Abstract
Purpose
To determine the feasibility and diagnostic accuracy of high spatial resolution myocardial perfusion MR at 3.0 Tesla using k-space and time domain undersampling with sensitivity encoding (k-t SENSE).
Materials and Methods
The study was reviewed and approved by the local ethic review board. k-t SENSE perfusion MR was performed at 1.5 Tesla and 3.0 Tesla (saturation recovery gradient echo pulse sequence, repetition time/echo time 3.0ms/1.0ms, flip angle 15°, 5x k-t SENSE acceleration, spatial resolution 1.3×1.3×10mm3). Fourteen volunteers were studied at rest and 37 patients during adenosine stress. In volunteers, comparison was also made with standard-resolution (2.5×2.5×10mm3) 2x SENSE perfusion MR at 3.0 Tesla. Image quality, artifact scores, signal-to-noise ratios (SNR) and contrast-enhancement ratios (CER) were derived. In patients, diagnostic accuracy of visual analysis to detect >50% diameter stenosis on quantitative coronary angiography was determined by receiver-operator-characteristics (ROC).
Results
In volunteers, image quality and artifact scores were similar for 3.0 Tesla and 1.5 Tesla, while SNR was higher (11.6 vs. 5.6) and CER lower (1.1 vs. 1.5, p=0.012) at 3.0 Tesla. Compared with standard-resolution perfusion MR, image quality was higher for k-t SENSE (3.6 vs. 3.1, p=0.04), endocardial dark rim artifacts were reduced (artifact thickness 1.6mm vs. 2.4mm, p<0.001) and CER similar. In patients, area under the ROC curve for detection of coronary stenosis was 0.89 and 0.80, p=0.21 for 3.0 Tesla and 1.5 Tesla, respectively.
Conclusions
k-t SENSE accelerated high-resolution perfusion MR at 3.0 Tesla is feasible with similar artifacts and diagnostic accuracy as at 1.5 Tesla. Compared with standard-resolution perfusion MR, image quality is improved and artifacts are reduced.
Introduction
Among the cardiac applications of MR imaging, signal-to-noise (SNR) limited methods such as myocardial perfusion MR (perfusion MR) are most likely to benefit from higher field strength (1-9). Initial studies have shown improvements in SNR, contrast enhancement and diagnostic accuracy for perfusion MR at 3.0 Tesla compared with 1.5 Tesla (1,2,5).
One of the main challenges of first-pass perfusion MR imaging is the need for rapid data acquisition in order to minimize motion-induced artifacts and to maximise cardiac coverage during the myocardial passage of the contrast agent. Spatial undersampling methods, such as sensitivity encoding (SENSE) can provide some of the necessary data acquisition speed, but are associated with an SNR penalty, which increases notably with greater than twofold acceleration in 2D imaging methods (10,11). Methods that exploit spatiotemporal data correlations such as k-space and time domain undersampling with SENSE (k-t SENSE) allow for substantial further acceleration of data acquisition (12-15). k-t SENSE typically shows improved SNR behaviour over SENSE as the temporal bandwidth in reconstruction is adapted to the actual object dynamics based on training data. Applying spatial and spatiotemporal undersampling methods to perfusion MR at 3.0 Tesla is attractive, because the high field strength will partly compensate for the associated SNR loss.
The purpose of this study was to determine the feasibility and diagnostic accuracy of high spatial resolution myocardial perfusion MR at 3.0 Tesla using k-t SENSE in comparison with k-t SENSE high spatial resolution perfusion MR at 1.5Tesla and standard-resolution acquisition at 3.0 Tesla. .
Methods
This study received financial support from Bayer Schering Pharma AG (Zurich, Switzerland) and the company provided the contrast agent. The authors had full control of the data and over the information submitted for publication.
