Abstract
OBJECTIVE—Pressure mitigation is crucial for the healing of plantar diabetic foot ulcers. We therefore discuss characteristics and considerations associated with the use of offloading devices.
RESEARCH DESIGN AND METHODS—A diabetic foot ulcer management survey was sent to foot clinics in all 50 states and the District of Columbia in 2005. A total of 901 geographically diverse centers responded. The survey recorded information regarding usage frequency and characteristics of assessment and treatment of diabetic foot ulcers in each center.
RESULTS—Of the 895 respondents who treat diabetic foot ulcers, shoe modifications (41.2%, P < 0.03) were the most common form of pressure mitigation, whereas total contact casts were used by only 1.7% of the centers.
CONCLUSIONS—This study reports the usage and characteristics of offloading devices in the care of diabetic foot ulcers in a broadly distributed geographic sample. Less than 2% of specialists use what has been termed the “gold standard” (total contact cast) for treating the majority of diabetic foot ulcers.
In the treatment of diabetic foot ulcers, pressure modulation, commonly referred to as “offloading,” is most successful when pressure is mitigated at an area of high vertical or shear stress (1). Common methods to offload the foot include bed rest, wheel chair, crutch-assisted gait, total contact casts, felted foam, half shoes, therapeutic shoes, and removable cast walkers (2). Although it is well known that pressure mitigation through offloading devices is crucial for the healing of plantar diabetic foot ulcers, there are, to the best of our knowledge, no reports in the literature that describe the characteristics and considerations associated with the use of pressure mitigation devices in a broad geographically diverse sample of specialists. Therefore, the purpose of this study was to describe the characteristics and considerations associated with the use of offloading devices in foot clinics in the U.S.
RESEARCH DESIGN AND METHODS
A diabetic foot management survey was sent to 5,200 private and academic practices and clinics in all 50 states and the District of Columbia in 2005. A total of 901 geographically diverse centers responded from 48 states and the District of Columbia. The data were analyzed by dividing the U.S. into four census regions (West, Midwest, South, and Northeast) based on regions described by the U.S. Census Bureau. The survey recorded information about the usage frequency and characteristics of assessment and treatment of diabetic foot ulcers in each center.
RESULTS
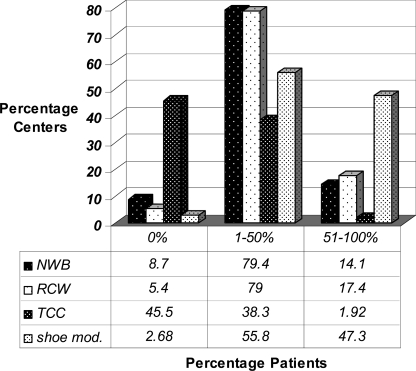
Of the 901 respondents, 895 centers actively treated diabetic foot ulcers. The type and frequency of plantar offloading used is summarized in Figure 1. Of the 895 centers, shoe modifications (41.2%, P < 0.03) were the most common form of pressure mitigation in >51% of diabetic foot ulcer treatments. There were no significant regional differences in therapy. Total contact casts (TCCs) were used by only 1.7% of the centers for the majority of diabetic foot ulcer treatment, whereas 15.2% of the centers reported use of removable cast walkers. A total of 2.6% of the centers reported application of other modalities such as therapeutic shoes, and 12.3% of the centers reported use of complete non–weight-bearing (NWB) strategies such as crutches and wheelchairs for the majority of treatment. A total of 58.1% (520 centers) did not consider TCCs as the gold standard to offload the noninfected plantar diabetic foot ulcers. A total of 45.5% of the centers nationwide reported no use of TCCs as an offloading modality. Commonly reported factors affecting frequency of TCC usage included patient tolerance (55.3%), the time needed to apply the cast (54.3%), cost of materials (31.6%), reimbursement issues (27.5%), familiarity with method of application (25%), customizing parts (20.9%), staffing/ordering supplies (15.2%), and clinician coverage (10.6%).
Figure 1.
Type and frequency of plantar offloading used across 895 clinics.
CONCLUSIONS
TCCs have been considered the gold standard by academicians and consensus committees alike (3); however, the results of this study suggest that this standard is actively used by merely 1.7% of centers for treatment of the majority of plantar diabetic foot ulcer treatment. Most of the centers (73.4%) used TCCs in <25% of their patients, but (at best) intermittently. A further 45.5% of centers reported not using TCCs at all. This discrepancy between consensus documents, randomized controlled trials, and clinical reality may be secondary to a number of potential negative attributes that may discourage clinicians from using this modality. TCC application is time-consuming and often associated with a learning curve. Most centers do not have a physician or cast technician available with adequate training or experience to safely apply a TCC. Moreover, TCCs do not allow patients, family members, or health care providers to assess the foot or wound on a daily basis and are therefore often contraindicated in cases of soft tissue infections or osteomyelitis. Other patient complaints may include impaired activities of daily living, such as difficulty sleeping comfortably, and bathing difficulties while trying to avoid getting the cast wet. Certain designs of TCCs may also exacerbate postural instability (4).
