Abstract
The purpose of this study was to investigate the impact of the Request for Proposal (RFP) process – specifically, the profit status of provider agencies awarded contracts, the service volume awarded and contract duration – on the quality of home care services and outcomes. A cross-sectional (contract characteristics) and repeated measures (clients) design was used to collect data on the study variables. Primary data were collected in 2002–2003 from 11 Community Care Access Centres (CCACs) and 11 nursing provider agencies in Ontario. The sample included 750 home care clients recruited consecutively from home care referrals. Follow-up assessments were completed on 498 clients. CCACs and provider agencies completed written questionnaires about profit status, contract volume, duration of contract, potential for renewal, number of visits made by a principal nurse and number of visits made by a registered nurse. Data were collected on client health outcomes either at admission to home care service for new clients or at entry to the study for long-term clients, and then at discharge from service or at the end of six weeks, whichever came first, using the eight subscales of the Medical Outcome Study SF-36. Analysis was conducted using hierarchical linear modelling.
For the most part, contract characteristics were not related to the consistency of principal nurse visits or client outcomes. Where differences existed, they were small. Clients of agencies awarded longer contracts received greater consistency in principal nurse visits than clients of agencies awarded shorter contracts. Clients cared for by for-profit agencies reported slightly higher satisfaction with care and better mental health outcomes than clients cared for by not-for-profit agencies. The percentage of visits made by a registered nurse was positively associated with social function outcome for clients at follow-up. In conclusion, the study findings suggest that contract characteristic variables had a small effect on home care client outcomes.
Abstract
Cette étude avait pour but d’examiner l’incidence du processus de demande de propositions (DP) – plus précisément, le statut à but lucratif des organismes fournisseurs de services qui ont obtenu des contrats, le volume de service octroyé et la durée des contrats – sur la qualité des services fournis aux récipiendaires de soins à domicile et les résultats. On a eu recours à une conception axée sur des mesures transversales (caractéristiques des contrats) et répétées (clients) pour recueillir des données sur les variables de l’étude. Des données primaires ont été recueillies en 2002–2003 auprès de 11 centres d’accès aux soins communautaires (CASC) et 11 fournisseurs de soins infir-miers en Ontario. L’échantillon comprenait 750 bénéficiaires de soins à domicile recrutés de manière consécutive à partir d’aiguillages vers des soins à domicile. Des évaluations de suivi ont été effectuées pour 498 clients. Les CASC et les orga-nismes fournisseurs de services ont rempli des questionnaires écrits sur leur statut d’organismes à but lucratif, le volume de contrats, la durée des contrats, le potentiel de renouvellement, le nombre de visites effectuées par une infirmière principale et le nombre de visites effectuées par une infirmière autorisée. À l’aide des huit sous-échelles de la Medical Outcome Study SF-36, des données ont été recueillies sur les résultats des clients en matière de santé soit au moment de l’admission aux services de soins à domicile pour les nouveaux clients, soit au moment du début de la participation à l’étude pour les clients à long terme, puis à la fin des services ou après six semaines, selon la première éventualité. Une analyse a été effectuée en utilisant une modélisation linéaire hiérarchique.
La plupart des variables dans les caractéristiques des contrats n’étaient pas liées à la régularité des visites des infirmières principales ou aux résultats des clients. Là où il y avait des différences, celles-ci étaient faibles. Les clients des organismes qui ont obtenu des contrats plus longs bénéficiaient de visites plus régulières de la part des infirmières principales que ceux des organismes auxquels on avait octroyé des contrats de plus courte durée. Les clients soignés par des organismes à but lucratif affichaient un niveau de satisfaction légèrement plus élevé et de meilleurs résultats en matière de santé mentale que ceux qui sont traités par des organismes sans but lucratif. Le pourcentage de visites effectuées par une infirmière autorisée a été associé positivement à un résultat social plus élevé pour les clients au moment du suivi. En conclusion, les constatations de l’étude suggèrent que les variables dans les caractéristiques des contrats on eu un effet minime sur les résultats des clients recevant des soins à domicile.
Home care has become an increasingly important component of healthcare services. Publicly funded programs exist in every province, although the manner in which such services are organized and delivered varies (Health Canada 1999). In Ontario, home care falls under the jurisdiction of the Ministry of Health and Long-Term Care (MOHLTC). In 1997, the MOHLTC established 43 Community Care Access Centres (CCACs) to provide a single point of access to home care and to coordinate long-term care placement. By 2002, two CCACs had merged, leaving a total of 42 CCACs. The CCACs are statutory not-for-profit corporations under the Community Care Access Corporations Act, 2001, and are accountable to the MOHLTC through a Memorandum of Understanding. The CCACs purchase services from providers using a competitive process known as a Request for Proposal (RFP) that sets out a CCAC’s service requirements (Carefoote 1998). Introduction of the RFP process has been associated with a large increase in the market share of for-profit nursing provider agencies (Doran et al. 2002).
