Abstract
Background
We compared 89 older abstinent alcoholics (OAA, mean abstinence of 14.8 yrs), to 53 age and gender comparable older non-alcoholic controls (ONC) with regard to lifetime and current psychiatric diagnoses, lifetime psychiatric symptom counts, and psychological measures in the mood, anxiety, and externalizing disorder domains. We compared these findings with our previously reported results in analogous middle-aged samples (MAA versus MNC).
Methods
The methods used were the same as in our previous study of MAA versus MNC.
Results
OAA had more lifetime psychiatric and mood disorder diagnoses than ONC. They also had more lifetime symptoms and psychological test evidence of psychiatric disorder in all domains. However, OAA were less different from ONC than were MAA from MNC on most psychiatric and psychological measures. In both studies, differences between alcoholics and controls were dramatically larger in the externalizing compared with the mood and anxiety domains, and there was little evidence that psychiatric comorbidity measures impacted abstinence duration.
Conclusions
The finding that OAA had less psychiatric illness than MAA may involve a combination of selective survivorship, selection bias, and cohort differences. Although selection bias may be present in clinical studies of samples of any age, it is a more potent problem in older samples. However, given these potential biases, our results underestimate psychiatric comorbidity in OAA, strengthening our finding of increased psychiatric disorder in OAA versus ONC.
Keywords: abstinence, comorbid psychiatric illness, externalizing, anxiety, mood
1. Introduction
Over the past 15 years, the pervasiveness of psychiatric comorbidity in alcohol use disorders (AUD) and drug use disorders (DUD) has been well documented in epidemiological studies with very large community samples (Grant et al., 2004a; Grant et al., 2004b; Kessler et al., 1997; Regier et al., 1990), with even greater psychiatric comorbidity in samples drawn from treatment settings (Helzer and Pryzbeck, 1988; Regier et al., 1990; Tomasson and Vaglum, 1995). There is now a well-developed literature showing high rates of lifetime and current psychiatric diagnoses in both active alcoholics and alcoholics with short-term abstinence (Grant et al., 2004a; Grant et al., 2004b; Kessler et al., 1996; Merikangas et al., 1998; Regier et al., 1990). However, there is far less data on alcoholics with long-term abstinence, and also little data on sub-diagnostic psychiatric disorders in alcoholics, as opposed to psychiatric symptomatology that meets criteria for diagnosis. We recently addressed these issues (Di Sclafani et al., 2007; Fein et al., 2007), comparing middle-aged long-term abstinent alcoholics (MAA; mean age=46.5 years, mean abstinence 6.3 years) to age and gender-comparable middle-aged non-alcoholic controls (MNC). We found that MAA compared with MNC had: 1) an increased prevalence of lifetime mood, anxiety, and externalizing disorder diagnoses, 2) an increased prevalence of current (prior 12 month) mood and anxiety disorder diagnoses, and 3) there was no association of duration of abstinence with lifetime or current psychiatric diagnoses, consistent with psychiatric diagnoses having little or no effect on relapse. Examining psychiatric symptom counts and psychological measures associated with psychiatric disorders, we found that the bulk of the difference between groups was sub-diagnostic. Finally, we found that the difference in the presence and severity of psychiatric disorders (both diagnostic and sub4 diagnostic) between MAA and MNC was more than twice as large for externalizing disorders as it was for mood or anxiety disorders.
In the current study, we examine the same issues in older long-term abstinent alcoholics (OAA; mean age=69.3 years, mean abstinence=14.8 years) compared with age and gender-comparable older non-alcoholic controls (ONC). We compared the findings in OAA versus ONC to those we had previously reported in MAA versus MNC. Our central questions were: 1) whether there is increased psychiatric disorder in OAA vs. ONC, and 2) whether this disorder is different in pattern or magnitude from that seen in MAA versus MNC. Studying older alcoholics allows us to examine associations between abstinence duration and psychiatric comorbidity in individuals with even longer abstinence durations than was possible in MAA.
2. Methods
2.1 Participants
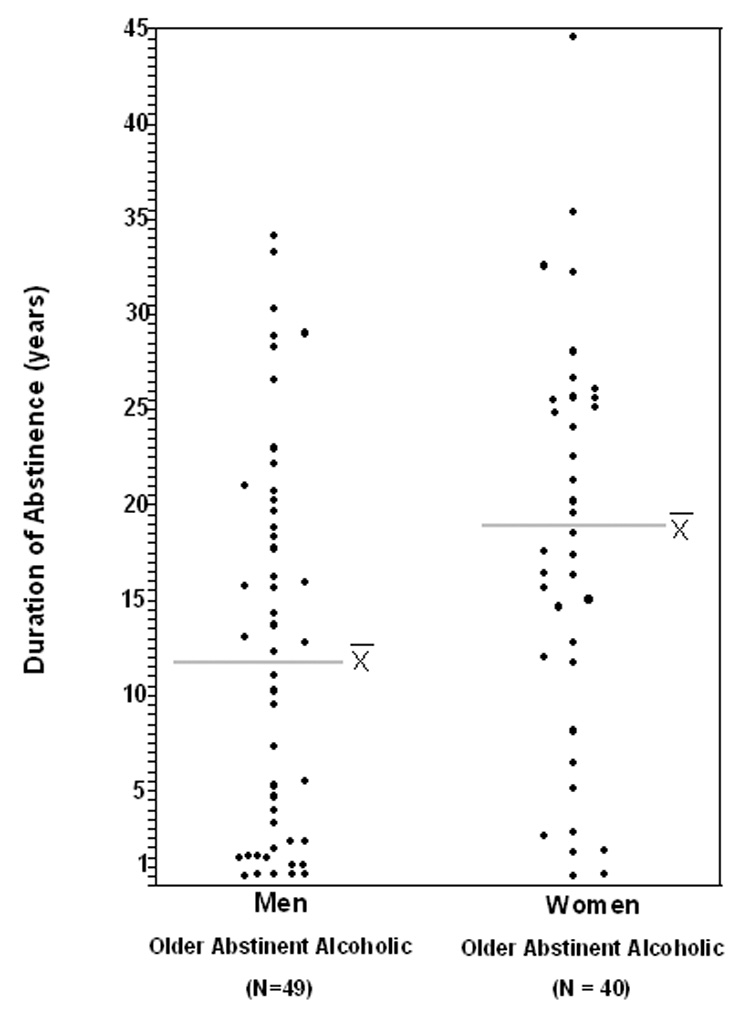
A total of 142 participants were recruited for the study from the San Francisco Bay Area community by postings at AA meetings, mailings, newspaper advertisements, a local Internet site, and participant referrals. The study consisted of two groups, OAA and ONC. The inclusion criteria for the OAA group were: 1) met lifetime DSM-IV (American Psychiatric Association, 2000) criteria for alcohol dependence, 2) had a lifetime drinking average of at least 100 standard drinks per month for men and 80 standard drinks per month for women, and 3) were abstinent for at least 6 months. A standard drink was defined as 12 ounces beer, 5 ounces wine, or 1.5 ounces liquor. The control group consisted of 24 men and 29 women, ranging in age from 60 to 85 years of age (mean = 69.3 years). The OAA group (n = 89) contained 49 men and 40 women, ranging from 60 to 85 years of age (mean = 67.5 years), abstinent from 6 months to 44 years (mean = 14.8 years). Figure 1 displays the distribution of abstinence duration for both genders. Although there is a slight skewing toward shorter abstinence durations, there is a good representation of abstinence durations across a large and comparable range for both men and women. The inclusion criteria for the ONC group was a lifetime drinking average of less than 30 standard drinks per month, with no periods of drinking more than 60 drinks per month.
