Lyme disease, which is caused by the bacterium Borrelia burgdorferi, is transmitted by the bite of an infected tick vector. There are 2 reasons Lyme disease has not been common in Canada. First, although populations of the western black-legged tick, Ixodes pacificus, are established throughout parts of southern British Columbia, this tick infrequently bites humans and relatively few ticks are infected.1 Second, the black-legged tick, Ixodes scapularis (Figures 1 and 2), is currently established in only a few specific locations in central and eastern Canada (known as endemic areas), including areas within southeastern Manitoba, southern and eastern Ontario, southeastern Nova Scotia, and, as preliminary data suggest, southern Quebec and New Brunswick. However, these black-legged ticks are more likely to bite humans and a relatively high proportion are infected.1
Figure 1.

Nymphal black-legged ticks (Ixodes scapularis) in various stages of engorgement
Figure 2. Adult female black-legged ticks (I scapularis) in various stages of engorgement.

Black-legged ticks transmit Borrelia burgdorferi in both nymphal and adult female life stages
There is a low but nonetheless real risk of infection in people across Canada, even in areas where ticks are not established, owing to ticks that are dispersed from endemic areas by migratory birds. Studies suggest that the range of the black-legged tick is expanding in some parts of eastern and possibly central Canada, and the scope of endemic areas is thought to be increasing—a process that could accelerate with climate change.1,2 Lyme disease will be nationally notifiable in Canada by the end of 2008.
Know the signs
Early Lyme disease is characterized by an expanding area of erythema extending from the site where the infecting tick bite occurred. This lesion, called erythema migrans (EM), is typically > 5 cm and is not normally associated with the typical signs of skin inflammation, such as itchiness, scaling, pain, swelling, or exudation (Figures 3 and 43). Erythema migrans appears 1 to 2 weeks (range of 3 to 30 days) after infection and persists for up to 8 weeks, by which time the bacterium has left the skin and disseminated hematogenously. For a short period (< 48 hours) after the tick bite, there might be a limited circular area of inflammation where the tick bite penetrated the skin. Patients with EM might suffer from nonspecific signs, such as fatigue, headache, and arthralgia.
Figure 3.

A patient with an erythema migrans lesion
Figure 4. A patient with an erythema migrans lesion.

The small central area of inflammation is likely a response to the tick bite, not to Borrelia burgdorferi
Disseminated Lyme disease is associated with various symptoms:
Neurologic signs or neuroborreliosis
Acute peripheral nervous system involvement associated with Lyme disease includes radiculopathy, cranial neuropathy (Bell palsy, Figure 5), and mononeuropathy multiplex. Central nervous system involvement includes lymphocytic meningitis and, rarely, encephalomyelitis (parenchymal inflammation of brain or spinal cord, with focal abnormalities). Neurologic symptoms of late Lyme disease can include encephalomyelitis, peripheral neuropathy, or encephalopathy.
Figure 5.

A patient suffering from neuroborreliosis (Bell palsy)
Musculoskeletal signs
Lyme arthritis is a monoarticular or oligoarticular form of arthritis most commonly involving the knee (Figure 6). It can, however, also affect other large joints or the temporomandibular joint. Large effusions that are disproportionate to the pain are typical. If untreated, Lyme arthritis is often intermittent, with episodes of joint inflammation spontaneously resolving after a few weeks to a few months. Persistent swelling of the same joint for 12 months or more is not a usual presentation.
Figure 6.

