Austin, TX), and relatedness among isolates was assessed using analytical parameters that anchor Rep-PCR fingerprints to the “gold standard” of multilocus sequence typing according to previously published methods (12). Specifically, parameters were optimized for identifying bands on electrophoretic gels (minimum profiling of 0.0, minimum area of 1.8, and shoulder sensitivity of 0.0) and for calculating genetic distances from banding patterns (optimization of 1.0, tolerance of 0.52, and the Dice algorithm) (see reference 12 for details).
Population genetic analyses available in the computer program Arlequin, version 3.0 (8), were performed to measure genetic distances among bacterial populations. Specifically, analysis of molecular variance was used to apportion genetic variation among different populations of E. coli and thereby to examine the bacterial population genetic substructure. Arlequin was used to calculate pairwise FST values among bacterial populations, which can be interpreted as short-term genetic distances (26, 28). To measure the effects of demographic and behavioral risk factors on genetic similarity between bacteria from individual humans and bacteria from their livestock, we used nonparametric statistical tests, since neither predictors nor outcome variables were normally distributed. Specifically, we calculated Spearman's rank order correlation coefficients for interval level predictor variables, and we conducted Mann-Whitney U tests for categorical predictor variables. The outcome variable in all cases was genetic distance between bacteria from humans and bacteria from livestock, measured as FST. These analyses were run using the computer program SPSS, version 14.0 (SPSS, Chicago, IL). To examine the effects of household and host species on bacterial genetic distance, Mantel's and rowwise matrix correlation tests (5, 23) were conducted using MatMan, version 1.1 (Noldus Information Technology, Wageningen, The Netherlands), with binary matrices (0/1) used to represent household or species identity and matrices of FST values used to represent genetic distances among bacterial isolates from different human or livestock individuals. For matrix correlation tests, statistical significance was assessed using 1,000 random permutations of the original matrices.
RESULTS
Six hundred seventy-two isolates were collected from 48 livestock and 35 humans from the community near Bwindi Impenetrable National Park and 56 livestock and 73 humans from the community near Kibale National Park (Table 1). Samples represented approximately 13% and 23%, respectively, of households in each location. The median age of humans sampled was 15 years near Bwindi and 12 years near Kibale, and samples consisted of 41.2% males and 50.7% males in each location, respectively, with an age range of 0.2 to 70 years. Humans sampled were engaged in a diversity of occupations, including subsistence farmers, students, carpenters, pit sawyers, tea factory workers, porters (for tourists visiting the mountain gorillas in Bwindi), and assistants for chimpanzee research projects near Kibale.
TABLE 1.
E. coli isolates collected from humans and livestock from communities in rural western Uganda
| Community | Species sampled | No. of individuals sampled | No. of isolates collected and analyzed | No. of genetically distinct isolatesa | Mean no. of isolates per individual (SEM) | Mean no. of genetically distinct isolates per individual (SEM) |
|---|---|---|---|---|---|---|
| Bwindi | Humans | 35 | 87 | 61 | 2.49 (0.18) | 1.74 (0.132) |
| Cattle | 5 | 13 | 7 | 2.6 (0.6) | 1.4 (0.245) | |
| Goats | 34 | 105 | 50 | 3.09 (0.16) | 1.47 (0.114) | |
| Sheep | 9 | 19 | 13 | 2.38 (0.324) | 1.63 (0.324) | |
| Kibale | Humans | 73 | 252 | 151 | 3.45 (0.103) | 2.07 (0.111) |
| Goats | 48 | 168 | 98 | 3.5 (0.103) | 2.04 (0.13) | |
| Sheep | 8 | 28 | 15 | 3.5 (0.267) | 1.88 (0.35) |
Characteristic Rep-PCR banding patterns were used to define unique genotypes. Genotypes were considered to be unique if they differed by one or more bands on the fingerprint pattern.