Figure 1.
Exclusion criteria for both groups were: 1) lifetime or current diagnosis of schizophrenia or schizophreniform disorder (c-DIS) (Robins et al., 1998), 2) significant history of head trauma or cranial surgery, 3) history of significant neurological disease, 4) history of diabetes, stroke, or hypertension that required medical intervention, 5) laboratory evidence of hepatic disease, 6) clinical evidence of Wernicke-Korsakoff syndrome, or 7) history of drug abuse or dependence, other than nicotine or caffeine. (We excluded individuals with comorbid drug disorders so that we could ascribe differences between alcoholic and control samples to the effects of alcohol use without the confounding effects of drug abuse/dependence.)
The previously published study of MAA versus MNC employed exactly the same criteria and methods as this study of OAA versus ONC. The MAA group (n = 52) comprised 24 women and 28 men, ranging from 35 to 57 years of age (mean = 46.5 years), abstinent from 6 months to 21 years (mean = 6.3 years). The MNC consisted of 23 women and 25 men, ranging in age from 34 to 59 years of age (mean = 45.6 years). Table 1 presents the demographic and alcohol use measures for the OAA, ONC, MAA, and MNC groups.
Table 1.
Demographic and Alcohol Use Data for Older Abstinent Alcoholics and Controls
| Older, Long-term Abstinent Alcoholics | Older Normal Controls | Middle-Aged Abstinent Alcoholics | Middle-aged Normal Controls | Effect Size (%) b | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variables | Men (n=49) | Women (n=39) | Men (n=24) | Women (n=29) | Men (n=28) | Women (n=24) | Men (n=25) | Women (n=23) | Study × Group | Study |
| Demographics | ||||||||||
| Age (years) | 67.4 ± 5.4 | 67.7 ± 6.7 | 70.0 ± 6.3 | 68.7 ± 7.3 | 44.9 ± 6.9 | 48.4 ± 6.4 | 43.4 ± 6.3 | 48.0 ± 6.6 | 1.2 | -- |
| Year of Education Family History | 15.7 ± 2.8 | 15.5 ± 2.7 | 16.8 ± 2.4 | 15.9 ± 1.9 | 15.5 ± 1.9 | 15.5 ± 2.4 | 16.3 ± 2.2 | 16.0 ± 1.9 | 0 | -- |
| Density a | .263 ± .24 | .370 ± .29 | .087 ± .13 | .159 ± .19 | .395 ± .25 | .440 ± .29 | .142 ± .26 | .175 ± .21 | 0.5 | -- |
| Alcohol Use Variables | ||||||||||
| Age First Drank Alcohol | 17.6 ± 3.6 | 18.2 ± 4.0 | 24.6 ± 14.4 | 20.7 ± 4.9 | 14.8 ± 2.9 | 17.1 ± 5.6 | 18.8 ± 4.9 | 20.4 ± 4.9 | 0.2 | -- |
| Age at First Heavy Use | 28.7 ± 10.8 | 29.0 ± 7.9 | n/a | n/a | 21.5 ± 4.5 | 25.3 ± 7.6 | n/a | n/a | -- | 8.5*** |
| Alcohol Lifetime Duration (months) | 428.1 ± 121 | 369.3 ± 140 | 501.3 ± 209 | 519.9 ± 130 | 261.7 ± 93.7 | 277.1 ± 105 | 232.2 ± 130 | 294 ± 130 | 4.5*** | -- |
| Average Dose (drinks/month) | 185.7 ± 145 | 140.3 ± 86 | 8.97 ± 10.1 | 7.45 ± 7.85 | 177.3 ± 147 | 129.3 ± 77.5 | 6.91 ± 8.3 | 6.85 ± 7.6 | 0 | -- |
| Peak Duration (months) | 148 ± 131 | 77.3 ± 69.1 | 134.4 ± 177 | 103.7 ± 126 | 60.9 ± 57.8 | 92.3 ± 82.3 | 70.4 ± 80.7 | 113.8 ± 113 | 0 | -- |
| Peak Dose (drinks/month) | 341.3 ± 213 | 317 ± 243 | 21.3 ± 19 | 16.6 ± 13 | 339.7 ± 253 | 270.2 ± 201 | 15.1 ± 14.5 | 16.7 ± 22.4 | 0.1 | -- |
| Abstinence Duration (years) | 12.4 ± 10.2 | 17.7 ± 10.8 | n/a | n/a | 6.27 ± 6.1 | 6.29 ± 5.6 | n/a | n/a | -- | 18.1*** |
Measures are reported mean ± standard deviation.
