Abstract
Reactive Attachment Disorder (RAD) is a childhood disorder characterized by extremely inappropriate social relating across a variety of interactions that must be present by age 5. Although children diagnosed with RAD appear to demonstrate significantly more behavioral problems and psychosocial difficulties than children without RAD, there have been few examinations of empirically informed treatments for this disorder. One avenue that may be particularly promising is the use of treatments that have been successfully used to decrease similar problematic behaviors in children. The present case study outlines the use of behavior management training (BMT) in the treatment of a 7-year-old female child with RAD. Given the marked reduction in problematic behaviors exhibited by this child as a result of a typical course of BMT, it is recommended that randomized clinical trials be conducted to test the efficacy of BMT for RAD.
Keywords: reactive attachment disorder, maltreatment, therapy, case study
Reactive Attachment Disorder (RAD) is a childhood disorder characterized by extremely inappropriate social relating across a variety of social interactions that must be present before the age of 5 (American Psychiatric Association, 2000). Observed disturbances in social interactions must be attributable to pathogenic care, defined as the failure to meet the basic emotional and/or physical needs of the child and/or an absence of a stable caregiver to which the child could form an attachment. According to the Diagnostic and Statistical Manual of Mental Disorders (4th ed.; DSM-IV; American Psychiatric Association, 1994), RAD is characterized by two subtypes: inhibited and disinhibited. In the inhibited type, children tend to be emotionally withdrawn and unlikely to seek comfort or attention, even from familiar adults. In the disinhibited type, children are apt to be overly assertive in their social interactions, demanding attention or affection from any adult in their proximity (including strangers). However, surprisingly little work has examined the utility of treatments for this disorder. The aim of the current report is to use data from the successful treatment of one child with RAD to spur researchers to conduct research to identify effective treatments for this disorder.
Children diagnosed with RAD appear to demonstrate significantly more behavioral problems and psychosocial problems than children without RAD. Although RAD has received little empirical attention, research has demonstrated that children with RAD score significantly higher than children without RAD on the following dimensions: general behavioral problems, social problems, withdrawal, somatic complaints, anxiety/depression, thought problems, attention problems, delinquent behavior, aggressive behavior, lack of empathy, and excessive self-monitoring (Kay Hall & Geher, 2003), and RAD symptoms are associated with higher rates of hyperactivity and other behavioral and emotional problems (Millward, Kennedy, Towlson, & Minnis, 2006). Clinical case studies suggest that RAD is also associated with deficits in social relatedness, delayed language and motor skill development, failure to acquire age-appropriate self-care skills, problematic eating behaviors (e.g., gorging), emotional lability, problems with attention and concentration, impulsivity, and oppositional behaviors (Hinshaw-Fusilier, Boris, & Zeanah, 1999; Richters & Volkmar, 1994). Furthermore, children experiencing pathogenic care (a symptom of RAD) exhibit numerous mal-adaptive behaviors including hypersexuality, impulsivity, hyperactivity, developmental delays, language impairments, suicidal and homicidal ideation, hoarding/gorging food, as well as conduct problems such as stealing, lying, destroying property, fire setting, and cruelty to animals (Parker & Forrest, 1993; Reber, 1996).
Despite the behavioral and emotional problems linked with RAD, epidemiological data regarding RAD prevalence rates are lacking. The majority of work investigating rates of RAD has examined whether children in foster care are at particular risk for RAD symptomatology. Emerging data suggest that these children do, in fact, demonstrate greater rates of RAD symptoms than children not in the foster care system (Millward et al., 2006). Furthermore, approximately 35% to 45% of maltreated children in foster care appear to have clinically meaningful RAD symptoms (Boris, Zeanah, Larrieu, Scheeringa, & Heller, 1998; Zeanah et al., 2004). As suggested by the disorder's name, RAD is believed to result from disrupted attachments with primary caregivers that result from pathogenic care. According to attachment theory (Bowlby, 1978), a child forms an attachment to a primary caregiver beginning in infancy as a function of the child's need for protection, nurturance, and comfort. Problematic attachments can serve as risk factors for later problems such as externalizing problem behaviors (van Ijzendoorn, Schuengel, & Bakermans-Kranenburg, 1999). Given the high rates of RAD symptoms among children who experienced suboptimal care (e.g., some children in foster care), treatments aimed at ameliorating RAD symptomatology and associated impairment could reduce suffering among a good many children.