Pairwise FST values, which can vary from 0 to 1, are given for populations of bacteria from humans and livestock near Bwindi and Kibale in Table 2. In both locations, humans and livestock harbored bacteria that were very closely related (maximum FST of 0.053). Bacteria from humans near Bwindi were most closely related to bacteria from livestock in that same community. Likewise, bacteria from humans near Kibale were most closely related to bacteria from livestock in that same community. Notably, for both locations, humans harbored bacteria even more similar genetically to bacteria from livestock in the same location than to bacteria from humans in the other location, and the same trend held for livestock.
TABLE 2.
Pairwise interpopulation FST values for E. coli bacteria from humans and livestock in two communities in rural western Uganda
| Populationb |
FST (SE)a
|
||
|---|---|---|---|
| Livestock in Bwindi | Humans in Bwindi | Livestock in Kibale | |
| Livestock in Bwindi (n = 137) | |||
| Humans in Bwindi (n = 87) | 0.027 (0.004) | ||
| Livestock in Kibale (n = 196) | 0.027 (0.004) | 0.050 (0.008) | |
| 4Humans in Kibale (n = 252) | 0.040 (0.006) | 0.053 (0.008) | 0.011 (0.002) |
Standard errors (in parentheses) were estimated using a bootstrap analysis with 1,000 replicates calculated with the computer program Arlequin (8). Each of the six FST values shown is statistically significantly different from the null expectation of no genetic difference between the populations (P < 0.01).
Sample sizes indicate numbers of bacterial isolates per population.
Analysis of molecular variance was used to quantify the apportionment of bacterial genetic diversity within and among individuals, populations, and species (Table 3). Most bacterial genetic diversity was contained within individual humans and livestock (65.3% and 66.7%, respectively). Differences among individuals accounted for an approximately equal proportion of bacterial genetic diversity in humans (29.7%) as in livestock (31.1%). Differences among locations accounted for only very minor proportions of bacterial genetic diversity (approximately 5.0% in humans and 2.9% in livestock). Differences among species accounted for an even smaller proportion of bacterial genetic diversity (less than 1%), again implying high bacterial “gene flow” between humans and livestock.
TABLE 3.
Hierarchical analyses of molecular of variance for E. coli isolates collected from humans and livestock in two communities in two regions of rural western Uganda
| Variance component | Observed partition
|
Φ Statistic | P valueb | |
|---|---|---|---|---|
| Variance | % of Total | |||
| Humans (n = 339 isolates from 108 individuals at two locations) | ||||
| Between locations | 0.402 | 04.99 | ΦCT = 0.050 | <0.0001 |
| Among individuals within locations | 2.391 | 29.74 | ΦSC = 0.313 | <0.0001 |
| Within individuals | 5.247 | 65.27 | ΦST = 0.347 | <0.0001 |
| Livestock (n = 333 isolates from 104 individuals at two locations) | ||||
| Between locations | 0.172 | 02.81 | ΦCT = 0.022 | <0.0001 |
| Among individuals within locations | 2.448 | 31.08 | ΦSC = 0.318 | <0.0001 |
| Within individuals | 5.257 | 66.74 | ΦST = 0.333 | <0.0001 |
| Humans and livestock (n = 672 isolates from 212 individuals at two locations) | ||||
| Between species | 0.063 | 00.81 | ΦCT = 0.008 | <0.0001 |
| Among individuals within species | 2.537 | 32.30 | ΦSC = 0.326 | <0.0001 |
| Within individuals | 5.252 | 66.89 | ΦST = 0.331 | <0.0001 |
a Data consisted of bacterial genotypes represented as a series of binary variables indicating the presence or absence of bands at each of 103 band positions identified and scored using the “bandmatch” procedure of the computer program BioNumerics, version 4.0 (Applied Maths, Inc.), according to previously reported analytical methods (12).
Probability of having a more extreme variance component and Φ statistic than the observed value by chance alone; probabilities were calculated from 16,000 random permutations of the data using Arlequin. ΦCT was tested with random permutations of whole populations across locations, ΦSC was tested with random permutations of individuals across populations but within the same location, and ΦST was tested with random permutations of individuals across populations without regard to either their original population or location (9).