Effect is significant:
p≤0.05
p≤0.01
p≤0.001
N/A: Not applicable
Proportion of 1st Degree Relative Problem Drinkers
Percent of variance of the dependent variable accounted for by the Study × Group effect for variables present in both alcoholic and control groups, and for the Study effect for variables present in the alcoholic groups only. Note that analyses are uncontrolled for multiple comparisons
2.2 Procedures
All participants were fully informed of the study’s procedures and aims, and signed a consent form prior to their participation. Participants completed four sessions that each lasted between an hour and a half and three hours, and included clinical, neuropsychological, electrophysiological, and neuroimaging assessments. A trained research associate administered these assessments to all participants. All participants completed all sessions. Non-alcoholic controls were asked to abstain from consuming alcohol for at least 24 hours prior to any lab visit. A Breathalyzer (Intoximeters, Inc., St. Louis, MO) test was administered to all participants. A 0.000 alcohol concentration was required of all participants in all sessions. Participants were compensated for their time and travel expenses upon completion of each session. Participants who completed the entire study were also given a completion bonus.
2.2.1 Alcohol Use Measures
In the first session (the clinical evaluation session), participants were interviewed on their lifetime drug and alcohol use using a timeline follow-back assessment. (Skinner and Allen, 1982; Skinner and Sheu, 1982; Sobell et al., 1988; Sobell and Sobell, 1992).
2.2.2 Family History of Alcoholism
The Family Drinking Questionnaire was administered based on the methodology of Mann et al. (Mann et al., 1985; Stoltenberg et al., 1998). The questionnaire asked participants to rate the members of their family as being alcohol abstainers, alcohol users with no problem, or problem drinkers. Individuals were family history positive for alcoholism (FHP) if they had at least one first-degree relative who was a problem drinker, and the density of the family history of alcoholism (FHD) was defined as the proportion of first-degree relatives that were problem drinkers.
2.2.3 Psychiatric Diagnoses, Symptom Counts, and Psychological Measures of Psychiatric Disorder
For each domain, we assessed diagnoses and symptom counts using the c-DIS, and assessed the psychological substrate of psychiatric illness using specific psychological measures. Psychological measures used to assess anxiety were the Reiss-Epstein Anxiety Sensitivity Index (ASI) (Reiss et al., 1986), and the State and Trait Scales of the State-Trait Anxiety Inventory for Adults (STAI-S and STAI-T) (Spielberger, 1983). Anxiety disorder symptom counts on the c-DIS were summed across the diagnostic categories of social phobia, agoraphobia, panic disorder, post-traumatic stress syndrome, obsessive disorder, and compulsive disorder. Lifetime and current anxiety disorder diagnoses (across these same categories) were also determined.
Psychological measures used to assess mood were the Depression and Hypomania Scales of the Minnesota Multiphasic Personality Inventory-2 (MMPI-D and MMPI-H) (Hathaway and McKinley, 1989). Mood disorder symptoms on the c-DIS were summed across the diagnostic categories of depression, dysthymia, and mania. Lifetime and current mood disorder diagnoses were also determined.
Psychological measures used to assess the externalizing domain were the Socialization Scale of the California Psychological Inventory (CPI-SS) (Gough, 1969), and the Psychopathic Deviance Scale of the MMPI-2 (MMPI-PD) (Hathaway and McKinley, 1989). Externalizing disorder symptoms on the c-DIS were summed across the diagnostic categories of conduct disorder and antisocial personality disorder (ASPD). Lifetime and current externalizing disorder diagnoses were also determined.
2.3 Statistical Analysis
The data were analyzed using the Statistical Package for the Social Sciences (SPSS Inc., 2004). We compared diagnosis rates between groups using continuity corrected chi-square tests for rates of any psychiatric diagnosis and on diagnosis rates for mood, anxiety, or externalizing disorders. These comparisons were performed separately for lifetime and current diagnoses. In the analysis of current diagnoses (last 12 months), we removed all OAA with less than 18 months of abstinence, so that diagnoses during the period of drinking and the first six months of abstinence would not be included (this is the same procedure we used in the analyses of the MAA data). Symptom counts and psychological measures were analyzed by ANOVA, with group and gender as main effects. We computed the effect size measure (percent of variance of the dependent variable accounted for by the independent variable) to facilitate comparisons of effects across measures and between the OAA study and the MAA study.
Finally, the data from OAA and ONC were compared with the data we previously published on MAA and MNC. Regarding diagnosis rates, we tested for homogeneity of the twoby-two table of group by diagnosis (separately for lifetime and current diagnoses) across studies (separately for any diagnosis, or for mood, anxiety, or externalizing diagnoses). If the homogeneity test was significant, we tested whether the group difference differed between the two studies. For each group within each study, the rate of psychiatric disorder is given. The standard deviation of those rates is estimated as sqrt (pq/n). Using the nomenclature that M or O denotes middle-aged or older, and A or C denotes alcoholic and control, we tested the hypothesis that the diagnosis rates for (MAA-MNC) = (OAA-ONC), or (MAA-MNC) – (OAA-ONC) = 0. If D = (MAA-MNC) – (OAA-ONC), then we computed the rate for D, the std(D), converted D to z and computed the probability that z > 0. Regarding analysis of continuous variables (symptom counts and psychological measures), we concatenated the data from the two studies and performed ANOVAs. Differences in the effect of alcoholism in the older versus middle-aged studies would manifest as a significant group (abstinent alcoholic versus control) by study (older versus middle-aged) interaction effects. Analyses of associations with psychiatric measures were uncorrected for multiple comparisons because the number of demographic and alcohol use variables was so large. These analyses were performed to generate hypotheses for further study
3. Results
3.1 Demographic and Alcohol Use Variables
As noted, Table 1 above presents the demographic and alcohol use measures for the OAA, ONC, MAA, and MNC groups. The OAA and MAA did not differ on either the average monthly alcohol dose or on the peak monthly alcohol dose, suggesting rough comparability in the severity of alcoholism. OAA started heavy use later than MAA, consistent with changing societal norms.