Lyme arthritis in the knee
Cardiac signs
Cardiac involvement associated with Lyme disease includes intermittent atrioventricular heart block, often involving the atrioventricular node (although heart block can occur at multiple levels), and sometimes myopericarditis. Carditis can occur in early stages of the disease.
Erythema migrans
Multiple EM lesions can occur in early disseminated Lyme disease.
A condition referred to as “chronic Lyme disease” has been suggested by a small number of medical practitioners, but its existence is viewed with scepticism by the mainstream medical community.4
Diagnosis
Diagnosis is made based on clinical signs and supported, where possible, by laboratory tests. Laboratory diagnosis using the 2-tier antibody testing method is recommended5,6; however, there are some caveats to this test:
Many patients with EM and some patients with early disseminated Lyme disease receive negative test results, although most patients become sero-positive as the infection progresses in untreated individuals.
A small percentage of patients with early Lyme disease who are treated with antibiotics will not produce an antibody response to infection, and will therefore continue to have negative serologic test results.7
Confidence in a positive serologic test result is greater if the patient has a history of living in or visiting an endemic area.
Caution against the use of laboratory tests in which accuracy and clinical usefulness have not been adequately established has been published, as well as caution against tests that use interpretation criteria that have not been properly validated.8
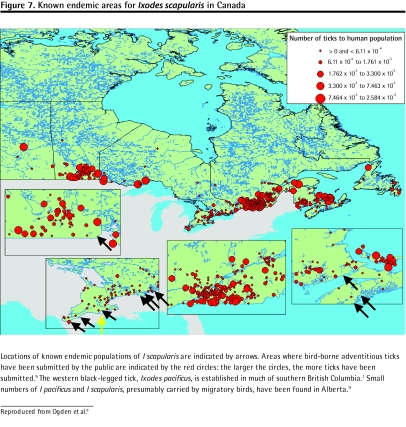
In Canada
Residence in, or a visit to, an endemic area of Canada (Figure 79) or abroad (eg, the United States, much of Europe, and temperate Asia) provides strong support for a clinical diagnosis. Lyme disease, however, cannot be ruled out in people who do not fit the above criteria, as it is possible to be bitten by infected ticks transported from endemic areas by migratory birds. The risk of Lyme disease is greatest in spring and early summer, when the nymphal ticks are most active, but can also occur into late autumn.
Figure 7. Known endemic areas for Ixodes scapularis in Canada.
Locations of known endemic populations of I scapularis are indicated by arrows. Areas where bird-borne adventitious ticks have been submitted by the public are indicated by the red circles: the larger the circles, the more ticks have been submitted.9 The western black-legged tick, Ixodes pacificus, is established in much of southern British Columbia.1 Small numbers of I pacificus and I scapularis, presumably carried by migratory birds, have been found in Alberta.9
If patients find feeding ticks on their skin, they can submit the ticks to the National Microbiology Laboratory for identification and testing for B burgdorferi infection (visit www.phac-aspc.gc.ca/id-mi/tickinfo-eng.php for more details). Patients with compelling clinical symptoms should be treated without waiting for diagnostic test results of submitted ticks.
Treatment
A 14-day course of treatment with appropriate antibiotics (eg, 100 mg of doxycycline twice daily, 500 mg of amoxicillin 3 times a day, or 500 mg of cefuroxime axetil twice daily) is effective in early Lyme disease.10 (Note that cephalexin is ineffective.) Treatment of disseminated Lyme disease patients is best conducted by, or under the advice of, an infectious disease specialist.
Prevention of Lyme disease
Lyme disease is a preventable disease. The following are recommendations from the Public Health Agency of Canada:
Wear long pants and long-sleeved shirts when walking in wooded areas where ticks might be present.
Tuck trousers into socks, limiting the access of ticks to bare skin where they can feed.
