Abstract
A 16 year old amateur soccer player sustained a minor head injury while contesting a ball in the air. He was unconscious for two minutes and remained “dizzy” for about an hour. After two days he developed a profound left lower motor neurone facial nerve palsy. He was found to have a complex fracture of the left petrous temporal bone, with fluid in the left middle ear and left mastoid. Treatment was conservative with oral steroids and oral co‐amoxiclav and a left myringotomy to decompress his middle ear. The spectrum of aetiology, presentation, and prognosis for facial nerve injuries is discussed.
Keywords: haemotympanum, delayed palsy, steroids, facial nerve palsy, head injury
A 16 year old amateur soccer player sustained a minor head injury while contesting a ball in the air. His opponent's head struck his left pre‐auricular area. He was unconscious for two minutes and remained “dizzy” for about an hour.
He presented to the accident and emergency department of our district general hospital six hours later, complaining of “crunching” around the left side of his jaw on closing his mouth and of a partial loss of hearing in his left ear. On examination his Glasgow coma score was 15 and his cranial nerves were intact. He had surgical emphysema in the left pre‐auricular area and blood in the left external auditory canal. Jaw occlusion was normal.
Plain skull films (in accordance with SIGN guidelines1) were normal but, given the clinical suspicion of a (basal) skull fracture, he was admitted for observation and computed tomographic (CT) scanning the following morning. Neurological observations were normal overnight and he proceeded to CT examination. No skull fracture was seen. He was, however, kept in for a further 48 hours of observation as he clinically had a basal skull fracture.
On the morning of his expected discharge he complained of an inability to close his left eye. He had first noticed this the previous evening and it had gradually worsened overnight. Cranial nerve examination revealed a profound left lower motor neurone facial nerve palsy (fig 1). All other cranial nerves had preserved function. He had no alteration in taste, but still complained of deafness. Review of his CT images in the light of this development revealed free gas in the tissues around the left mandible and left temporomandibular joint (fig 2). The images also raised suspicion of a fracture through the mastoid inferiorly.
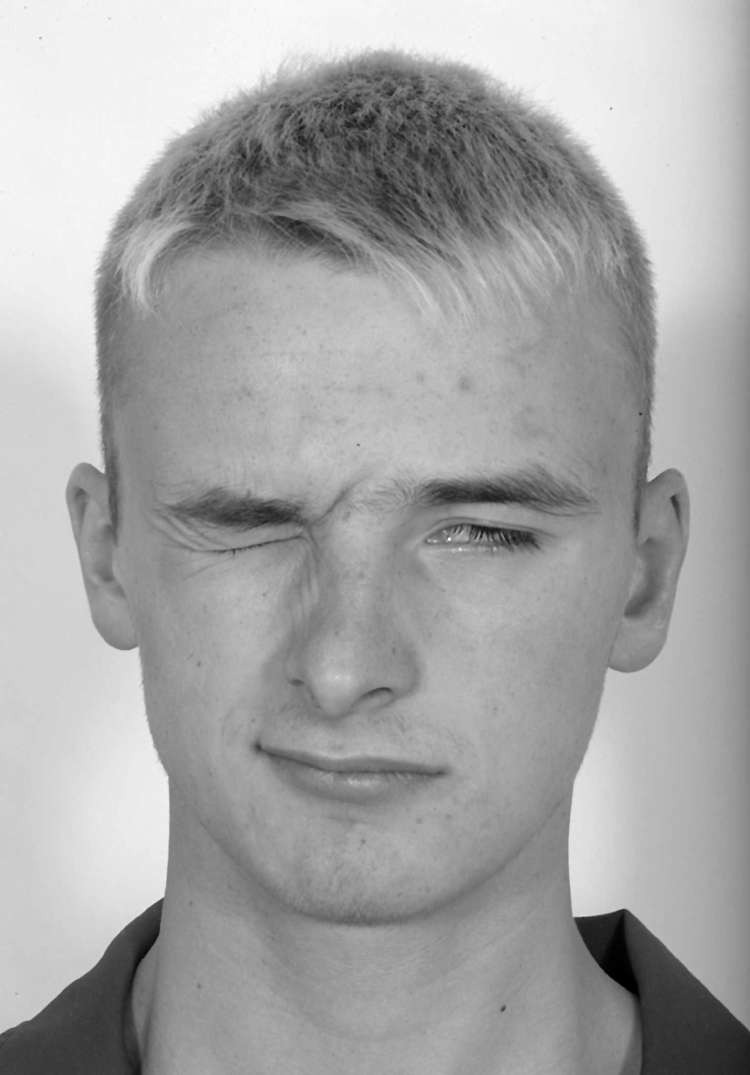
Figure 1 Profound left lower motor neurone facial nerve palsy resulting in inability to close left eye. Reproduced with permission from the patient.