3.2 OAA versus ONC
3.2.1 Prevalence of Lifetime and Current Psychiatric Diagnoses
Over half of the OAA (46 of 89 = 51.7%) compared with less than one third of ONC (13 of 53 = 30.2%) had a lifetime psychiatric diagnosis (χ2 = 5.40, p < .02). There was also a trend for a greater percentage of lifetime mood diagnoses in the OAA versus ONC (40 of 89 = 44.9% versus 15 of 53 = 28.3%; χ2 = 3.21, p = .07), but no differences between groups in the proportions of individuals with lifetime anxiety or externalizing disorder diagnoses. There was no difference between OAA and ONC (4.5% versus 3.8%) in current psychiatric diagnoses.
3.2.2 Lifetime Psychiatric Symptom Counts
Table 2 presents the data for lifetime psychiatric symptom counts and current psychological measures of individuals’ disposition toward anxiety, depression, hypomania, and deviance proneness. We first examined symptoms aggregated over all three domains (mood, anxiety, and externalizing). OAA had 77% more psychiatric symptoms than ONC (F1,138 = 20.66, p ≪ 0.0001, effect size = 13.0 %), with a trend toward women having more symptoms than men (F1,138 = 3.13, p = 0.08, effect size = 2.2 %). Examining the three domains separately, OAA had over 50% more lifetime anxiety symptoms than ONC (p = 0.01, effect size = 4.4 %), there was a trend for women to have more anxiety symptoms than men (p = 0.09, effect size = 2.1 %). OAA had almost 50% more lifetime mood symptoms than ONC (p = 0.02, effect size = 3.8%), and women had 80% more mood symptoms than men (p = 0.001, effect size =7.2 %), with no group by gender interaction. OAA had over 2.5 times the number of lifetime externalizing symptoms as did ONC (p ≪ 0.0001, effect size = 22.2 %), and men had over 50% more lifetime externalizing symptoms than women (p = 0.008, effect size = 5.0 %). There were no group by gender interactions for any of the symptom count measures.
Table 2.
Psychological Measures and Psychiatric Symptom Counts
| Older, Long-term Abstinent Alcohol | Older Normal Controls | Middle-Aged Abstinent Alcoholics | Middle-aged Normal Controls | Effect Size (%)b | |||||
|---|---|---|---|---|---|---|---|---|---|
| Variables | Men (n=49) | Women (n=40) | Men (n=24) | Women (n=29) | Men (n=28) | Women (n=24) | Men (n=25) | Women (n=23) | |
| Total Psychiatric Sx a | 25.1 ± 19.0 | 30.0 ± 14.4 | 12.8 ± 10.1 | 17.5 ± 14.7 | 46.5 ± 23.6 | 43.9 ± 25.2 | 13.8± 12.7 | 21.3 ± 18.1 | 4.2** |
| Anxiety | |||||||||
| Anxiety Sx a | 8.12 ± 8.8 | 9.87 ± 9.1 | 3.96 ± 3.9 | 7.00 ± 7.4 | 14.7 ± 13.0 | 14.9 ± 13.3 | 3.28 ± 4.3 | 7.91 ± 8.7 | 2.3** |
| ASI | 20.9 ± 11.2 | 19.8 ± 8.9 | 13.3 ± 9.4 | 15.0 ± 10.1 | 20.1 ± 11.9 | 21.7 ± 13.5 | 12.9 ± 8.8 | 14.6 ± 11.7 | 0.1 |
| STAI-S | 29.9 ± 8.8 | 26.8 ± 5.0 | 26.7 ± 5.6 | 26.9 ± 6.0 | 31.9 ± 10.9 | 32.2 ± 6.8 | 28.0 ± 9.9 | 26.3 ± 7.5 | 1.1 |
| STAI-T | 35.0 ± 9.5 | 33.0 ± 7.1 | 32.3 ± 7.3 | 33.5 ± 8.7 | 41.1 ± 10.9 | 41.5 ± 10.4 | 33.6 ± 8.3 | 33.1 ± 9.5 | 3.4** |
| Mood | |||||||||
| Mood Sx a | 6.7 ± 8.7 | 12.5 ± 8.2 | 4.3 ± 6.2 | 8.0 ± 9.8 | 16.8 ± 12.7 | 18.3 ± 14.8 | 4.56 ± 7.4 | 10.4 ± 9.4 | 2.7** |
| MMPI-D | 19.8 ± 5.3 | 19.2 ± 3.7 | 19.3 ± 3.8 | 19.6 ± 4.4 | 22.8 ± 6.9 | 24.2 ± 7.1 | 18.0 ± 4.1 | 18.9 ± 5.1 | 5.4*** |
| MMPI-H | 16.9 ± 4.1 | 17.8 ± 4.0 | 14.7 ± 4.6 | 15.3 ± 5.3 | 19.9 ± 5.5 | 16.0 ± 4.2 | 15.6 ± 3.7 | 15.4 ± 4.1 | 0 |
| Externalizing | |||||||||
| Externalizing Sx a | 10.3 ± 6.3 | 7.65 ± 5.1 | 4.54 ± 3.5 | 2.48 ± 2.7 | 15.1 ± 7.9 | 10.8 ± 7.0 | 6.00 ± 5.5 | 2.96 ± 3.2 | 1.7** |
| CPI-SS | 32.3 ± 4.1 | 33.2 ± 4.1 | 35.9 ± 4.4 | 37.7 ± 3.7 | 27.4 ± 5.7 | 29.8 ± 5.9 | 36.2 ± 4.0 | 36.3 ± 4.0 | 3.7** |
| MMPI-PD | 17.7 ± 4.4 | 16.9 ± 2.7 | 14.7 ± 2.9 | 14.6 ± 3.9 | 21.8 ± 4.2 | 21.5 ± 3.8 | 16.7 ± 3.0 | 16.2 ± 3.3 | 2.9** |
Measure scores are reported mean ± standard deviation
Effect is significant:
p≤0.05
p≤0.01
p≤0.001
Lifetime symptoms
Percent of variance of the dependent variable accounted for by the Study × Group effect. Note that analyses are uncontrolled for multiple comparisons
3.2.3 Current Psychological Measures of Mood, Anxiety, and Externalizing Disorder
We also compared OAA with ONC in terms of current psychological measures. In the anxiety domain, OAA had higher ASI Scores than ONC (F1,138 = 12.45, p = 0.001, effect size = 8.3 %), but did not differ from ONC on either the STAI State or Trait Anxiety scales, with no gender or group by gender effects for any measure. In the mood domain, OAA had higher MMPI Hypomania Scale Scores than ONC (F1,138 = 9.19, p = 0.003, effect size = 6.2 %), but did not differ from ONC on MMPI Depression Scale Scores (F1,138 = 0.004, ns, effect size = 0.0%), with no gender or group by gender effects for either measure. With regard to deviance proneness psychological measures, OAA had higher MMPI Psychopathic Deviance Scale Scores than ONC (F1,138 = 17.02, p ≪ 0.0001, effect size = 11.0 %), and were less socialized than ONC using the CPI Socialization Scale (F1,138 = 32.68, p ≪ 0.0001, effect size = 19.1%), with women tending to be more socialized than men (F1,138 = 3.46, p = 0.065, effect size = 2.4%), and with no other gender or group by gender effects.