It is important to evaluate the impact of the competitive RFP process on the quality of home care services because competition may work in disparate ways. For instance, competition may result in lower contractual prices, thereby forcing lower wages/benefits on staff, leading to decreased morale and increased staff turnover. Such labour market consequences may adversely affect care quality (Shapiro 1997). On the other hand, because CCACs may establish standards for client services, there is a potential that the competitive process may enhance the quality of care. The purpose of this study was to investigate the impact of the RFP process – specifically, the profit status of provider agencies awarded contracts, the service volume awarded and contract duration – on the quality of home care recipient services and outcomes.
Literature concerning the impact of the competitive bidding process on care quality and efficiency is limited. McCombs and Christianson (1987) described the experience of the National Long-Term Care Channeling Demonstration project in the United States. Of the five projects that used competitive bidding to select long-term care providers, those with one winner produced lower bid prices, presumably because lower prices were offset by higher volumes. However, there were increased monitoring and administration costs associated with the single winning bidders. In an analysis of the Massachusetts Department of Public Health’s competitive bidding for mental health services, Schlesinger et al. (1986) concluded that the contracting process added administrative complexity and that the initial cost savings appeared to be relatively small. To the extent that cost savings existed, they primarily reflected lower wages paid by for-profit, as opposed to public, agencies (Schlesinger et al. 1986). These lower wages were also associated with higher employee turnover and reduced continuity of care. Similar results were reported by Shapiro (1997) for Manitoba.
In an analysis of the impact of competitive bidding for home care services in Ontario, Browne (2000) observed that although market competition could lower costs, improve efficiency and enhance the quality and quantity of service in the short term, it might not have positive long-term effects. He contended that trust could be undermined and continuity of care weakened if staff turnover results from contracts that change every few years. Aronson and Neysmith (2006) noted that managed competition in Ontario has forced provider agencies to adopt leaner forms of work organization, such as cutting supervisory positions, in order to remain competitive. In at least one case, workers unionized because of lack of confidence in continued employment security with their agency as a result of the perceived risks of managed competition. In this same case, which resulted in an agency closure, “workers, union and management were set against each other in ways that masked the dynamics of restructuring” (Aronson and Neysmith 2006: 41). At the CCAC level, managed competition has blocked key avenues of communication among agencies competing for services (Williams et al. 1999). In a study of elderly women’s accounts of home care rationing, Aronson noted that some women experienced care as insufficient and depersonalizing (Aronson 2002).
Abelson et al. (2004) studied the experiences of clients, provider agencies and care managers in home healthcare in one Ontario community. They noted that while the implementation of the competitive contracting model focused attention on improved accountability between purchasers and providers, concerns were raised about both the quality of care and contractual transaction costs. Denton et al. (2002) studied occupational illnesses among office workers, nurses, personal support workers and therapists working in clients’ homes. High levels of stress, burnout and physical health problems were documented, many of which were deemed to be preventable. The study concluded that restructuring of home care services with the introduction of managed competition and organizational change were significant factors in decreasing job satisfaction, increasing absenteeism rates and increasing fear of job loss and propensity to leave.
There is a paucity of literature concerning the privatization of home care services. One US study found that non-profit home nursing agencies served more welfare, self-pay and indigent clients and made more visits per client than for-profit agencies (Shuster and Cloonan 1991). In another study, Rosenau and Linder (2001) compared performance indicators by home care agencies and concluded there was no difference between for-profit and non-profit agencies in 45% of performance indicators, whereas in 55% of the comparisons the non-profit service providers were reported to have performed better.
Study Variables
Donabedian’s structure, process, outcome framework was used to evaluate the relationships among contract structural variables, nursing process variables and client outcome variables (Donabedian 1980). The contract structural variables selected for investigation were profit status of the nursing provider agency, volume of service awarded and duration/potential for renewal of the service contract. Profit status was selected for investigation because it has been associated with the number of client visits and the time spent in direct patient care (Shuster and Cloonan 1991), both of which may affect client outcomes. Duration of service contract and potential for renewal were selected as variables for investigation because of evidence that longer contracts produce greater stability in staffing, resulting in higher staff morale and greater continuity of care (Schlesinger et al. 1986; Shapiro 1997). Volume of service was selected for investigation because it, too, could provide agencies with the opportunity to build stable staffing resources. The nursing process variable selected for investigation was continuity of care, which was operationally defined as the consistency of visits made by the principal nurse providing home nursing care (Woodward et al. 2004). The principal nurse was determined as the individual nurse who made the majority of visits over a client’s home care stay or over six weeks of data collection, whichever came first. Because of the literature suggesting better outcomes with a higher skill mix among providers (Aiken et al. 2002; McGillis Hall et al. 2003), percentage of visits made by a registered nurse (RN) was also included as a nursing intervention variable. In this study, we focused on two client outcome variables: satisfaction with nursing care and functional health outcomes, which were operationally defined as clients’ achievement of physical, emotional, social and role functioning. In addition, data were collected on clients’ medical diagnosis, age, gender, baseline functional health and baseline status on the outcome variables, because these variables were expected to explain variation in outcome achievement (Tourangeau and Tu 2003).