Existing treatments for RAD tend to be attachment-based therapies. Perhaps the most publicized of these treatments is holding therapy, also known as rebirthing or rage reduction therapy. As described by Hanson and Spratt (2000), these therapies are based on the premise that the behavioral features of RAD are the consequence of suppressed rage experienced by children who experienced pathogenic care. Thus, the therapies comprised prolonged restraint of the child and exposing the child to noxious stimuli (e.g., tickling, poking, tapping, yelling) until the child's attempts to escape the noxious stimuli have ceased. At that point, the child is given to the caregiver for attachment. Healthy attachment is thought to be able to occur at that point as the child's rage has been released throughout the restraining and noxious stimuli portion of treatment.
Little research has investigated whether holding therapies are effective for the treatment of RAD. In fact, we know of only one published trial of holding therapy for children with attachment difficulties (Myeroff, Mertlich, & Gross, 1999). The efficacy of holding therapy was examined in a sample of children whose foster parents contacted an Attachment Clinic. Eligible children demonstrated both aggressive behaviors and difficulty attaching to foster parents. Participants in the holding therapy condition consisted of families willing to engage in holding therapy. The comparison group consisted of families who chose not to participate in the holding therapy for reasons such as time and/or financial constraints and lack of interest in treatment. Children who received holding therapy demonstrated a significant decrease in aggressive and delinquent behaviors relative to children that did not participate in holding therapy. However, there are several limitations to this study that make interpretations difficult. Perhaps the most notable limitation is that participants were not randomly assigned to treatment conditions. This is problematic, as there could be very meaningful differences between those families willing and able to participate in holding therapy relative to those families who did not. For instance, given that the comparison group comprised at least some caregivers who did not have the time or financial resources for treatment, those caregivers in the active treatment may have had more time to spend with children outside of treatment. Spending time with children outside of treatment may have led to increased attachment to caregivers and at least partially accounted for observed gains.
In addition to the lack of empirical support for attachment therapies such as holding and rebirthing therapies for RAD, numerous mental health professionals and professional societies warn against the use of these therapies (e.g., Barth, Crea, John, Thoburn, & Quinton, 2005; Boris & Zeanah, 2005; Chaffin et al., 2006; Haugaard & Hazan, 2004; Mercer, 2001; Speltz, 2002). Use of holding-type therapies is cautioned for several reasons. For instance, physical injury and even death have occurred for some children undergoing holding therapies (see Chaffin et al., 2006). Furthermore, it is questionable as to whether releasing rage is actually beneficial. In fact, empirical evidence indicates that venting anger may actually increase anger and aggression (Bushman, 2002). Another criticism of holding therapies is that because children with RAD tend to have severe abuse or neglect histories, holding therapies could perpetuate the trauma that these children have experienced (Hanson & Spratt, 2000). Criticisms such as these, combined with the lack of empirical work supporting the effectiveness of holding therapies, suggest the need for alternative treatments for RAD.
Although holding therapies are the most popular and controversial of the attachment therapies, other attachment-based therapeutic techniques have been developed for children with attachment difficulties (e.g., play therapy, art therapy). However, to date, we know of no randomized clinical trials (RCTs) designed to evaluate the utility of a treatment specifically targeting RAD. In fact, the only RCT of which we are aware in this area was designed to evaluate the utility of an intervention aimed at preventing long-term behavior problems in foster children, a group at particular risk for RAD symptomatology (Boris et al., 1998; Millward et al., 2006; Zeanah et al., 2004). Attachment and Biobehavioral Catch-Up (ABC; Dozier et al., 2006), a 10-session manualized intervention for foster parents of young children, targets behavioral, emotional, and physiological dysregulation that can occur as a result of maltreatment. At 1-month follow-up, toddlers and infants in the ABC group exhibited lower cortisol levels and fewer parent-reported behavior problems among toddlers (but not infants) relative to participants in the education control group. Though promising, it is as yet unclear that this intervention would be effective with infants and children with RAD given this study did not assess for RAD symptomatology. In fact, although the infants and children in this study were considered to be at risk for developing disruptions in regulatory behaviors and relationship formation, they were not reported to actually have any psychological diagnoses or problematic behaviors (e.g., opposition, defiance, or aggression). Additionally, this intervention did not directly address aggressive and angry behaviors (common correlates of RAD), thereby further limiting the generalizablity of these findings to the treatment of RAD. Finally, given that the children in this study ranged in age from 20 to 60 months, there remain no known empirically supported treatments for older children and adolescents with RAD.