3.2.4 Association of Psychological and Psychiatric Measures with Alcohol Use Variables
There were no differences between OAA with versus without a lifetime psychiatric diagnosis on any demographic or alcohol use variable. However, there were a number of statistically significant associations between the psychiatric and psychological measures and the demographic and alcohol use variables. Within OAA, individuals with more years of education had higher scores on the CPI Socialization scale (r = 0.22, p = 0.03). More mood symptoms were associated with a shorter duration of active drinking (r = − 0.26, p = .01), more anxiety symptoms were associated with higher peak alcohol doses (r = 0.23, p = 0.03), and more externalizing symptoms were associated with a higher average alcohol dose (r = 0.32, p = 0.004), and starting heavy drinking at an earlier age (r = − 0.32, p = 0.002). There was also a negative association of scores on the MMPI Depression scale with alcohol abstinence duration and a corresponding positive association with duration of alcohol use (r = − 0.23, and r = 0.24, both p’s < .05). In the anxiety disorder domain, higher state anxiety scores on the STAI were associated with having one’s first drink at an earlier age (r = − 0.29, p = 0.005), and having drank for a longer period of time (r = 0.22, p = 0.04). Higher ASI scores were also associated with having drank for a longer period of time (r = 0.22, p = 0.04), and were also associated with a higher dose at first heavy use (r = 0.21, p = 0.04). These correlations should be viewed cautiously because they were not corrected for multiple comparisons.
3.3 ONC versus MNC (Older versus Middle-Aged Cohort Differences)
We carefully examined cohort differences by comparing ONC with MNC. There was a trend toward fewer lifetime psychiatric diagnoses in ONC versus MNC (χ2 = 3.3, p = .07), but no differences in current diagnoses or in the prevalence of diagnoses in any domain (all p’s > 0.30). There were lower scores on the MMPI Psychopathic Deviance Scale in ONC versus MNC. (F1,97 = 7.16, p = 0.009). With respect to all other symptom counts and psychological measures, the control groups were comparable (all p’s > 0.20).
3.4 OAA versus ONC compared with MAA versus MNC
3.4.1 Prevalence of Lifetime or Current Psychiatric Diagnoses
For lifetime diagnoses, the 2x2 tables for the two studies were dissimilar for any psychiatric diagnosis, anxiety, mood, or externalizing disorder diagnoses (all χ2 (3 df) > 10.9, p’s < 0.01). The difference in lifetime diagnosis rates between abstinent alcoholics and controls was smaller in the older compared with the middle-aged studies for anxiety (z = 1.75, p = 0.04) and externalizing disorder diagnoses (z = 1.86, p = 0.03), but not for any psychiatric diagnosis or mood disorder diagnoses.
For current diagnoses, the 2×2 tables for the two studies were dissimilar for any psychiatric diagnosis, anxiety, or mood disorder diagnoses (all χ2 (3 df) > 14.7, p’s < 0.002). The difference in current diagnosis rates between abstinent alcoholics and controls was smaller in the older compared with the middle-aged studies for any psychiatric diagnosis(z = 3.78, p < 0.001), anxiety diagnoses (z = 2.97, p < 0.002), and mood disorder diagnoses (z = 2.93, p < 0.002). There were no current externalizing disorder diagnoses in any of the four groups: OAA, ONC, MAA, or MNC; thus, there were no differences between groups or across studies.
3.4.2 Lifetime Psychiatric Symptom Counts
The comparison between the middle-aged and older study for symptom counts and psychological measures of psychiatric disorder are presented in Table 2. There was a smaller group (alcoholic versus control) difference for the OAA compared with the MAA study when lifetime psychiatric symptoms were summed across all three domains (i.e., the group by study effect; F1,234 = 10.73, p = 0.002, effect size = 4.2 %), with no study by gender, or group by study by gender effects (all p’s > 0.27). The OAA were also less different from their controls than were the MAA from their controls for lifetime symptoms in each domain (p’s ≤ 0.04, effect sizes ≤ 2.7%), with no study by gender or group by study by gender effects (all p’s > 0.21).