Methods
Data were collected over a 12-month period in 2002–2003. A survey design was used to collect data on the contract characteristic variables. Data on nursing process variables were collected from provider agency administrative records. A repeated measures design was used to collect data on client outcomes at two points: on admission or recruitment into the study (T1) and at discharge or after six weeks (T2), whichever came first. The study received ethical approval from the Research Ethics Board of the University of Toronto.
Setting and sample
The setting consisted of CCACs and their nursing provider agencies. CCACs were eligible to participate if they had participated in an earlier phase of the study, in which data were collected on the service volumes and duration of service contracts awarded to nursing provider agencies in Ontario prior to restructuring through to 2003 (Doran et al. 2002). Forty-two of the 43 CCACs in Ontario had participated in this earlier study. A purposeful sample of one CCAC from each region in Ontario was targeted, ensuring regional representation. A total of 11 CCACs were randomly sampled from among the 42 provincial CCACs. If a CCAC declined, another CCAC in the same region was invited to participate. Eleven CCACs declined to participate, either because of multiple concurrent commitments or owing to impending changes in provider contracts related to a competitive bidding cycle. All nursing provider agencies holding contracts with the participating CCACs were invited to participate. One agency with a single contract declined to participate, resulting in a total of 11 nursing agencies with 34 contracts represented. There were more contracts than agencies because nursing provider agencies held contracts with more than one CCAC. Moreover, more than one nursing agency in a given CCAC may be awarded a contract. All clients over 18 years of age who received home nursing services and were able to provide informed consent were eligible to participate. A sample size of 700 clients was sought based on an estimated small effect size and a power of 95%. A small effect size was anticipated based on the findings of an earlier study by Irvine Doran et al. (2000), which had investigated the relationship between nursing services and home care client outcomes in Ontario using the same outcome measure as that utilized in this study.
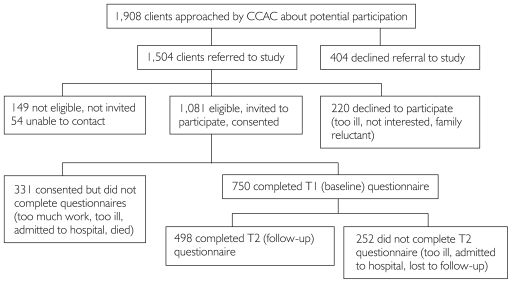
Figure 1 provides a summary of the client sample recruitment and follow-up. Of the 1,908 clients referred to the study coordinator, 1,081 were eligible and were invited to participate. Of these, 750 consented to participate, for a response rate of 69%. The three most common reasons for refusal to participate included “too ill,” “not interested” and “family member reluctant.” Follow-up assessments were completed on a total of 498 clients. Reasons for subject dropout included “too ill,” “admitted to hospital” and “died.” Independent t-tests were used to compare responders and those who dropped out at Time 2 on the basis of age and T1 SF-36 subscales, specifically, general health status, vitality, emotional role, physical role, physical function, social function, vitality and mental health. No meaningful differences were noted (see Table 1). Cross-tabs were conducted to compare responders and non-responders on the basis of gender and profit status, with only small differences noted (see Table 2).
FIGURE 1.
Summary: Client sample recruitment and follow-up
TABLE 1.
Age and baseline outcome characteristics of clients who responded and did not respond to Time 2 questionnaire
| Characteristic | Responded T2 Mean (SD) (n=494) | Did Not Respond T2 Mean (SD) (n=255) |
|---|---|---|
| Age | 64.09 (15.29) | 63.10 (16.30) |
| T1 General Health Status (SF-36) | 46.64 (23.53) | 46.86 (22.96) |
| T1 Bodily Pain | 3.72 (1.49) | 3.72 (1.49) |
| T1 Emotional Role Function | 58.13 (35.29) | 56.03 (34.50) |
| T1 Physical Role Function | 35.14 (31.71) | 33.51 (30.23) |
| T1 Physical Function | 33.38 (29.39) | 34.24 (28.72) |
| T1 Mental Health | 63.13 (21.91) | 62.47 (21.21) |
| T1 Social Function | 48.39 (25.99) | 51.00 (26.13) |
| T1 Vitality | 36.14 (22.94) | 37.10 (22.76) |
TABLE 2.