In the absence of empirically supported treatments for RAD, investigating the utility of treatments that have been documented to be effective for the treatment of disorders with similar symptoms and correlates (and to cause no harm) may be a reasonable approach. Several treatments have been found to be efficacious in the reduction of many behavioral problems. For example, parent training programs such as Parent-Child Interaction Therapy (PCIT; Eyberg & Boggs, 1998), Behavior Management Training (BMT; Barkley, 1997), and the Incredible Years (Webster-Stratton & Reid, 2003) are empirically based treatments that primarily focus on helping parents improve the quality of interactions with their child, communicate behavioral expectations clearly, and provide appropriate consequences for child behavior. BMT appeared particularly relevant for the treatment of the child presented in the present case study given the treatment's age appropriateness (e.g., PCIT targets preschool-age children) and utility with individual clients (e.g., the Incredible Years is generally group based).
BMT (Barkley, 1997) consists of a 10-session manualized treatment program for caregivers of school-age children with behavioral problems such as defiance, aggression, and problems with attention and concentration (i.e., problems commonly seen in RAD). BMT is designed to provide caregivers with psychoeducation about childhood misbehavior as well as to instruct caregivers on parenting skills they can use to increase compliance, decrease disruptive behavior, establish proper disciplinary systems, and improve school behavior with a home-based reward system. BMT has been found to be efficacious in reducing problematic behaviors in children between 6 and 11 years of age (Anastopoulos, Shelton, DuPaul, & Guevremont, 1993). Also, BMT is associated with lower premature termination rates among caregivers relative to other caregiver-training therapies (e.g., problem-solving communication training) aimed at reducing problem behaviors in children (Barkley, Edwards, Laneri, Fletcher, & Metevia, 2001). Furthermore, no reports of harmful outcomes for children participating in BMT have been documented. Given that children with RAD often exhibit oppositional and aggressive behaviors (Kay Hall & Geher, 2003; Millward et al., 2006), it follows that BMT may prove to be an effective treatment for RAD. In addition, BMT comprises components identified in a recent meta-analysis to be associated with better outcomes among attachment-based therapies, including being time limited, goal directed, behaviorally oriented, and concerned with parental participation (Bakermans-Kraneneburg, van Ijzendoorn, & Juffer, 2003). Preliminary findings from a case study of a patient receiving treatment for RAD are provided to illustrate the potential utility of this treatment for the reduction of RAD symptoms and associated impairment.
Method
Patient Description
The patient was a 7-year-old Caucasian girl whose caregivers (her grandparents) sought treatment at our university-affiliated outpatient clinic for the child's behavioral problems. The grandparents reported that since moving in with them earlier that year, the child exhibited several problematic behaviors. For example, they described that she was often noncompliant and seemed to enjoy “annoying others” both at home and at school. Additionally, she engaged in socially inappropriate behaviors such as strongly and painfully hugging others (children as well as adults across a variety of settings), refusal to adequately clean herself after using the toilet, “eating like a dog” (i.e., with her face to the plate without the assistance of silverware), and vaginal and anal self-touching. The child experienced recurrent urinary tract infections (UTIs), which the grandparents attributed to her vaginal and anal self-touching. The child was reportedly often defiant with her school teachers, and school authorities threatened expulsion if the hurtful hugging did not cease. The grandparents also indicated that the child did not play with other children on the playground at school and had no age-appropriate friends at home (she had one friend in the neighborhood who was significantly younger). The grandparents presented for treatment to improve the child's social skills and decrease her engagement in socially inappropriate and defiant behaviors.
The grandparents indicated that they had very little contact with their granddaughter before they adopted her. They reported that the child lived in another state with both biological parents when she was born. However, within her first year, her parents separated and her father obtained custody of the child. The mother was committed to a psychiatric hospital shortly thereafter following a suicide attempt. The grandparents reported that the child's father neglected the child emotionally and physically. To illustrate, they were informed that the child was responsible for feeding herself before 2 years of age and was not taught to clean herself after using the toilet. A history of sexual abuse was also suspected but unconfirmed. The grandparents applied for custody as soon as they learned the child was living with a foster family upon her father's death.
Pretreatment Assessment
Clinical interview
Developmental and psychosocial history regarding the child was obtained in an intake interview with her grandparents, who served as her legal guardians. The clinical interview consisted of two instruments: (a) The Mini-International Neuro-psychiatric Interview for Children and Adolescents (MINI-Kid; Sheehan et al., 1998) is a short, structured interview designed to assess symptoms of several Axis I disorders as listed in the DSM-IV and the International Statistical Classification of Diseases and Related Health Problems (World Health Organization, 1990). The MINI-Kid has been found to demonstrate good reliability and diagnostic sensitivity (Judit et al., 2004). (b) The Clinical Interview–Parent Report Form (Barkley, 1997) was used to gather information regarding the child's educational, medical, psychiatric, family, and social history. In addition, the therapist rated the severity of the child's overall psychosocial functioning using the Clinical Global Impressions (CGI; Guy, 1976), a 7-point Likert-type scale ranging from normal (1) to among the most extremely ill patients (7).