3.4.3 Current Psychological Measures of Mood, Anxiety, and Deviance Proneness
OAA were less different from ONC than were MAA from MNC on the STAI Trait Anxiety Scale (F1,234 = 8.21, p = 0.005, effect size = 3.4%), but did not differ from ONC on the STAI State Anxiety Scale or on the ASI (F1,234 = 0.12, p = 0.73 and F1,234 = 2.52, p = 0.11, effect sizes < 1.1%). OAA were less different from ONC than were MAA from MNC on the MMPI Depression Scale (F1,234 = 13.27, p < 0.0001, effect size = 5.4%), but did not differ in from ONC on the MMPI Hypomania Scale (p > 0.90, effect size = 0.0%). OAA were also less different from ONC than were MAA from MNC on both the MMPI Psychopathic Deviance Scale (F1,234 = 7.06, p = 0.008, effect size = 2.9%), and the CPI Socialization Scale (F1,234 = 9.05, p = 0.003, effect size = 3.7%).
4. Discussion
The sample size of the current study is small in terms of estimating rates of specific comorbid psychiatric disorders, but large in comparison to the extant data on long-term abstinence in older alcoholics. The samples were more than adequate to demonstrate that psychiatric disorders are more prevalent in OAA than ONC, and that psychiatric comorbidity is less in OAA compared with ONC versus MAA compared with MNC.
The findings on psychiatric disorder in OAA compared with ONC shows both a number of similarities as well as a number of important differences from our earlier findings on psychiatric disorder in MAA compared with MNC. MAA compared with MNC versus OAA compared with ONC were similar in the following ways: 1) both studies showed more lifetime psychiatric diagnoses in alcoholics than controls, 2) both studies showed higher lifetime symptom counts in all three psychiatric domains assessed (anxiety, mood, and externalizing disorders) in alcoholics than controls, 3) both groups of alcoholics showed some evidence of psychological abnormality in all three domains, and 4) in both studies there were dramatically larger differences between alcoholics and controls in the externalizing versus the mood and anxiety domains.
Overall, the OAA were less different from ONC than were MAA from MNC. Moreover, in the MAA, there was an increased prevalence of lifetime diagnoses versus controls in all three psychiatric domains: mood, anxiety, and externalizing disorders. (In the OAA versus ONC, a trend for increased prevalence was evident only for mood diagnoses.) Less than 5% of OAA had a current psychiatric diagnosis, compared with current diagnoses in about 50% of MAA. The lesser psychiatric disorder in the OAA vs. ONC compared with MAA vs. MNC was also evident in lifetime symptom counts in each domain, and on at least one psychological test in each domain.
The interpretation of the smaller effect sizes between abstinent alcoholics and controls in the OAA versus MAA studies is not obvious. There is the possibility that psychiatric disorder makes maintaining abstinence difficult as one ages, so that the rate of relapse in psychiatrically impaired alcoholics increases with age. That interpretation would be consistent with our findings. However, significant caution is warranted before subscribing to this interpretation. First, there was no association within the OAA (or within MAA (Di Sclafani et al., 2007; Fein et al., 2007)) of abstinence duration with psychiatric disorder measures. In the middle-aged study, we concluded that alcoholics were able to maintain abstinence in the presence of ongoing psychiatric illness (in the presence of a current diagnosis). In this study of older alcoholics, less than five percent of participants had a current psychiatric diagnosis; therefore we cannot come to the same conclusion.
There are a number of factors that may have contributed to the lower prevalence and severity of psychiatric disorder in the OAA compared with MAA. First, selective survivorship may be a factor. Although selection bias is almost unavoidable in clinical studies of samples of any age, it may be more of an issue in older samples. Heavy alcohol consumption has been shown to negatively impact life expectancy both directly and indirectly (Ojesjo et al., 1998; Jarque-Lopez et al., 2001; Goldacre et al., 2004; Sher, 2005; Wojtyniak et al., 2005; Rehm et al., 2006). It is also possible that the alcoholics who survived into their sixties, seventies, and eighties and volunteer for demanding research studies are also the physically healthier individuals. This would reduce psychiatric comorbidity in the OAA sample, since psychiatric and physical health are related, especially in older populations (Haug, et. al., 2004; Braam, et. al., 2005; Kisely & Simon, 2006; Ng, et. al., 2006; Copsey Spring, et. al., 2007). However, if this type of selection bias is present in the current study, our results underestimate psychiatric comorbidity in OAA, strengthening our finding of psychiatric disorder in OAA compared with ONC.
There were also cohort differences that may have contributed to the differences between the OAA and MAA findings. There was a trend toward lesser scores on ‘externalizing’ psychological scales and fewer lifetime externalizing symptoms in ONC compared with MNC. This may be due to societal values that were present during the youth and middle-age of the older cohort, especially norms that frowned upon the expression and acceptance of abnormal behaviors, especially antisocial behaviors. For instance, the rates of illegitimate births (National Center for Health Statistics, 1993a) and divorce (National Center for Health Statistics, 1993b) for the older cohort were about half that for the middle-aged cohort. Older cohorts also had dramatically reduced rates of adolescents and young adults arrested for any crime, or for violent crime among juveniles (Federal Bureau of Investigation, 1993).
In summary, we want to emphasize that psychiatric disorder in OAA, while less than that in MAA, is still higher than in ONC. This is true for lifetime diagnoses, lifetime symptom counts, and abnormal psychological measures of anxiety sensitivity, hypomania, socialization, and deviance proneness. The fact that these differences are present in this sample of older individuals, who are abstinent an average of 15 years, is a testament to the very strong association of psychiatric and psychological disturbance with chronic alcoholism. The OAA results are in concordance with the MAA results in showing that the bulk of psychiatric disorder in the long-term abstinent alcoholics is subdiagnostic. Finally, the results in both OAA and MAA vis-à-vis the greater magnitude of externalizing compared with mood and anxiety abnormalities is concordant with the alcohol research literature, (Iacono et al., 1999; Chassin et al., 1999; Blum et al., 2000; Mazas et al, 2000; Flory and Lynam, 2003; Krueger et al., 2005; Markon and Krueger, 2005) emphasizing the central role of externalizing disorders in alcoholism.