Removable cast walkers (RCW) are, as their name implies, cast-like devices that are removable to allow for self-inspection of the wound and application of topical therapies that require frequent administration. Further, RCWs can be easily converted into an instant TCC (iTCC) (5). Wound healing efficacy and cost-effectiveness of iTCCs have been demonstrated in several randomized controlled trials (6,7). However, the results of this survey suggested that RCWs were only used by 15.2% of the centers in the treatment of the majority of the wounds treated. Almost half of the centers (48%) used RCWs in <25% of plantar diabetic foot ulcers. The most likely explanation is the cost and lack of reimbursement associated with RCWs in the U.S. Most patients either cannot or are not willing to pay the extra money for the RCW, forcing clinicians to absorb the extra cost.
Whereas no offloading modality was used 100% of the time by the centers assessed, shoe modification was by far the most commonly used. This is despite data that suggests these are not effective means of offloading (8). Additionally, there are real concerns that an aperture applied around the wound based solely on visual cues may increase shear and vertical forces at the wound's periphery secondary to the “edge effect” (9). The popularity of shoe modifications may be secondary to many factors. Patients are often resistant to cast applications or the extra costs associated with RCWs. Clinicians are therefore compelled to use alternative methods such as shoe modifications that are less costly and reimbursable. Further, patients are often more tolerant of the slight modifications made to shoes with which they are familiar.
We are unaware of other reports in the medical literature that have reported usage frequency and characteristics of offloading devices in the podiatric medical care of diabetic foot ulcers. Fewer than 2% of centers use what has been termed the gold standard (TCCs) for treating the majority of diabetic foot ulcers in this broadly distributed sample. Based on these findings, it is likely that although most specialists understand that amelioration of pressure, shear, and repetitive injury are principal tenets of diabetic foot ulcer care, the cost/benefit analysis, realities of maintaining a busy clinical practice, the available manpower, and reimbursement issues may influence clinicians to use less optimal pressure mitigation methods.
Published ahead of print at http://care.diabetesjournals.org on 11 August 2008.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C Section 1734 solely to indicate this fact.
References
- 1.Armstrong DG, Lavery LA, Bushman TR: Peak foot pressures influence healing time of diabetic ulcers treated with total contact casting. J Rehabil Res Dev 35:1–5, 1998 [PubMed] [Google Scholar]
- 2.Wu SC, Crews RT, Armstrong DG: The pivotal role of offloading in the management of neuropathic foot ulceration. Curr Diab Rep 5:423–429, 2005 [DOI] [PubMed] [Google Scholar]
- 3.Lower extremity amputation episodes among persons with diabetes: New Mexico, 2000. MMWR Morb Mortal Wkly Rep 52:66–68, 2003 [PubMed] [Google Scholar]
- 4.Lavery LA, Fleishli JG, Laughlin TJ, Vela SA, Lavery DC, Armstrong DG: Is postural instability exacerbated by off-loading devices in high risk diabetics with foot ulcers? Ostomy Wound Manage 44:26.-32: 34, 1998 [PubMed] [Google Scholar]
- 5.Armstrong DG, Short B, Espensen EH, Abu-Rumman PL, Nixon BP, Boulton AJ: Technique for fabrication of an “instant total-contact cast” for treatment of neuropathic diabetic foot ulcers. J Am Podiatr Med Assoc 92:405–408, 2002 [DOI] [PubMed] [Google Scholar]
- 6.Armstrong DG, Lavery LA, Wu S, Boulton AJ: Evaluation of removable and irremovable cast walkers in the healing of diabetic foot wounds: a randomized controlled trial. Diabetes Care 28:551–554, 2005 [DOI] [PubMed] [Google Scholar]
- 7.Katz IA, Harlan A, Miranda-Palma B, Prieto-Sanchez L, Armstrong DG, Bowker JH, Mizel MS, Boulton AJ: A randomized trial of two irremovable off-loading devices in the management of plantar neuropathic diabetic foot ulcers. Diabetes Care 28:555–559, 2005 [DOI] [PubMed] [Google Scholar]
- 8.Fleischli JG, Lavery LA, Vela SA, Ashry H, Lavery DC: 1997 William J Stickel Bronze Award: Comparison of strategies for reducing pressure at the site of neuropathic ulcers. J Am Podiatr Med Assoc 87:466–472, 1997 [DOI] [PubMed] [Google Scholar]
- 9.Armstrong DG, Athanasiou KA: The edge effect: how and why wounds grow in size and depth. Clin Podiatr Med Surg 15:105–108, 1998 [PubMed] [Google Scholar]