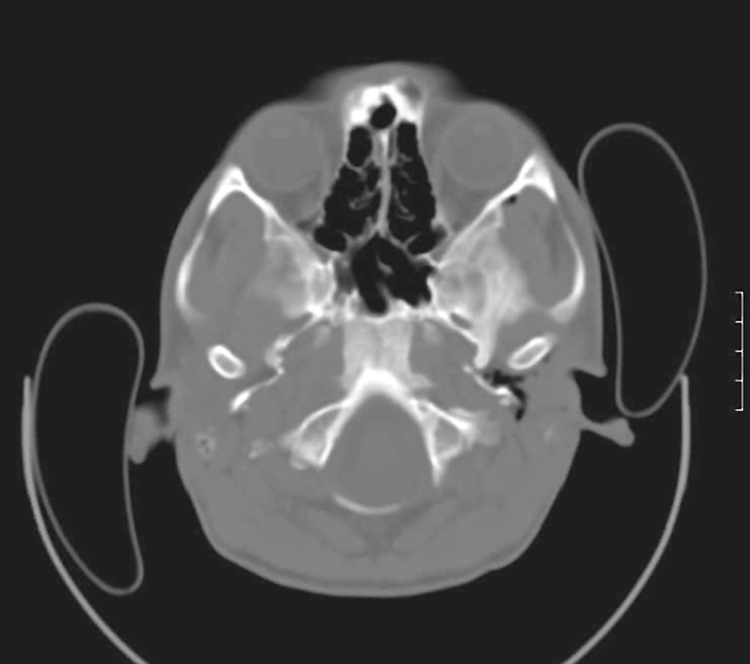
Figure 2 Gas around the left temporomandibular joint.
He was reviewed by an ENT surgeon the following morning, who recommended CT scanning of the temporal bones. This revealed a complex fracture of the left petrous temporal bone, with fluid in the left middle ear and left mastoid (fig 3). There was no evidence of ossicular disruption or damage to the geniculate ganglion or stylomastoid foramen. Clinical attempts to localise his lesion by his symptoms were limited by a haemotympanum, suggesting a mechanical as well as possible neurological cause for his hearing deficit.
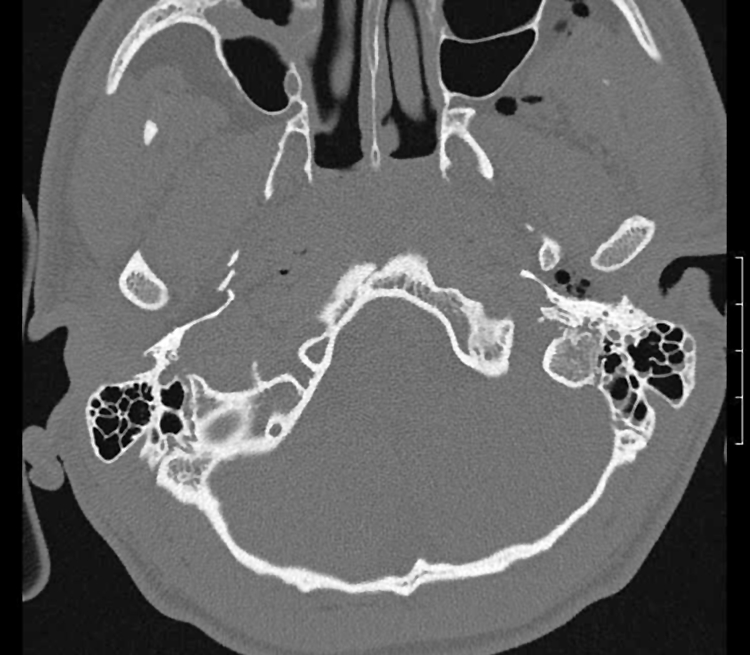
Figure 3 Fluid in left mastoid air cells. Reproduced with permission from the patient.
On the basis of the history (delayed onset and subacute progression), CT scan, and a bulging tympanic membrane, he was thought to have facial nerve compression secondary to swelling (haematoma with or without infection) rather than direct trauma. He was treated conservatively with oral steroids and oral co‐amoxiclav and underwent left myringotomy to decompress his middle ear.
He was allowed home the following day and reviewed in the ENT clinic two weeks later. At that point his facial nerve had recovered almost completely and he was discharged. When seen a further two months later he had no residual signs.
Discussion
Post‐traumatic facial nerve palsy is relatively common, especially when the temporal bone is fractured.2 It can be categorised as either immediate or delayed onset.3 The more common type of injury is immediate onset,2 which usually results from direct laceration or contusion of the nerve at the site of a temporal bone fracture. Delayed onset palsy is most commonly caused by oedema, external compression by haematoma fluid, or arterial or venous thrombosis and is not usually noticed until four or five days after head injury. This results in partial or complete degeneration of the nerve.
High resolution CT scanning of the petrous temporal bones is indicated in all cases of immediate onset facial nerve palsy so that the relation between a fracture and the facial canal can be determined. Immediate onset facial palsy with fracture through the facial canal is an indication for early surgical intervention.4,5
The facial nerve is prone to trauma as it passes through the skull base. The most common closed injury is a basal skull fracture, but there is controversy about the best management of these patients.6 Some surgeons believe, if facial paralysis is delayed in onset, treatment may be expectant, particularly if CT scans do not show a disruption of the facial canal. Others tend to explore more promptly, particularly if the palsy occurred immediately, giving a high likelihood that the nerve was injured by direct impingement or transected at fracture.