Gender and profit status of clients who responded and did not respond to Time 2 questionnaire
| Responded T2 Frequency (Percentage) (n=491) | Did Not Respond T2 Frequency (Percentage) (n=252) | |
|---|---|---|
| Male | 197 (40.1%) | 92 (36.5%) |
| Female | 294 (59.9%) | 160 (63.5%) |
| For Profit | 287 (58.2%) (n=493) | 145 (56.9%) (n=255) |
| Not for Profit | 206 (41.8%) | 110 (43.1%) |
The mean age of clients was 64 years; 61% of participants were married or cohabitating, 61% were female and 60% had completed high school. The majority (84%) of clients were newly admitted for nursing services. The most common diagnoses were diseases or disorders of the skin and subcutaneous tissue (21.4%, primarily requiring wound care), cardiovascular system (13.3%), digestive system (12.2%) and musculoskeletal system (10.6%). Carcinoma was recorded as a primary diagnosis for 153 clients (20.8%); the proportion of clients with carcinoma was the same among for-profit and not-for-profit agencies. Two hundred ninety-eight (42%) of the clients were classified by the CCAC case manager with an anticipated duration of care of five weeks or less; 413 or 58% of the clients had an anticipated duration of care of over five weeks.
Measures
PATIENT CHARACTERISTIC VARIABLES
Clients’ medical diagnosis, age and gender were obtained from CCAC records. To enable risk adjustment based on the client baseline functional healthcare needs, we used the MI-Choice Screener (Fries et al. 2002), a set of 32 items excerpted from the interRAI-Home Care tool, originally designed as a telephone screening tool to determine whether the more in-depth interRAI-HC assessment was warranted. Part A is a general section with such items as difficulty with housework, stamina/physical activity, bathing, skin problems and cognitive skills. Lower scores represent less difficulty in performing the activity. This variable is referred to as “screener general” in the presentation of results. Part B of the MI-Choice Screener assesses specific instrumental activities of daily living (IADLs) such as preparing meals, ordinary housework, managing medications and shopping. Scores range from 0 (no difficulty in performing the activity) to 1 (difficulty in performing the activity). This variable is referred to as “screener IADL” in this report.
At the time of referral to the CCAC, case managers classified clients as short-term or long-term. Long-term clients had an anticipated duration of care of three months or more. This classification was used as a crude measure of chronicity in the risk adjustment models described below.
CONTRACT CHARACTERISTIC VARIABLES
Data on profit status of the nursing provider agency, the contract volume, duration and potential for renewal were collected from CCAC records using a survey tool that each CCAC responded to. Contract volume was measured as the total number of annual nursing visits in the most recent service contract. Duration and potential length if contract is renewed were measured in months.
NURSING PROCESS VARIABLES
The nursing provider agencies provided the data on the consistency of visits made by the same nurse and number of visits made by a registered nurse (RN) for each client enrolled in the study. The proportion of visits made by an RN was computed by dividing the number of visits by an RN by the total number of nursing visits (i.e., RN plus registered practical nurse visits) for the client over the six-week period of data collection.
CLIENT OUTCOME VARIABLES
The Client Satisfaction Scale (CSS) (Reeder and Chen 1990) was used to collect data on client satisfaction. The CSS is a 35-item tool assessing technical quality and personal relationships between patients and providers, and general satisfaction. Reliability of the CSS has been reported at 0.93 using Cronbach alpha (Reeder and Chen 1990). Cronbach alpha for the CSS in this study is reported in Table 3. Client health outcomes were assessed with the Medical Outcome Study SF-36 (Stewart and Kamberg 1992). The SF-36 was found to be reliable (Cronbach alpha 0.76 to 0.94 for each subscale), sensitive to change and related to several nursing variables (e.g., proportion of RN visits) in a home healthcare setting (Irvine Doran et al. 2000). The Cronbach alpha for the SF-36 subscales in this study were >0.79, with the exception of the social function subscale. Higher scores reflect better outcomes.
TABLE 3.