Acknowledgements
We’d like to express our appreciation to each of our volunteer research participants, and to the NRI recruitment and assessment staff.
This work was supported by NIAAA grant # AA11311, “Effects of Alcohol Abuse on the Aging Brain”.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association. DSM-IV-R: Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, D.C: American Psychiatric Publishing; 2000. [Google Scholar]
- Blum K, Braverman ER, Holder JM, Lubar JF, Monastra VJ, Miller D, Lubar JO, Chen TJ, Comings DE. Reward deficiency syndrome: A biogenetic model for the diagnosis and treatment of impulsive, addictive, and compulsive behaviors. Journal of Psychoactive Drugs. 2000;32:1–112. doi: 10.1080/02791072.2000.10736099. [DOI] [PubMed] [Google Scholar]
- Braam AW, Prince MJ, Beckman AT, Delesaul P, Dewey ME, Geerlings SW, Kivela Sl, Lawlor BA, Magnusson H, Meller I, Peres K, Reischies FM, Roelands M, Schoevers RA, Saz P, Skoog I, Turrina C, Versporten A, Copelan JR. Physical health and depressive symptoms in older Europeans. Results from EURODEP. British Journal of Psychiatry. 2005;187:35–42. doi: 10.1192/bjp.187.1.35. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control. Alcohol-attributal deaths and years of potential life lost-United States, 2001. MMWR Morbidity and Mortality Weekly Report. 2004;53:866–870. [PubMed] [Google Scholar]
- Chassin L, Pitts SC, DeLucia C, Todd M. A longitudinal study of children of alcoholics: Predicting young adult substance use disorders, anxiety, and depression. Journal of Abnormal Psychology. 1999;108:106–119. doi: 10.1037//0021-843x.108.1.106. [DOI] [PubMed] [Google Scholar]
- Copsey Spring TR, Yanni LM, Levenson JL. A shot in the dark: Failing to recognize the link between physical and mental illness. Journal of General Internal Medicine. 2007;22:677–680. doi: 10.1007/s11606-006-0089-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Sclafani V, Finn P, Fein G. Psychiatric comorbidity in long-term abstinent alcoholic individuals. Alcoholism: Clinical and Experimental Research. 2007;31:795–803. doi: 10.1111/j.1530-0277.2007.00361.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fein G, Di Sclafani V. Cerebral reserve capacity: Implications for alcohol and drug abuse. Alcohol. 2004;32:63–67. doi: 10.1016/j.alcohol.2003.10.003. [DOI] [PubMed] [Google Scholar]
- Fein G, Di Sclafani V, Finn P, Scheiner DL. Sub-diagnostic psychiatric comorbidity in alcoholics. Drug and Alcohol Dependence. 2007;87:139–145. doi: 10.1016/j.drugalcdep.2006.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fein G, McGillivray S. Cognitive performance in long-term abstinent elderly alcoholics. Alcoholism: Clinical and Experimental Research. 2007;31:1788–1799. doi: 10.1111/j.1530-0277.2007.00481.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flory K, Lynam DR. The relation between attention deficit hyperactivity disorder and substance abuse: what role does conduct disorder play? Clinical Child and Family Psychology Review. 2003;6:1–16. doi: 10.1023/a:1022260221570. [DOI] [PubMed] [Google Scholar]
- Goldacre MJ, Duncan M, Griffith M, Cook-Mozaffari P. Alcohol as a certified cause of death in a ‘middle England’ population 1979–1999: Database study. Journal of Public Health (Oxford) 2004;26:343–346. doi: 10.1093/pubmed/fdh183. [DOI] [PubMed] [Google Scholar]
- Gough HGPD. Manual for the California Psychological Inventory (So Scale) Palo Alto, CA: Consulting Psychological Press; 1969. [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Pickering RP, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2004a;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Ruan WJ, Pickering RP. Co-occurrence of 12-month alcohol and drug use disorders and personality disorders in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2004b;61:361–368. doi: 10.1001/archpsyc.61.4.361. [DOI] [PubMed] [Google Scholar]
- Hathaway S, McKinley J. MMPI-2: Minnesota Multiphasic Personality Inventory. Minneapolis, MN: University of Minnesota Press; 1989. [Google Scholar]
- Haug TT, Mykletun A, Dahl AA. The association between anxiety, depression, and somatic symptoms in a large population: The HUNT-II study. Psychosomatic Medicine. 2004;66:845–851. doi: 10.1097/01.psy.0000145823.85658.0c. [DOI] [PubMed] [Google Scholar]
- Helzer JE, Pryzbeck TR. The co-occurrence of alcoholism with other psychiatric disorders in the general population and its impact on treatment. Journal of Studies on Alcohol. 1988;49:219–224. doi: 10.15288/jsa.1988.49.219. [DOI] [PubMed] [Google Scholar]
- Iacono WG, Carlson SR, Taylor J, Elkins IJ, McGue M. Behavioral disinhibition and the development of substance-use disorders: Findings from the Minnesota Twin Family Study. Developmental Psychopathology. 1999;11:869–900. doi: 10.1017/s0954579499002369. [DOI] [PubMed] [Google Scholar]
- Jarque-Lopez A, Gonzalez-Reimers E, Rodrigues-Moreno F, Santolaria-Fernandez F, Lopez-Lirola A, Ros-Vilamajo R, Espinosa-Villarreal JG, Martinez-Riera A. Prevalence and mortality of heavy drinkers in a general medical hospital unit. Alcohol. 2001;36:335–338. doi: 10.1093/alcalc/36.4.335. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Crum RM, Warner LA, Nelson CB, Schulenberg J, Anthony JC. Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Archives of General Psychiatry. 1997;54:313–321. doi: 10.1001/archpsyc.1997.01830160031005. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Nelson CB, McGonagle KA, Edlund MJ, Frank RG, Leaf PJ. The epidemiology of co-occurring addictive and mental disorders. American Journal of Orthopsychiatry. 1996;66:17–31. doi: 10.1037/h0080151. [DOI] [PubMed] [Google Scholar]