What is already known on this topic
The facial nerve has a potentially precarious route through the temporal bone, leaving it liable to injury when the base of the skull is fractured
Generally traumatic facial nerve palsies are felt to recover poorly, mainly because of a perceived large magnitude of trauma causing a skull fracture
What this study adds
This case illustrates the spectrum of aetiology, presentation, and prognosis for facial nerve injuries, which can occur with relatively minor trauma in a sporting setting
Initial clinical suggestion of temporal bone injury can “red flag” compression or laceration to the facial nerve and such athletes need to be monitored accordingly
Electrodiagnostic studies can be used in patients with traumatic facial palsy to determine prognosis. Prognosis with neuropraxia can be excellent, but neurotmesis confers a much less optimistic outlook.2 These tests are not usually carried out unless there is complete facial nerve paralysis.
Most authorities report quite a slow recovery of function after traumatic facial nerve palsy, with the degree of palsy having a greater influence on recovery of function than the time of onset. Adegbite et al7 found that, in a study of 25 patients with post‐traumatic facial nerve palsy, complete recovery had occurred at the four month point in 62% of patients who had a partial lesion, but in none of those who had complete paralysis. Recovery of function of the facial nerve can be graded using the House‐Brackmann system (table 1).8 Despite the delayed onset and complete facial nerve paralysis with rather rapid recovery, the grade in this case was thankfully grade I, equating to total recovery of the patient's left facial nerve.
Table 1 House‐Brackmann facial grading scale.
| Grade | Description | Characteristics | Estimated function (%) |
|---|---|---|---|
| I | Normal | Normal facial function in all nerve branches | 100 |
| II | Slight | Gross: slight weakness on close inspection, slight synkinesis | 80 |
| At rest: normal tone and symmetry | |||
| Motion: forehead, good to moderate movement; eye, complete closure with minimum effort; mouth, slight asymmetry | |||
| III | Moderate | Gross: obvious but not disfiguring facial asymmetry. Synkinesis is noticeable but not severe. May have hemi‐facial spasm or contracture | 60 |
| At rest: normal tone and symmetry | |||
| Motion: forehead, slight to moderate movement; eye, complete closure with effort; mouth, slight weakness with maximum effort | |||
| IV | Moderately severe | Gross: asymmetry is disfiguring and/or obvious facial weakness | 40 |
| At rest: normal tone and symmetry | |||
| Motion: forehead, no movement; eye, incomplete eye closure; mouth, asymmetrical with maximum effort | |||
| V | Severe | Gross: only slight, barely noticeable, movement | 20 |
| At rest: asymmetrical facial appearance | |||
| Motion: forehead, no movement; eye, incomplete closure; mouth, slight movement | |||
| VI | Total | No facial function | 0 |
The House‐Brackmann scale8 is the most commonly used facial nerve grading scale. It is used to approximate the quantity of volitional motion the patient has based on their clinical facial presentation. Although it is based on clinical observation, and variation among observers exists, it allows us to grossly describe the characteristics and degree of facial nerve motion using a subjective analysis scale, which is easily and reliably applied.
Footnotes
Competing interests: none declared
Figure 1 is reproduced with the patient's permission.
References
- 1.Scottish Intercollegiate Guidelines network New guidelines for the treatment of patients with head injuries. www.sign.ac.uk (accessed 21 Dec 2005)
- 2.Li J, Goldberg G, Munin M C.et al Post‐traumatic bilateral facial palsy: a case report and literature review. Brain Injury 200418315–320. [DOI] [PubMed] [Google Scholar]
- 3.Diamond C, Frew I.The facial nerve. Oxford: Oxford University Press, 1979162–256.
- 4.Darrouzet V, Bonfils‐Dindart C, Bebear J P. Management of post‐traumatic facial paralysis. A decision based on a series of 85 cases. Neurochirurgie 199844235–246. [PubMed] [Google Scholar]
- 5.Darrouzet V, Duclos J Y, Liguoro D.et al Management of facial paralysis resulting from temporal bone fractures: our experience in 115 cases. Otolaryngol Head Neck Surg 200112577–84. [DOI] [PubMed] [Google Scholar]
- 6.Nadol J B., Jr Facial paresis and paralysis. In: Wilson WR, Nadol Jr JB, Randolph GW, eds. The clinical handbook of ear, nose and throat disorders. Lancaster: Parthenon Publishing Group, 2002113–131.
- 7.Adegbite A B, Khan M I, Tan L. Predicting recovery of facial nerve function following injury from a basilar skull fracture. J Neurosurg 199175759–762. [DOI] [PubMed] [Google Scholar]
- 8.House J W, Brackmann D E. Facial nerve grading system. Otolaryngol Head Neck Surg 198593146–147. [DOI] [PubMed] [Google Scholar]