Mantel's tests of matrix correlation indicated that in both locations (Bwindi and Kibale), humans from the same household tended to share genetically similar bacteria (r value of 0.269 and P value of <0.001, and r value of 0.188 and P value of <0.001, respectively). In the community near Kibale, livestock from the same household also tended to share similar bacteria (r = 0.132; P < 0.001). This trend was marginally nonsignificant for livestock in the community near Bwindi (r = 0.054; P = 0.097), perhaps due to low sample sizes. Rowwise matrix correlation analyses demonstrated that humans and livestock from the same households near Bwindi tended to harbor genetically similar bacteria (Zr statistic = 39; P = 0.039); however, this same trend was not apparent near Kibale (Zr statistic = −145.9; P = 0.074).
Nonparametric statistical analyses were used to examine the effects of age, sex, tending livestock, experiencing gastrointestinal symptoms (which was excluded for Bwindi because no one reported symptoms), fetching water from an open water source, and washing hands before eating (which was excluded for Kibale because only one person reported not washing hands before eating) on human-livestock bacterial genetic similarity. In households near Kibale, none of these predictors was significantly associated with FST (P ≥ 0.06 in all cases). In households near Bwindi, washing hands before eating was significantly associated with increased human-livestock bacterial genetic distance (Z = −2.317; P = 0.010 [Mann-Whitney U test]); people who didn't wash their hands before eating harbored bacteria approximately twice as similar genetically to bacteria of their livestock as did people who washed their hands prior to eating (mean FST of 0.1213 versus 0.2263, respectively).
DISCUSSION
This study provides evidence that close contact between people and livestock can lead to high rates of E. coli transmission between species. In general, FST values among all populations of bacteria sampled were very low, indicating little genetic subdivisioning among E. coli samples from different species in rural western Uganda, even over distances of several hundred kilometers. Bacteria from humans and livestock in the same community were virtually indistinguishable genetically. In fact, human-livestock bacterial genetic similarity within a location was higher even than human-human or livestock-livestock bacterial genetic similarity between locations. In both locations, the household had a significant effect on the similarity of bacteria among humans, with people from the same household tending to share genetically similar bacteria. The same trend was observed for livestock near Kibale, and a similar significant “household effect” was observed for human-livestock bacterial genetic similarity near Bwindi.
In rural sub-Saharan Africa, as in much of the developing world, people and their livestock live in exceptionally close quarters. Housing of animals near a homestead or within the domicile increases opportunities for contamination of the shared environment with enteric bacteria. When not in the homestead, animals are tethered and/or grazed in locations where their owners perform farm work and harvest food. Water for domestic use is frequently collected from wells that are not protected from contamination. Documented modes of enteric bacterial transmission include direct ingestion; transmission via other animals (including insects); and contaminated water, air, and fomites (17). Studies have shown that fecally excreted E. coli can contaminate the farm environment as well as hides of animals (4, 20). Humans can become infected directly or indirectly via the fecal-oral route through food (1), the environment (29), or direct contact with farm animals and/or feces (16).
Although the exact mode(s) of human-livestock bacterial transmission in our study areas remains uncertain, our statistical analyses suggest that both behavioral and demographic factors affect human-livestock bacterial transmission rates. Humans in both study locations tended to share genetically similar E. coli strains with members of the same household, and the same trend held true for livestock in households near Kibale. In households near Bwindi, people and livestock from the same household tended to share genetically similar bacteria, and regular hand washing in that location apparently decreased human-livestock bacterial transmission. The World Health Organization reported that poor sanitation, lack of access to clean water, and inadequate personal hygiene are responsible for an estimated 90% of childhood diarrheas (34). It has also been reported that promotion of hand washing reduces diarrhea incidence by an average of 33% (18). Our results extend these findings to the specific case of zoonotic E. coli in rural sub-Saharan Africa, and they reinforce the notion that both living conditions and hygiene significantly impact transmission rates of diarrheal pathogens.
This study also builds on our previously reported investigations of bacterial transmission between humans and wildlife in western Uganda (11, 13, 27). Goldberg et al. (11) examined chimpanzees in Uganda and showed that the level of bacterial gene flow between chimpanzees and humans employed in chimpanzee research and tourism was high. Goldberg et al. (13) further demonstrated that human behavior and primate ecology affect rates of bacterial transmission among people, livestock, and monkeys in western Uganda. Data from the present study add to this growing evidence that both ecology and human behavior can affect rates of gastrointestinal bacterial transmission among people, livestock, and wildlife.