Caregiver self-report measures
At intake, the grandparents completed a battery of measures regarding the child's behavioral and emotional functioning. The Conners' Parent Rating Scales–Revised (CPRS-R; Conners, 1997) comprises items that specifically assess attention deficit hyperactivity disorder (ADHD) and related behavior problems.
Ongoing and Posttreatment Assessments
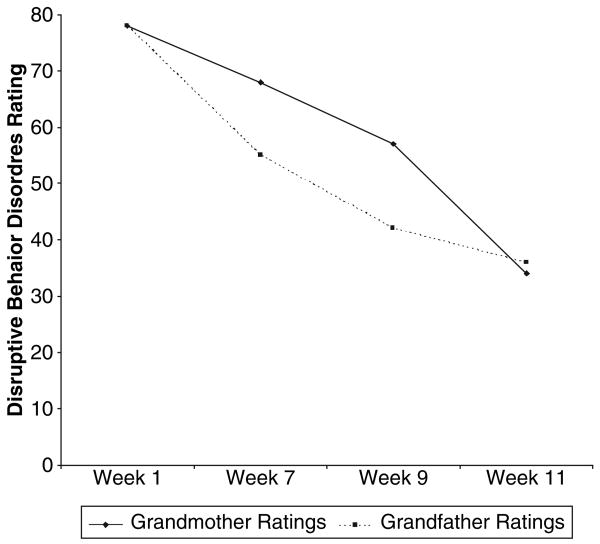
At both intake and periodically throughout treatment, caregivers completed ratings of the child's disruptive behaviors at home using the Disruptive Behavior Disorders Rating Scale–Parent Form (Barkley, 1997). This measure assessed 26 disruptive behaviors. Each behavior was rated on a scale of 0 (never or rarely) to 3 (very often). Scores can range from 0 to 78. In addition, at termination, the therapist and the child's grandmother rated the child's improvement on a Likert-type CGI scale, ranging from very much worse (1) to very much improved (7). The therapist also conducted an unstructured clinical interview of the child's RAD symptomatology at termination.
Procedure
The therapist was an advanced graduate student in clinical psychology supervised weekly by a doctorate-level, licensed clinical psychologist. Treatment was consistent with that detailed in Defiant Children: A Clinician's Manual for Assessment and Parent Training (Barkley, 1997). As outlined in this manual, BMT consists of approximately 10 sessions (or steps) and targets caregivers of children with behavioral problems. Caregiver(s) typically meet with the therapist for the first 9 sessions on a weekly basis, with the last session taking place about a month after the previous session. Step 1 consists of a discussion of various factors that can contribute to children's misbehavior and the homework assignment concerns completion of a “family problems inventory” sheet that outlines stressors (e.g., parental, familial) that may play a role in the inconsistency of discipline. Step 2 concerns a discussion of the daily implementation of “special time,” a period of approximately 20 minutes during which the child engages in an activity of her choice and caregivers simply pay attention to and comment on the child's good and/or neutral play behaviors. During Step 3, caregivers are taught techniques to increase their ability to give effective commands. Step 4 involves the implementation of a home point system used to positively reinforce compliance. After successful completion of Step 4 (i.e., implementation of a point system), Step 5 introduces disciplinary methods that are to be used for punishment (i.e., taking away of points, time out). Finally, Steps 6 through 9, as well as Step 10 (the booster session), outline strategies for generalizing timeouts to other misbehavior, modifying behavior in public places (including school), and anticipating future behavior problems to address relapse prevention. For instance, caregivers are taught to work with teachers to create daily report cards the teacher can send home with the child to report on the child's school behaviors so that caregivers can modify school behaviors using BMT techniques. The treatment manual explicitly states that each step must be successfully completed (including completion of homework/implementation of the parenting skill) before progressing to the next step (for specific information regarding BMT techniques, please see Barkley, 1997).
Treatment consisted of 12 sessions after intake. The first 11 sessions spanned 12 weeks (Step 2 was repeated because of caregiver failure to complete homework assignments) and included a diagnostic feedback session plus BMT Steps 1 through 9. Session 12 (BMT Step 10, the booster session) occurred 1 month following Session 11. Each session lasted approximately 50 minutes.