- Kisely S, Simon G. An international study comparing the effect of medically explained and unexplained somatic symptoms on psychosocial outcome. Journal of Psychosomatic Research. 2006;60:125–130. doi: 10.1016/j.jpsychores.2005.06.064. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Markon KE, Patrick CJ, Iacono WG. Externalizing psychopathology in adulthood: A dimensional-spectrum conceptualization and its implications for DSM-V. J Abnormal Psychology. 2005;114:537–550. doi: 10.1037/0021-843X.114.4.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann RE, Sobell LC, Sobell MB, Pavan D. Reliability of a family tree questionnaire for assessing family history of alcohol problems. Drug and Alcohol Dependence. 1985;15:61–67. doi: 10.1016/0376-8716(85)90030-4. [DOI] [PubMed] [Google Scholar]
- Markon KE, Krueger RF. Categorical and continuous models of liability to externalizing disorders: a direct comparison in NESARC. Archives of General Psychiatry. 2005;62:1352–1359. doi: 10.1001/archpsyc.62.12.1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazas CA, Finn PR, Steinmetz JE. Decision-making biases, antisocial personality, and early-onset alcoholism. Alcoholism: Clinical and Experimental Research. 2000;24:1036–1040. [PubMed] [Google Scholar]
- Merikangas KR, Mehta RL, Molnar BE, Walters EE, Swendsen JD, Aguillar-Gaziola S, Bijl R, Borges G, Caraveo-Anduaga JJ, DeWit DJ, Kolody B, Vegas WA, Wittchen HU, Kessler RC. Comorbidity of substance use disorders with mood and anxiety disorder: Results of the International Consortium in Psychiatric Epidemiology. Addictive Behaviors. 1998;23:893–907. doi: 10.1016/s0306-4603(98)00076-8. [DOI] [PubMed] [Google Scholar]
- Ng TP, Feng L, Chiam PC, Kua EH. Psychiatric morbidity and acute hospitalization in elderly people. International Psychogeriatrics. 2006;18:701–711. doi: 10.1017/S1041610206003346. [DOI] [PubMed] [Google Scholar]
- Ojesjo L, Hagnell O, Otterbeck L. Mortality in alcoholism among men in the Lundby Community Cohort, Sweden: a forty-year follow-up. Journal of Studies on Alcohol. 1998;59:140–145. doi: 10.15288/jsa.1998.59.140. [DOI] [PubMed] [Google Scholar]
- Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, Goodwin FK. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. Journal of the American Medical Association. 1990;264:2511–2518. [PubMed] [Google Scholar]
- Rehm J, Patra J, Popova S. Alcohol-attributable mortality and potential years of life lost in Canada 2001: Implications for prevention and policy. Addiction. 2006;101:373–384. doi: 10.1111/j.1360-0443.2005.01338.x. [DOI] [PubMed] [Google Scholar]
- Reiss S, Peterson RA, Gursky DM, McNally RJ. Anxiety sensitivity, anxiety frequency and the prediction of fearfulness. Behaviour Research and Therapy. 1986;24:1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- Robins LN, Cottler L, Buckholz K, Compton W. The Diagnostic Interview Schedule for DSM-IV. St. Louis, MO: Washington University School of Medicine; 1998. [Google Scholar]
- Sher L. Alcohol use and suicide rates. Medical Hypotheses. 2005;65:1010–1012. doi: 10.1016/j.mehy.2005.07.003. [DOI] [PubMed] [Google Scholar]
- Skinner HA, Allen BA. Alcohol dependence syndrome: Measurement and validation. Journal of Abnormal Psychology. 1982;91:199–209. doi: 10.1037//0021-843x.91.3.199. [DOI] [PubMed] [Google Scholar]
- Skinner HA, Sheu WJ. Reliability of alcohol use indices. The Lifetime Drinking History and the MAST. Journal of Studies on Alcohol. 1982;43:1157–1170. doi: 10.15288/jsa.1982.43.1157. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline Follow-back: A technique for assessing self-reported alcohol consumption. In: Allen J, Litten RZ, editors. Measuring Alcohol consumption: Psychosocial and Biochemical Methods. Totowa, N.J: Humana Press; 1992. [Google Scholar]
- Sobell LC, Sobell MB, Riley DM, Schuller R, Pavan DS, Cancilla A, Klajner F, Leo GI. The reliability of alcohol abusers’ self-reports of drinking and life events that occurred in the distant past. Journal of Studies on Alcohol. 1988;49:225–232. doi: 10.15288/jsa.1988.49.225. [DOI] [PubMed] [Google Scholar]
- Spielberger CD. State-Trait Anxiety Inventory for Adults: Form Y Review Set – Manual, Test, Scoring Key. Redwood City, CA: Mind Garden, Inc; 1983. [Google Scholar]
- SPSS Inc. SPSS 13.0 for Windows. 13.0 ed. Chicago, IL: SPSS Inc; 2004. [Google Scholar]
- Stoltenberg SF, Mudd SA, Blow FC, Hill EM. Evaluating measures of family history of alcoholism: Density versus dichotomy. Addiction. 1998;93:1511–1520. doi: 10.1046/j.1360-0443.1998.931015117.x. [DOI] [PubMed] [Google Scholar]
- Tomasson K, Vaglum P. A nationwide representative sample of treatment-seeking alcoholics: a study of psychiatric comorbidity. Acta Psychiatrica. 1995;92:378–385. doi: 10.1111/j.1600-0447.1995.tb09600.x. [DOI] [PubMed] [Google Scholar]
- Wojtyniak B, Moskalewicz J, Stokwiszewski J, Rabczenko D. Gender-specific mortality associated with alcohol consumption in Poland in transition. Addiction. 2005;100:1779–1789. doi: 10.1111/j.1360-0443.2005.01247.x. [DOI] [PubMed] [Google Scholar]