Client outcome variables
| Outcome Variable | T1 Cronbach Alpha | T1 Mean (SD) | T2 Cronbach Alpha | T2 Mean (SD) |
|---|---|---|---|---|
| Client Satisfaction with Nursing Care | 0.96 | 4.16 (0.54) | ||
| SF-36 Subscales | ||||
| General Health (n=498) | 0.79 | 46.47 (23.53) | 0.85 | 47.07 (25.79) |
| Physical Function (n=483) | 0.93 | 33.63 (29.15) | 0.95 | 37.32 (32.10) |
| Physical Role (n=478) | 0.96 | 34.53 (31.21) | 0.96 | 36.41 (31.18) |
| Emotional Role (n=480) | 0.96 | 57.37 (34.89) | 0.95 | 59.12 (35.56) |
| Social Function (n=495) | 0.61 | 49.33 (26.07) | 0.78 | 51.99 (30.83) |
| Bodily Pain (n=490) | 0.80 | 50.18 (25.33) | 0.90 | 50.69 (26.62) |
| Vitality (n=484) | 0.80 | 36.48 (22.71) | 0.87 | 39.74 (24.81) |
| Mental Health (n=483) | 0.83 | 62.90 (21.49) | 0.87 | 67.91 (21.62) |
Data analysis
Means and standard deviations were calculated to describe the distribution of the study variables. Hierarchical linear modelling (HLM) was conducted to assess the relationships among the contract characteristic variables, nursing intervention variables and client outcomes. Risk adjustment was addressed in three ways: (1) controlling for functional healthcare needs (MI-Choice Screener); (2) controlling for age, medical diagnosis, cancer diagnosis and baseline scores on SF-36 subscales; and (3) controlling for anticipated duration of care as a measure of chronicity. For-profit status was coded 0 and not-for-profit status was coded 1.
Results
Descriptive results
Eighteen (52.9%) of the nursing provider contracts were held by for-profit agencies. On average, there were three nursing service contracts per CCAC (range, 2–5), with an average volume of 56,352 (±27,760) nursing visits, contract length 35 (±7.4) months and potential length 52 (±14.6) months if extensions were granted. The length of contracts was comparable to the provincial mean of 33 months and potential length if contract renewed of 49 months. Clients in the study received a median of 10 visits over six weeks or less. The consistency of nurse provider ranged from 0.18 (e.g., two out of the 11 nursing visits were made by the same nurse) to 1.0 (all nursing visits were made by the same nurse). On average, the same nurse provided 67% of visits to a client, and 72% (±39%) of the visits were made by an RN. The mean and standard deviation of the client outcome measures are presented in Table 3. There was a significant improvement from T1 (admission or recruitment) to T2 (discharge or after six weeks) in four of the subscales measuring client health outcomes: clients’ physical function, social function, vitality and mental health.
HIERARCHICAL LINEAR MODELLING (HLM) RESULTS
The results of the HLM analysis testing the relationships among the contract characteristic variables, consistency of nurse visits, proportion of visits made by an RN and client outcomes are presented below. Analysis was restricted to those outcomes that demonstrated significant improvement.
CONSISTENCY OF NURSE VISITS
There were 540 clients who had complete data on the contract characteristic variables and consistency of nurse visits at T2. Age of client (t=2.67, df=521, p=0.01) and length of contract (t=2.84, df=521, p=0.01) were positively associated with consistency of nurse visits. The consistency of nurse visits decreased as the total number of visits increased (t=–5.46, df=521, p=.0001), suggesting that there is lower consistency of care provided for longer-stay clients.
PHYSICAL FUNCTION
There were 336 clients who had complete data on the contract characteristic variables and physical function at T2. Client age (t=–4.21, df=283, p=0.001), screener IADL (t=–2.88, df=283, p=0.01) and anticipated duration of care (t=–3.38, df=283, p=0.001) were negatively associated with physical function at T2, while physical function at T1 (t=10.64, df=283, p=0.001) was positively associated with physical function at T2. These results indicate that older, chronically ill clients had lower physical functioning at T2 than younger, more acute clients. Clients who lived with someone were more likely to have higher physical function scores at T2 than those who lived alone (t=2.90, df=283, p<0.01). The interaction between cancer as primary diagnosis and physical function at T1 was significant (t=2.77, df=283, p=0.01). This conditional relationship suggests that for clients with no cancer diagnosis, baseline physical function is highly positively related to follow-up functional status. For clients with a cancer diagnosis, baseline physical function is not as highly related to follow-up physical function.
SOCIAL FUNCTION
There were 355 clients who had complete data on the contract characteristic variables and social function at T2. Social function at T1 (t=12, df=304, p<0.001), screener general (t=2.04, df=304, p=0.04) and percentage of visits by an RN (t=2.69, df=304, p=0.01) were all positively associated with social function at T2. Screener general assesses difficulty with housework, stamina/physical activity, bathing, skin problems, and cognitive skills. As previously noted, lower scores represent less difficulty in performing the activity. A positive relationship between screener general and social function at T2 is counter-intuitive. Clients who had more visits from an RN had higher social functioning at T2 than clients who had fewer visits made by an RN. Overall, diagnostic category was a predictor of social function at T2 (t=1.85, df=304, p=0.02), suggesting social function varied by medical diagnosis category. Poorer general health status, as assessed by SF-36 at T1, was negatively related to social function at T2 (t=–2.34, df=304, p=0.02).