Our results should be interpreted cautiously with respect to generalized patterns of enteric bacterial transmission. In particular, results might have been different for pathogens more virulent than E. coli. The bacteria sampled for the present study were nonpathogenic commensals (none of the study participants reported symptoms consistent with highly enteropathogenic E. coli, such as O157:H7). Higher pathogen virulence might lead to either higher or lower rates of transmission, depending on the effects of clinical disease on behavior and bacterial shedding into the environment. In this light, it is important that neither the physical environment nor other animals that might play a role in bacterial transmission in this setting (e.g., chickens, dogs, and rodents) were sampled. Mammalian livestock were chosen because of the documented role of these animals in zoonotic E. coli transmission; however, other species and contaminated features of the physical environmental would almost certainly play important roles and merit further investigation. Furthermore, the analytical methods used did not allow us to determine the direction of transmission among species. Although animal fecal contamination of homesteads makes zoonotic transmission likely, many opportunities for anthroponotic transmission also exist in this system. Finally, the study was geographically limited to rural western Uganda, and comparative populations of humans or livestock from other locations were not included. Future investigations incorporating other study populations would help place our results in a broader geographical context. The findings of this study should therefore be interpreted as pertaining to generalized patterns of bidirectional, interspecific bacterial transmission in a specific population that has not previously been studied in this regard.
Despite these caveats, the patterns of genetic similarity documented in this study suggest that rates of E. coli transmission between humans and livestock are high in rural southwestern Uganda. We predict that these patterns will hold true for other similar developing economies, where close human-livestock interactions characterize daily life, and for other pathogens transmitted via similar modes. Finally, it should be noted that Uganda has a high prevalence of human immunodeficiency virus/AIDS, which renders the human population immunocompromised and therefore susceptible to opportunistic infections (32). This situation, in addition to increased globalization and a steady flow of international tourists visiting the national parks near our study communities, raises concerns about the potential for zoonoses of livestock origin to become established and to spread. Only by understanding the ecological and behavioral factors that influence human-animal pathogen transmission in such settings can rational interventions to safeguard animal and human health be designed.
Acknowledgments
We gratefully acknowledge the Uganda National Council for Science and Technology and the local council governments of the local communities for granting us permission to conduct this research. We also thank F. Nizeyimana, D. Maniragaba, S. Mbonigaba, D. Mabesha, and J. Byarugaba, for providing invaluable assistance in the field and E. Estoff, K. Inendino, J. Salzer, E. Wheeler, K. Knuffman, and S. Hampson for providing assistance in the laboratory.
This material is based upon work supported by a Wildlife Conservation Society research fellowship (to I.B.R.) and by the Morris Animal Foundation under award no. D04ZO-67 and D07ZO-024.
Footnotes
Published ahead of print on 6 August 2008.
REFERENCES
- 1.Bell, B. P., M. Goldoft, P. A. Griffin, M. A. Davis, D. C. Gordon, P. I. Tarr, C. A. Bartleson, J. H. Lewis, et al. 1994. A multistate outbreak of E. coli O157:H7-associated bloody diarrhea and hemolytic uremic syndrome from hamburgers. JAMA 2721349-1353. [PubMed] [Google Scholar]
- 2.Beutin, L. 2006. Emerging enterohaemorrhagic Escherichia coli, causes and effects of the rise of a human pathogen. J. Vet. Med. B Infect. Dis. Vet. Public Health 53299-388. [DOI] [PubMed] [Google Scholar]
- 3.Butynski, T. M., and J. Kalina. 1998. Gorilla tourism: a critical look, p. 280-300. In E. J. Milner-Gulland, and R. Mace (ed.), Conservation of biological resources. Blackwell Science Ltd., Oxford, United Kingdom.