Wear light-coloured clothing. It is easier to see and remove any ticks that come in contact with light-coloured surfaces rather than dark-coloured. Apply insect repellents that contain DEET (diethyltoluamide) to clothing or exposed skin. To maintain effectiveness, product application might have to be repeated more frequently than required to prevent mosquito or black fly bites. Always follow the label directions when applying any insect repellent.
Perform a careful self-examination for attached ticks after being in a potential tick habitat. If infected and feeding ticks are removed within 36 hours of attachment, transmission of Borrelia burgdorferi is prevented in most cases.
Use tweezers to remove an attached tick. Grasp the tick’s head and mouth parts as close to the skin as possible, and pull slowly until the tick is removed. Be careful not to twist, rotate, or crush the tick during removal.
After removing the tick, use soap and water to wash the site where the tick was attached.
If clinical signs appear, seek treatment early. Treatment is much easier in early Lyme disease and appropriate treatment might prevent the more severe and debilitating symptoms of disseminated Lyme disease.
Footnotes
Competing interests
None declared
Reproduced from Ogden et al.9
References
- 1.Ogden NH, Lindsay RL, Sockett PN, Morshed M, Artsob H. The rising challenge of Lyme disease in Canada. Can Commun Dis Report. 2008;34(1):1–19. [PubMed] [Google Scholar]
- 2.Ogden NH, Maarouf A, Barker IK, Bigras-Poulin M, Lindsay LR, Morshed MG, et al. Climate change and the potential for range expansion of the Lyme disease vector Ixodes scapularis in Canada. Int J Parasitol. 2006;36(1):63–70. doi: 10.1016/j.ijpara.2005.08.016. Epub 2005 Oct 5. [DOI] [PubMed] [Google Scholar]
- 3.White GM, Cox NH. Diseases of the skin: a color atlas and text. 2. St Louis, MO: Mobsy; 2005. chap 24. [Google Scholar]
- 4.Feder HM, Jr, Johnson BJ, O’Connell S, Shapiro ED, Steere AC, Wormser GP, et al. A critical appraisal of “chronic Lyme disease. N Engl J Med. 2007;357(14):1422–30. doi: 10.1056/NEJMra072023. [DOI] [PubMed] [Google Scholar]
- 5.Canadian Public Health Laboratory Network. The laboratory diagnosis of Lyme borreliosis: guidelines from the Canadian Public Health Laboratory Network. Can J Infect Dis Med Microbiol. 2007;18(2):145–8. doi: 10.1155/2007/495108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Recommendations for test performance and interpretation from the Second National Conference on Serologic Diagnosis of Lyme Disease. [Accessed 2008 Aug 20];MMWR Morb Mortal Wkly Rep. 1995 44(31):590–1. Available from: www.cdc.gov/mmwr/preview/mmwrhtml/00038469.htm. [PubMed]
- 7.Aguero-Rosenfeld ME, Nowakowski J, Bittker S, Cooper D, Nadelman RB, Wormser GP. Evolution of the serologic response to Borrelia burgdorferi in treated patients with culture-confirmed erythema migrans. [Accessed 2008 Aug 20];J Clin Microbiol. 1996 34(1):1–9. doi: 10.1128/jcm.34.1.1-9.1996. Available from: http://jcm.asm.org/cgi/reprint/34/1/1?view=long&pmid=8748261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. Caution regarding testing for Lyme disease. [Accessed 2008 Aug 20];MMWR Morb Mortal Wkly Rep. 2005 54(5):125. Available from: www.cdc.gov/mmwr/preview/mmwrhtml/mm5405a6.htm.
- 9.Ogden NH, Trudel L, Artsob H, Barker IK, Beauchamp G, Charron DF, et al. Ixodes scapularis ticks collected by passive surveillance in Canada: analysis of geographic distribution and infection with Lyme borreliosis agent Borrelia burgdorferi. J Med Entomol. 2006;43(3):600–9. doi: 10.1603/0022-2585(2006)43[600:ISTCBP]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 10.Wormser GP, Dattwyler RJ, Shapiro ED, Halperin JJ, Steere AC, Klempner MS, et al. The clinical assessment, treatment, and prevention of lyme disease, human granulocytic anaplasmosis, and babesiosis: clinical practice guidelines by the Infectious Diseases Society of America. [Accessed 2008 Aug 25];Clin Infect Dis. 2006 43(9):1089–134. doi: 10.1086/508667. Epub 2006 Oct 6. Available from: www.journals.uchicago.edu/doi/pdf/10.1086/508667?cookieSet=1. [DOI] [PubMed] [Google Scholar]