VITALITY
There were 339 clients who had complete data on the contract characteristic variables and vitality at T2. Vitality at T1 was positively associated with vitality at T2 (t=13.79, df=288, p=0.001). Clients with shorter anticipated duration of care (t=–3.17, df=288, p=0.002) and higher IADL functioning (t=–1.90, df=288, p=0.05) had higher scores for vitality at T2.
MENTAL HEALTH
There were 429 clients who had complete data on the contract characteristic variables and mental health at T2. Clients from for-profit agencies experienced higher scores for mental health compared to clients from not-for-profit agencies (t=2.36, df=378, p=0.02). Mental health at T1 was also a predictor of mental health at T2 (t=15.05, df=378, p<0.01).
CLIENT SATISFACTION
On a scale of 1 to 5, clients were highly satisfied with nursing care (mean = 4.16, ±0.54). There were 355 clients who had complete data on the contract characteristic variables and satisfaction at T2. Clients from for-profit agencies reported slightly higher satisfaction scores compared to clients from not-for-profit agencies (t=2.75, df=322, p=0.01). The interaction between age and gender of clients was also significant (t=–2.47, df=322, p=0.02); younger females were more satisfied than younger males, but older females were less satisfied than older males.
Discussion
The purpose of this study was to investigate the impact of the RFP process – specifically, the profit status of the provider agency, service volume and contract duration on the quality of care and outcomes for home care clients. For the most part, no differences were observed in the quality of care (i.e., consistency of visits made by the principal nurse) and client outcomes between for-profit and not-for-profit agencies. The two differences that were observed were small. The overall lack of difference between for-profit and not-for-profit agencies is consistent with what has been previously observed, suggesting that differences are disappearing as both types of agencies face similar market competition (Rosenau and Linder 2001). For instance, in Ontario, all provider agencies are expected to meet specific service standards that are delineated in the RFP and monitored by the CCACs. The results concerning the other contract characteristic variables were mixed. Service volume did not have a significant impact on the quality of care or client outcome variables. On the other hand, there is evidence that the length of service contracts affords provider agencies some benefits. Specifically, there was a significant relationship between longer service contracts and greater consistency of principal nurse visits (i.e., continuity of care). Perhaps the agencies awarded longer contracts are able to build their staffing to levels that provide the flexibility and staff resources to optimize nurse assignments.
The majority of clients in this study were long-term clients, with an anticipated duration of care of over five weeks. These clients were followed for a maximum of six weeks. It is possible that this follow-up did not provide sufficient time to observe significant change in all of the outcomes for these types of clients; specifically, there were four dimensions of the SF-36 that did not demonstrate significant change from baseline to follow-up assessment (i.e., general health, physical role, emotional role and bodily pain). As a result, the impact of the contract characteristic variables on these outcomes may not have been fully tested in this study.
Consistency of care provider is one measure of continuity (Woodward et al. 2004). Absolute consistency is not an achievable target for all clients, and it is probably not even a desirable target because a change in staffing provides the opportunity for the infusion of new care perspectives. No differences in consistency of nurse provider were observed between for-profit and not-for-profit agencies. Not surprisingly, it was harder to maintain consistency for longer-term clients, although older clients received higher consistency than younger clients.
Two types of client outcomes were investigated: satisfaction with nursing care and health outcomes. Clients were highly satisfied with their nursing care, and clients from for-profit agencies were slightly more satisfied than those from not-for-profit agencies. It is possible that the clients’ perceptions could have been adversely affected if they were cared for by an agency that was experiencing significant shifts in service volumes. This was more likely to be the case for not-for-profit agencies, because there was a significant increase in the market share for for-profit agencies following the introduction of managed competition. The percentage volume of nursing services provided by for-profit provider agencies increased from 18% in 1995 to 46% in 2001 (Doran et al. 2002).
In the HLM analyses, we controlled for a number of client characteristic variables. T2 outcomes were found to be related to many of these, most importantly the clients’ baseline health status, ADL or IADL functioning and sometimes age and gender. For all but one of the outcomes, there was no difference in outcome status for clients cared for by for-profit and not-for-profit agencies; specifically, a difference was observed for mental health outcome, demonstrating better mental health outcomes for clients cared for by for-profit agencies than not-for-profit agencies. This one difference could have occurred by chance.