During the diagnostic feedback session, the therapist explained that, at the time of treatment, there was no empirically supported treatment for RAD and suggested the use of BMT to teach the caregivers parenting skills they could use to manage the child's problematic behaviors, including those associated with RAD (e.g., problematic eating, hugging, and self-touching behaviors). It was stressed that there was no known literature on the efficacy of BMT for RAD and that the use of BMT to modify these behaviors would be novel. The grandparents consented to the use of BMT for the treatment of the child's problematic behaviors. Goals for the treatment of RAD-related symptoms and behaviors were outlined: (a) decrease inappropriate hugging and self-touching and (b) increase child's compliance with caregiver and teacher commands to modify behaviors thought to be correlates of her RAD (e.g., inappropriate eating and toilet behaviors).
Results
Pretreatment Assessments
Consistent with DSM-IV criteria of RAD, the grandparents reported that the child exhibited severely disturbed and developmentally inappropriate social relatedness (e.g., painful and inappropriate hugging; excessive familiarity with adult figures such as previous foster parents, teachers, relatives she recently met) in most contexts (e.g., home, school) that by all accounts was apparent prior to age 5. Additionally, the child suffered from pathogenic care as evidenced by her father's long-standing neglect of the child's basic physical needs (e.g., lack of food preparation, failure to teach the child use of silverware, lack of toilet training). The child therefore met diagnostic criteria for RAD.
The grandparents' ratings on the CPRS-R suggest that they observed the child as having a variety of difficulties in areas such as social skills, organization, concentration, and attention. These ratings resulted in significant clinical elevations consistent with the child's prior diagnosis of ADHD–Combined Type and confirmed the grandparents' report of the child's disruptive behaviors. The ADHD diagnosis was also confirmed by the clinical interview.
In addition, the child scored a 78 (the highest possible score) on the Disruptive Behavior Disorders Rating Scale-Parent Form. The therapist-rated CGI severity rating at intake was 5 (markedly ill).
Overview of Treatment Response
BMT resulted in decreased problematic behaviors as well as increased compliance with caregiver and teacher commands and increased play with age-appropriate peers. To illustrate, by Session 5, both caregivers reported that the child looked forward to special time each night and was doing her homework so that she could have special time (special time was used as a reward for homework completion). During Session 6, the grandmother stated she practiced giving effective commands and that the child's compliance was increasing as a result. During Session 7, the grandmother reported that the point system had been successfully implemented as evidenced by increased compliance at home. Furthermore, she stated using the point system to reward the child for desired behaviors (e.g., appropriate toilet and eating behaviors) resulted in increased ability on the part of the child to appropriately use the toilet and eat using silverware. However, the child continued to misbehave at school (e.g., failed to comply with teacher requests). The point system was therefore modified so that the child obtained additional points at home if there were no misbehaviors reported at school and by Session 9. The grandmother reported that no points were taken away because of misbehavior at school for the entire week.
At the end of 11 sessions (Steps 1 through 9), the child's behaviors were very much improved. For instance, the grandparents reported that the child's toilet training was complete. Furthermore, the child no longer experienced UTIs, which they attributed to decreased self-touching as a result of BMT skills. They also stated that they saw the child playing with same-age peers on the playground at school. Grandparents attributed increased play to greater acceptance by her peers because of substantial decreases in the child's problematic behaviors (e.g., painful hugging). The child was complying with commands and receiving favorable reports from her teacher (who described the child as “doing well in school”). The child's grades and compliance with homework improved, and she continued to play with other children at home and on the schoolyard. Given the school's threat of expulsion, the child's school-related outcomes were particularly noteworthy.
One month after the last BMT session, the grandparents returned to treatment for a 1-month booster session (i.e., Step 10). They outlined the child's continued treatment gains. The child received top scores on the daily teacher report cards. Grandparents reported that the child was averaging approximately two timeouts per week (down from five), she no longer engaged in inappropriate or painful hugging, she continued to use the toilet and silverware appropriately, and they continued to observe her playing with other children (versus playing alone) on the schoolyard when they picked her up from school each day. The caregivers did not anticipate any future behavioral problems and stated they were pleased with the gains she had made throughout the course of BMT.
Complicating Factors
There were several factors that could have served to undermine this child's treatment outcome. First, comorbidity could have interfered with treatment. In addition, although the grandfather attended every therapy session, he was reluctant to use BMT skills. To illustrate, after Session 3, the grandmother telephoned the therapist stating that the grandfather did not complete Step 2 homework because he believed treatment was unnecessary as the child would “grow out of” her behavior problems. The therapist praised the grandmother for continuing to use BMT despite the lack of support from the grandfather. The therapist informed the grandmother that, according to the treatment manual, BMT skills could be effective even if only one caregiver used them as long as the grandfather did not attempt to undermine her use of the skills. The grandmother reported she did not believe the grandfather would attempt to undermine her use of the skills and agreed to inform the therapist should the grandfather begin to do so. However, based on grandmother report, the grandfather did not attempt to undermine the grandmother's use of BMT skills with their granddaughter.