- 4.Conedera, G., P. A. Chapman, S. Marangon, E. Tisato, P. Dalvit, and A. Zuin. 2001. A field survey of Escherichia coli O157 ecology on a cattle farm in Italy. Int. J. Food Microbiol. 6685-93. [DOI] [PubMed] [Google Scholar]
- 5.de Vries, H. 1993. The rowwise correlation between two proximity matrices and the partial rowwise correlation. Psychometrika 5853-69. [Google Scholar]
- 6.Donnenberg, M. 2002. Escherichia coli: virulence mechanisms of a versatile pathogen. Academic Press, San Diego, CA.
- 7.dos Santos, L. F., E. M. Gonçalves, T. M. I. Vaz, K. Irino, and B. E. C. Guth. 2007. Distinct pathotypes of O113 Escherichia coli strains isolated from humans and animals in Brazil. J. Clin. Microbiol. 452028-2030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Excoffier, L., G. Laval, and S. Schnieder. 2005. Arlequin version 3.0: an integrated software package for population genetics data analysis. Evol. Bioinform. Online 147-50. [PMC free article] [PubMed] [Google Scholar]
- 9.Excoffier, L., P. E. Smouse, and J. M. Quattro. 1992. Analysis of molecular variance inferred from metric distance among DNA haplotypes: applications to human mitochondrial DNA restriction data. Genetics 131479-491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Galland, J. C., D. R. Hyatt, S. S. Crupper, and D. W. Acheson. 2001. Prevalence, antibiotic susceptibility, and diversity of Escherichia coli O157:H7 isolates from a longitudinal study of beef cattle feedlots. Appl. Environ. Microbiol. 671619-1627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goldberg, T. L., T. R. Gillespie, I. B. Rwego, E. Wheeler, E. L. Estoff, and C. A. Chapman. 2007. Patterns of gastrointestinal bacterial exchange between chimpanzees and humans involved in research and tourism in western Uganda. Biol. Conserv. 135511-517. [Google Scholar]
- 12.Goldberg, T. L., T. R. Gillespie, and R. S. Singer. 2006. Optimization of analytical parameters for inferring relationships among Escherichia coli isolates from repetitive-element PCR by maximizing correspondence with multilocus sequence typing data. Appl. Environ. Microbiol. 726049-6052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goldberg, T. L., T. R. Gillespie, I. B. Rwego, E. E. Estoff, and C. A. Chapman. 2008. Forest fragmentation as cause of bacterial transmission among primates, humans, and livestock, Uganda. Emerg. Infect. Dis. 141375-1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reference deleted.
- 15.Hancock, D. D., T. E. Besser, and D. H. Rice. 1998. Ecology of Escherichia coli O157:H7 in cattle and impact of management practices, p. 85-91. In J. B. Kaper and A. D. O'Brien (ed.), Escherichia coli O157:H7 and other Shiga toxin-producing E. coli strains. ASM Press, Washington, DC.
- 16.Heuvelink, A. E., C. van Heerwaarden, J. T. Zwartkruis-Nahuis, R. van Oosterom, K. Edink, Y. T. van Duynhoven, and E. de Boer. 2002. Escherichia coli O157 infection associated with a petting zoo. Epidemiol. Infect. 129295-302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hutchison, M. L., L. D. Walters, A. Moore, and S. M. Avery. 2005. Declines of zoonotic agents in liquid livestock wastes stored in batches on-farm. J. Appl. Microbiol. 9958-65. [DOI] [PubMed] [Google Scholar]
- 18.Huttly, S. R., S. S. Morris, and V. Pisani. 1997. Prevention of diarrhoea in young children in developing countries. Bull. W. H. O. 75163-174. [PMC free article] [PubMed] [Google Scholar]
- 19.Köndgen, S., H. Kuhl, P. K. N′Goran, P. D. Walsh, S. Schenk, N. Ernst, R. Biek, P. Formenty, K. Mätz-Rensing, B. Schweiger, S. Junglen, H. Ellerbrok, A. Nitsche, T. Briese, W. I. Lipkin, G. Pauli, C. Boesch, and F. H. Leendertz. 2008. Pandemic human viruses cause decline of endangered great apes. Curr. Biol. 181-5. [DOI] [PubMed] [Google Scholar]
- 20.Lahti, E., O. Ruoho, L. Rantala, M. L. Hanninen, and T. Honkanen-Buzalski. 2003. Longitudinal study of Escherichia coli O157 in a cattle finishing unit. Appl. Environ. Microbiol. 69554-561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Leendertz, H. L., G. Pauli, K. Maetz-Rensing, W. Boardman, C. Nunn, H. Ellerbrok, S. A. Jensen, S. Junglen, and C. Boesch. 2006. Pathogens as drivers of population declines: the importance of systematic monitoring in great apes and other threatened mammals. Biol. Conserv. 131325-337. [Google Scholar]
- 22.MacFaddin, J. F. 1980. Enterobacteriaceae and other intestinal bacteria, p. 439-464. In J. F. MacFaddin (ed.), Biochemical tests for identification of medical bacteria. Williams & Wilkins, Baltimore, MD.