Consistency of care provider was not a significant predictor of client health outcomes. In contrast, the percentage of visits made by an RN was positively associated with clients’ social function outcome. These findings support the results of a previous study of home care nursing by O’Brien-Pallas et al. (2002) and underscore the need to retain RN skills at a defined proportion within an RFP.
Study limitations
A high percentage of the clients initially referred to the study declined to participate (42%) or failed to return the T2 questionnaire (34%). The research assistant’s records of responders and non-responders indicated that more acutely ill clients declined to participate in the study than less acutely ill clients. However, no significant differences were noted between the T2 responders and T2 non-responders on baseline outcome measures, age, gender or the provider agency’s profit status. Therefore, it is difficult to judge the impact of a non-response bias on the study findings. The results can be generalized only to clients who are similar to those represented in this study.
Conclusion
Debates about the comparative performance of for-profit and not-for-profit home healthcare providers have been prevalent in the healthcare literature (Rosenau and Linder 2001). Much of this debate has yet to be informed by evaluative studies. The current study begins to address this gap. In this study, we found that satisfaction with care was high among clients of for-profit and not-for-profit agencies. There were few differences in client outcomes by profit status of the nurse provider agency. Social function outcome was better for clients who received a higher proportion of registered nurse visits. It is important to develop a better understanding of the management and care practices that are most influential in promoting high-quality performance and optimum outcomes for clients in the home healthcare setting.
Acknowledgments
We gratefully acknowledge the Canadian Health Services Research Foundation (CHSRF) and the Ontario Ministry of Health and Long-Term Care (MOHLTC) for their funding of this research. The opinions, results and conclusions are those of the authors. No endorsement by the CHSRF or MOHLTC is intended or should be inferred. We would like to thank Barbara Thomson and the Statistical Consulting Service, Dept. of Statistics, University of Toronto, for their contribution to the data analysis.
Contributor Information
Diane Doran, Lawrence Bloomberg Faculty of Nursing, University of Toronto, Toronto, ON; School of Nursing, Queen’s University, Kingston, ON.
Jennie Pickard, Performance Management and Accountability, Central East Community Care Access Centre, Whitby, ON.
Janet Harris, Professional Practice and Chief Nursing Executive, Rouge Valley Health System, Whitby, ON.
Peter C. Coyte, Department of Health Policy, Management and Evaluation, Faculty of Medicine; University of Toronto, Toronto, ON.
Andrew R. Macrae, Manitoba Institute of Child Health, Dept. of Biochemistry and Medical Genetics, University of Manitoba, Winnipeg, MB.
Heather Laschinger, School of Nursing, University of Western Ontario, London, ON.
Gerarda Darlington, Department of Mathematics and Statistics, University of Guelph, Guelph, ON.
Jennifer Carryer, Faculty of Nursing, University of Toronto, Toronto, ON.
References
- Abelson J.S.T., Gold C., Woodward D.O., O’Connor D., Hutchison B. Managing under Managed Community Care: The Experiences of Clients, Providers and Managers in Ontario’s Competitive Home Care Sector. Health Policy. 2004;68(3):359–72. doi: 10.1016/j.healthpol.2003.10.011. [DOI] [PubMed] [Google Scholar]
- Aiken L.H., Clarke S.P., Sloane D.M., Sochalski J., Silber J.H. Hospital Nurse Staffing and Patient Mortality, Nurse Burnout, and Job Dissatisfaction. Journal of the American Medical Association. 2002;288(16):1987–93. doi: 10.1001/jama.288.16.1987. [DOI] [PubMed] [Google Scholar]
- Aronson J. Elderly People’s Accounts of Home Care Rationing: Missing Voices in Long-Term Care Policy Debates. Aging & Society. 2002;22:399–418. doi: 10.1017/s0144686x02008759. [DOI] [PubMed] [Google Scholar]
- Aronson J., Neysmith S.M. Obscuring the Costs of Home Care: Restructuring at Work. Work, Employment and Society. 2006;20(1):21–45. [Google Scholar]
- Browne P.L. Unsafe Practices: Restructuring and Privatization in Ontario Health Care. Ottawa: Canadian Centre for Policy Analysis; 2000. [Google Scholar]
- Carefoote R.L. Health care issues: Home care quality management, Where are we now? Where do we go from here? Canadian Journal of Nursing Administration. 1998;(May/June):78–91. [PubMed] [Google Scholar]
- Community Care Access Corporations Act, 2001, RSO 2001, c. 33. Retrieved March 25, 2007. http://www.e-laws.gov.on.ca/DBLaws/Statutes/English/01c33_e.htm .