Outcome Assessments
At termination, therapist-rated CGI was 3 (mildly ill) down from 5 (markedly ill) at intake. Furthermore, the therapist rated the child's improvement as 1 (very much improved), and the grandmother rated the child's improvement as 2 (much improved). As evidenced by Figure 1, the child's disruptive behaviors steadily and substantially decreased throughout the course of treatment. At termination, an unstructured clinical interview was conducted to assess the child's RAD symptomatology. Given the child no longer engaged in inappropriate or disturbed social relatedness, the child's RAD was considered in full remission.
Figure 1. Caregiver Ratings of Child's Disruptive Behaviors Throughout the Course of Treatment.
Discussion
As no empirically supported interventions currently exist for the treatment of children with RAD, it seems appropriate to examine the utility of treatments found to be effective for disorders that exhibit considerable symptom overlap with RAD. Given that RAD is associated with problems concerning attention as well as aggressive and defiant behaviors (Kay Hall & Geher, 2003; Millward et al., 2006), treatments aimed at managing these behaviors are indicated. BMT, a treatment designed and found to increase child compliance with the commands of authority figures and decrease problematic child behaviors (Barkley, 1997), may be particularly useful in the treatment of RAD. To begin to examine the utility of BMT in the treatment of RAD, this case study presented data regarding the effects of BMT with one child suffering from RAD.
BMT was designed to modify problematic behaviors by teaching caregivers skills that can increase children's compliance with commands and provide children with structure and predictability both at home and in environments outside the home such as school (Barkley, 1997). Because behavioral problems among children with RAD tend to be attributed to the pathogenic care, a treatment that targets parenting skills (e.g., BMT) appears particularly warranted. In the present case study, problematic behaviors related to RAD symptomatology (e.g., inappropriate hugging) and behaviors learned as a result of pathogenic care (e.g., eating with head to plate rather than using silverware) were targeted within the BMT framework. Throughout the course of BMT, the grandparents reported a decrease in (a) inappropriate attachment relations (e.g., decreased inappropriate hugging), (b) increased ability to form relationships with age-appropriate children, (c) decreased defiant behaviors in the home and school, (d) decreased self-stimulatory behaviors, and (e) improved grades and homework compliance. Given the health problems (e.g., UTIs) and school problems (e.g., threat of expulsion) this child experienced at the time the grandparents presented for treatment, these treatment gains are quite substantial.
It is particularly noteworthy that these treatment gains were made despite the complexities of this particular case, such as a comorbid diagnosis that could have interfered with treatment. Furthermore, these gains occurred in a relatively short time, despite non-compliance by one of the caregivers. This finding is consistent with Barkley's (1997) assertion that BMT can be effective for the treatment of other childhood disorders even when only one caregiver uses behavior management skills.
Despite the promising nature of these findings, there are several limitations to this case study that suggest further work in this area. First, a single case report is not sufficient to test the utility of BMT for the treatment of RAD. It is our hope that this case study, outlining the successful treatment of RAD using BMT, will spur researchers to conduct an RCT to test the efficacy of BMT for RAD. Second, although BMT encourages all primary caregivers to use parenting skills, only one caregiver implemented the techniques in the home. Thus, it could be that optimal gains were not attained and future work would benefit from the development of techniques aimed at increasing motivation to comply with BMT among all caregivers. Third, the caregivers in the present case example were not the child's biological parents. Given the high rates of RAD symptoms among children in foster care (Boris et al., 1998; Millward et al., 2006; Zeanah et al., 2004), our success with BMT for RAD has important implications for the treatment of children who are under the care of nonbiological caregivers. However, future work should also examine whether BMT is also effective for children who remain in the care of the caregivers who inflicted pathogenic care.
In sum, the successful reduction of problematic behaviors and increases in quality of life exhibited by the child in this case study indicate that BMT may demonstrate utility as a treatment for RAD and its associated impairment. Given this promising initial evidence, it is recommended that RCTs be conducted to evaluate the efficacy and effectiveness of BMT for the treatment of RAD.
Acknowledgments
Authors’ Note: This research was supported in part by an National Institutes of Health grant awarded by the National Institute of Drug Abuse to Julia D. Buckner (F31 DA021457).
Biographies
Julia D. Buckner, a PhD candidate at Florida State University, is completing an internship in the Division of Substance Abuse at the Yale University School of Medicine. Fall 2008, she will join the faculty as assistant professor of clinical psychology at Louisiana State University. Her work focuses on the nature and treatment of co-occurring anxiety and substance use disorders across the lifespan. She has received numerous awards for her research, including a National Research Service Award from the National Institute on Drug Abuse.