- 23.Mantel, N. 1967. The detection of disease clustering and a generalized regression approach. Cancer Res. 27209-220. [PubMed] [Google Scholar]
- 24.Naughton-Treves, L. 1997. Farming the forest edge: vulnerable places and people around Kibale National Park, Uganda. Geogr. Rev. 8727-46. [Google Scholar]
- 25.Naughton-Treves, L., A. Treves, C. Chapman, and R. Wrangham. 1998. Temporal patterns of crop-raiding by primates: linking food availability in croplands and adjacent forest. J. Appl. Ecol. 35596-606. [Google Scholar]
- 26.Reynolds, J., B. S. Weir, and C. C. Cockerham. 1983. Estimation of the coancestry coefficient: basis for a short-term genetic distance. Genetics 105767-779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rwego, I. B., G. Isabirye-Basuta, T. R. Gillespie, and T. Goldberg. Gastrointestinal bacterial transmission among humans, mountain gorillas, and domestic livestock in Bwindi Impenetrable National Park, Uganda. Conserv. Biol., in press. [DOI] [PubMed]
- 28.Slatkin, M. 1995. A measure of population subdivision based on microsatellite allele frequencies. Genetics 139457-462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Strachan, N. J. C., D. R. Fenlon, and I. D. Ogden. 2001. Modelling the vector pathway and infection of humans in an environmental outbreak of Escherichia coli O157. FEMS Microbiol. Lett. 20369-73. [DOI] [PubMed] [Google Scholar]
- 30.Taylor, L. H., S. M. Latham, and M. E. Woolhouse. 2001. Risk factors for human disease emergence. Philos. Trans. R. Soc. Lond. B Biol. Sci. 356983-989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Trabulsi, L., R. Keller, and T. Tardelli-Gomes. 2002. Typical and atypical enteropathogenic Escherichia coli. Emerg. Infect. Dis. 8508-513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tumwine, J. K., A. Kekitiinwa, S. Bakeera-Kitaka, G. Ndeezi, R. Downing, X. Feng, D. E. Akiyoshi, and S. Tzipori. 2005. Cryptosporidiosis and microsporidiosis in Ugandan children with persistent diarrhea with and without concurrent infection with the human immunodeficiency virus. Am. J. Trop. Med. Hyg. 73921-925. [PubMed] [Google Scholar]
- 33.Versalovic, J., T. Koeuth, and J. R. Lupski. 1991. Distribution of repetitive DNA sequences in eubacteria and application to fingerprinting of bacterial genomes. Nucleic Acids Res. 196823-6831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.WHO. 1997. Health and environment in sustainable development five years after the health summit. WHO/EHG/97.8. WHO, Geneva, Switzerland.
- 35.Wickham, M. E., C. Lupp, M. Mascarenhas, A. Vázquez, B. K. Coombes, N. F. Brown, B. A. Coburn, W. Deng, J. L. Puente, M. A. Karmali, and B. B. Finlay. 2006. Bacterial genetic determinants of non-O157 STEC outbreaks and hemolytic-uremic syndrome after infection. J. Infect. Dis. 194819-827. [DOI] [PubMed] [Google Scholar]