- Denton M., Zeytinoglu I.U., Davies S., Lian J. Job Stress and Job Dissatisfaction of Home Care Workers in the Context of Health Care Restructuring. International Journal of Health Services. 2002;32(4):327–57. doi: 10.2190/VYN8-6NKY-RKUM-L0XW. [DOI] [PubMed] [Google Scholar]
- Donabedian A. The Definition of Quality and Approaches to Its Assessment. Ann Arbor, MI: Health Administration Press; 1980. [Google Scholar]
- Doran D.M., Pickard J., Harris J., Coyte P.C., MacRae A., Laschinger H., et al. Competitive Bidding for Community-Based Nursing Services. Toronto: Report submitted to Canadian Health Services Research Foundation; 2002. [Google Scholar]
- Fries B.E., Shugarman L.R., Morris J.N., Simon S.E., James M. A Screening System for Michigan’s Home- and Community-Based Long-Term Care Programs. Gerontologist. 2002;42(4):462–74. doi: 10.1093/geront/42.4.462. [DOI] [PubMed] [Google Scholar]
- Health Canada. Provincial and Territorial Home Care Programs: A Synthesis for Canada. Ottawa: Author; 1999. [Google Scholar]
- Irvine Doran D.M., O’Brien-Pallas L., Murray M., Cockerill R., Sidani S., Laurie-Shaw B., et al. The Reliability and Validity of Two Health Status Measures for Assessing Outcomes of Home Care Nursing. Research in Nursing & Health. 2000;23:43–54. doi: 10.1002/(sici)1098-240x(200002)23:1<43::aid-nur6>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- McCombs J.S., Christianson J.B. Applying Competitive Bidding to Health Care. Journal of Health Politics, Policy & Law. 1987;12(4):703–22. doi: 10.1215/03616878-12-4-703. [DOI] [PubMed] [Google Scholar]
- McGillis Hall L., Doran D.M., Baker G., Pink G., Sidani S., O’Brien-Pallas L., et al. Nurse Staffing Models As Predictors of Patient Outcomes. Medical Care. 2003;41:1096–109. doi: 10.1097/01.MLR.0000084180.07121.2B. [DOI] [PubMed] [Google Scholar]
- O’Brien-Pallas L.L., Irvine Doran D.M., Murray M., Cockerill R., Sidani S., Laurie-Shaw B., et al. Evaluation of a Client Care Delivery Model, Part 2: Variability in Client Outcomes in Community Home Nursing. Journal of Nursing Economic$ 2002;20(1):13–21–36. [PubMed] [Google Scholar]
- Reeder P.J., Chen S.C. A Client Satisfaction Survey in Home Health Care. Journal of Nursing Quality Assurance. 1990;5(1):16–24. [PubMed] [Google Scholar]
- Rosenau P.V., Linder S.H. The Comparative Performance for For-Profit and Nonprofit Home Health Care Services in the US. Home Health Care Services Quarterly. 2001;20(2):47–59. doi: 10.1300/J027v20n02_03. [DOI] [PubMed] [Google Scholar]
- Schlesinger M., Dorwart R.A., Pulice R.T. Competitive Bidding and States’ Purchase of Services: The Case of Mental Health Care in Massachusetts. Journal of Policy Analysis & Management. 1986;5(2):245–63. [PubMed] [Google Scholar]
- Shapiro E. The Cost of Privatisation: A Case Study of Home Care in Manitoba. Winnipeg: Canadian Centre for Policy Alternatives; 1997. [Google Scholar]
- Shuster G.F., Cloonan P.A. Home Health Nursing Care: A Comparison of Non-Profit and For-Profit Agencies. Home Health Care Services Quarterly. 1991;12(1):23–36. doi: 10.1300/J027v12n01_04. [DOI] [PubMed] [Google Scholar]
- Stewart A.L., Kamberg C.J. Physical Functioning Measures. In: Stewart A.L., Ware J.E. Jr., editors. Measuring Functioning and Well-being: The Medical Outcomes Study Approach. Durham, NC: Duke University Press; 1992. [Google Scholar]
- Tourangeau A.E., Tu J.V. Developing Risk-Adjusted 30-Day Hospital Mortality Rates. Research in Nursing & Health. 2003;26:483–96. doi: 10.1002/nur.10110. [DOI] [PubMed] [Google Scholar]
- Williams A.P., Barnsley J., Leggat S., Deber R., Baranek P. Long-Term Care Goes to Market: Managed Competition and Ontario’s Reform of Community-Based Services. Canadian Journal on Aging. 1999;18(2):125–53. [Google Scholar]
- Woodward C.A., Abelson J.S.T., Tedford S., Hutchison B. What Is Important to Continuity of Home Care? Perspectives of Key Stakeholders. Social Science & Medicine. 2004;58(1):177–92. doi: 10.1016/s0277-9536(03)00161-8. [DOI] [PubMed] [Google Scholar]