Cristina Lopez is a PhD candidate at Florida State University. Her clinical and research interests include disorders that onset in childhood with an emphasis on childhood internalizing disorders.
Stephanie Dunkel is a PhD candidate at Florida State University. Currently, she is a clinical psychology trainee at the Florida State Multidisciplinary Center conducting psychoeducational assessments for the purpose of identifying school-age children who meet criteria for learning disabilities, autism spectrum disorders, and attention-deficit/hyperactivity disorder. Her research interests include developmental psychopathology, children's discrepant self-perceptions, problematic social interactions of children, coping response styles, and psychopathology in juvenile offenders.
Thomas E. Joiner, Jr., PhD, is Distinguished Research Professor & The Bright-Burton Professor in the Department of Psychology at the Florida State University. His work concerns nature and treatment of depression, suicidal ideation and behavior, and related disorders (e.g., anxiety, bulimia nervosa). He has received numerous awards for his research, including the Award for Distinguished Scientific Early Career Contributions from the American Psychological Association as well as research grants from the National Institute of Mental Health and various foundations.
Contributor Information
Julia D. Buckner, Yale School of Medicine
Cristina Lopez, Florida State University.
Stephanie Dunkel, Florida State University.
Thomas E. Joiner, Jr., Florida State University
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th. Washington, DC: Author; 1994. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th, text revision. Washington, DC: Author; 2000. [Google Scholar]
- Anastopoulos AD, Shelton TL, DuPaul GJ, Guevremont DC. Parent training for attention-deficit hyperactivity disorder: Its impact on parent functioning. Journal of Abnormal Child Psychology. 1993;21:581–596. doi: 10.1007/BF00916320. [DOI] [PubMed] [Google Scholar]
- Bakermans-Kranenburg MJ, van Ijzendoorn MH, Juffer F. Less is more: Meta-analyses of sensitivity and attachment interventions in early childhood. Psychological Bulletin. 2003;129:195–215. doi: 10.1037/0033-2909.129.2.195. [DOI] [PubMed] [Google Scholar]
- Barkley RA. Defiant children: A clinician's manual for assessment and parent training. 2nd. Vol. 264. New York: Guilford; 1997. [Google Scholar]
- Barkley RA, Edwards G, Laneri M, Fletcher K, Metevia L. The efficacy of problem-solving communication training alone, behavior management training alone, and their combination for parent-adolescent conflict in teenagers with ADHD and ODD. Journal of Consulting and Clinical Psychology. 2001;69:926–941. [PubMed] [Google Scholar]
- Barth RP, Crea TM, John K, Thoburn J, Quinton D. Beyond attachment theory and therapy: Towards sensitive and evidence-based interventions with foster and adoptive families in distress. Child and Family Social Work. 2005;10:257–268. [Google Scholar]
- Boris NW, Zeanah CH. Practice parameter for the assessment and treatment of children and adolescents with reactive attachment disorder of infancy and early childhood. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44:1206–1219. doi: 10.1097/01.chi.0000177056.41655.ce. [DOI] [PubMed] [Google Scholar]
- Boris NW, Zeanah CH, Larrieu JA, Scheeringa MS, Heller SS. Attachment disorders in infancy and early childhood: A preliminary investigation of diagnostic criteria. American Journal of Psychiatry. 1998;155:295–297. doi: 10.1176/ajp.155.2.295. [DOI] [PubMed] [Google Scholar]
- Bowlby J. Attachment theory and its therapeutic implications. Adolescent Psychiatry. 1978;6:5–33. [PubMed] [Google Scholar]
- Bushman BJ. Does venting anger feed or extinguish the flame? Catharsis, rumination, distraction, anger and aggressive responding. Personality and Social Psychology Bulletin. 2002;28:724–731. [Google Scholar]
- Chaffin M, Hanson R, Saunders BE, Nichols T, Barnett D, Zeanah CH, et al. Report of the APSAC Task Force on Attachment Therapy, Reactive Attachment Disorder, and Attachment Problems. Child Maltreatment. 2006;11:76–89. doi: 10.1177/1077559505283699. [DOI] [PubMed] [Google Scholar]
- Conners CK. Manual for the Conners' Rating Scales–Revised. North Tonawanda, NY: Multi-Health Systems; 1997. [Google Scholar]
- Dozier M, Peloso E, Lindheim O, Gordon MK, Manni M, Sepulveda S, et al. Developing evidence-based interventions for foster children: An example of a randomized clinical trial with infants and toddlers. Journal of Social Issues. 2006;62:767–785. [Google Scholar]
- Eyberg SM, Boggs SR. Parent-Child Interaction Therapy: A psychosocial intervention for the treatment of young conduct-disordered children. In: Briesmeister JM, Schaefer CS, editors. Handbook of parent training: Parents as co-therapists for children's behavior. 2nd. New York: Wiley; 1998. pp. 61–97. [Google Scholar]
- Guy W, editor. ECDEU assessment manual for psychopharmacology. rev. Rockville, MD: National Institute for Mental Health; 1976. [Google Scholar]
- Hanson RF, Spratt EG. Reactive attachment disorder: What we know about the disorder and implications for treatment. Child Maltreatment. 2000;5:137–145. doi: 10.1177/1077559500005002005. [DOI] [PubMed] [Google Scholar]
- Haugaard JJ, Hazan C. Recognizing and treating uncommon behavioral and emotional disorders in children and adolescents who have been severely maltreated: Reactive attachment disorder. Child Maltreatment. 2004;9:154–160. doi: 10.1177/1077559504264316. [DOI] [PubMed] [Google Scholar]
- Hinshaw-Fusilier S, Boris NW, Zeanah CH. Reactive attachment disorder in maltreated twins. Infant Mental Health Journal. 1999;20(Special Issue Disturbances and Disorders of Attachment):42–59. [Google Scholar]
- Judit B, Andrea B, Dominika D, Eszter L, Zsuzsa T, Péter N, et al. The Hungarian Adaptation of the M. I. N. I KID/A Gyermek M.I.N.I. kérdoív magyar nyelvu változatának ismertetése. Psychiatria Hungarica. 2004;19:358–364. [Google Scholar]
- Kay Hall SE, Geher G. Behavioral and personality characteristics of children with reactive attachment disorder. Journal of Psychology: Interdisciplinary and Applied. 2003;137:145–162. doi: 10.1080/00223980309600605. [DOI] [PubMed] [Google Scholar]
- Mercer J. Warning: Are you aware of “holding therapy”? Pediatrics. 2001;107:1498. [PubMed] [Google Scholar]
- Millward R, Kennedy E, Towlson K, Minnis H. Reactive attachment disorder in looked-after children. Emotional and Behavioural Difficulties. 2006;11:273–279. [Google Scholar]
- Myeroff R, Mertlich G, Gross J. Comparative effectiveness of holding therapy with aggressive children. Child Psychiatry and Human Development. 1999;29:303–313. doi: 10.1023/a:1021349116429. [DOI] [PubMed] [Google Scholar]
- Parker KC, Forrest D. Attachment disorder: An emerging concern for school counselors. Elementary School Guidance and Counseling. 1993;27:209–215. [Google Scholar]
- Reber K. Children at risk for reactive attachment disorder: Assessment, diagnosis, and treatment. Progress: Family Systems Research and Therapy. 1996;5:83–98. [Google Scholar]
- Richters MM, Volkmar FR. Reactive attachment disorder of infancy or early childhood. Journal of the American Academy of Child and Adolescent Psychiatry. 1994;33:328–332. doi: 10.1097/00004583-199403000-00005. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuro-psychiatric Interview (M.I.N.I): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59:22–33. [PubMed] [Google Scholar]
- Speltz ML. Description, history, and critique of Corrective Attachment Therapy. The APSAC Advisor. 2002;14:4–8. [Google Scholar]
- van Ijzendoorn MH, Schuengel C, Bakermans-Kranenburg MJ. Disorganized attachment in early childhood: Meta-analysis of precursors, concomitants, and sequelae. Development and Psychopathology. 1999;11:225–249. doi: 10.1017/s0954579499002035. [DOI] [PubMed] [Google Scholar]
- Webster-Stratton C, Reid MJ. The Incredible Years Parents, Teachers, and Children Training Series: A multifaceted treatment approach for young children with conduct problems. In: Kazdin AE, Weisz JR, editors. Evidence-based psychotherapies for children and adolescents. New York: Guilford; 2003. pp. 224–240. [Google Scholar]
- World Health Organization. Composite International Diagnostic Interview (CIDI) Version 1.0. Geneva, Switzerland: Author; 1990. [Google Scholar]
- Zeanah CH, Scheeringa M, Boris NW, Heller SS, Smyke AT, Trapani J. Reactive attachment disorder in maltreated toddlers. Child Abuse and Neglect. 2004;28:877–888. doi: 10.1016/j.chiabu.2004.01.010. [DOI] [PubMed] [Google Scholar]