Study population
Fifty-one subjects were prospectively recruited for the study between June and December 2006. Fourteen were volunteers without heart disease and no known cardiovascular risk factors (7 male, mean age 28 yrs, range 22-44). Thirty-seven were patients referred for invasive x-ray coronary angiography for evaluation of suspected or known coronary artery disease (CAD) (27 male, mean age 58 yrs, range 41-73). Exclusion criteria for recruitment were general contraindications to MR imaging or adenosine infusion. All subjects gave written informed consent and the study was approved by the local ethics review board. Of the 37 recruited patients, 2 were not studied at 1.5 Tesla, one because he developed angina during the first study at 3.0 Tesla leading to urgent X-ray angiography and a second patient because he was unwilling to attend. At 3.0 Tesla all studies were completed but in one patient data reconstruction failed. Finally, in one patient image quality was poor due to cardiac arrhythmia and poor breath-holding at both field strengths. Data from 33 of 37 patients were therefore available at both 1.5 and 3.0 Tesla and these 33 patients were used for comparative analyses.
Pulse sequences
k-t SENSE perfusion MR was used in combination with a saturation recovery gradient echo pulse sequence (repetition time /echo time msec 3.0/1.0, flip angle 15°, saturation prepulse delay 150 ms, partial Fourier sampling, acquisition window 120 ms, slice thickness 10 mm, k-t factor of 5 with 11 k-t interleaved training profiles, effective acceleration 3.8, 4 slices acquired sequentially over 2 RR intervals) (14). Because of different gradient performance and the aim to keep a constant acquisition window, 1.5 Tesla yielded an in-plane spatial resolution of 1.5 × 1.5 mm2, while at 3 Tesla in-plane resolution was 1.3 × 1.3 mm2.
Standard-resolution perfusion MR data were acquired using a pulse sequence with identical prepulse and imaging parameters as described for k-t SENSE data acquisition and used 2x SENSE acceleration. This provided an in-plane spatial resolution of 2.5 × 2.5 mm2.
Perfusion MR
MR studies were performed on 3.0 Tesla and 1.5 Tesla clinical MR systems (Achieva, Philips Medical Systems, Best, The Netherlands). Dedicated cardiac phased array receiver coils were used for signal reception (5-element at 1.5 Tesla, 6-element at 3.0 Tesla). All data were acquired during breath-holding in the end-inspiratory position. The true short axis of the left ventricle was determined from a series of scout images. Perfusion MR data were acquired in the short axis orientation at four different cardiac levels. All perfusion acquisitions used the same contrast regime of 0.1mmol/kg Gadobutrolum (Gadovist, Schering, Berlin, Germany) injected into an antecubital vein with the use of a power injector (Medrad Spectris Solaris, Medrad, Indianola, PA) at an injection speed of 5ml/sec followed by a 20 ml Saline flush.
Volunteer studies
Volunteers underwent rest perfusion MR studies at 3.0 Tesla and 1.5 Tesla in random order and on separate days. In addition, separate 2x SENSE rest perfusion MR scans were also performed at 3.0 Tesla.
In order to allow for measurements of SNR, noise maps were generated immediately after the contrast enhanced perfusion MR study in four volunteers from a separate zero flip angle scan with reconstruction coefficients inherited from the signal containing, non-zero flip angle acquisition. SNR was determined as the ratio of average absolute signal to standard deviation of the real channel of noise in the myocardial region-of-interests. Data were further normalized to unit voxel size to account for the small differences in spatial resolution between 1.5 and 3.0 Tesla.
Patient studies
Patient demographics are listed in Table 1. All patients were awaiting invasive X-ray angiography by clinical referral for evaluation of chest pain. They underwent adenosine-stress perfusion MR at 3.0 Tesla and 1.5 Tesla in random order and on separate days within 14 days of invasive X-ray angiography. Adenosine was administered intravenously at a dose of 140 mcg/kg/min during heart rate and blood pressure monitoring. Stress perfusion images were acquired after 3 minutes of the infusion. Late gadolinium-enhanced imaging with an appropriate inversion time was carried out 10 minutes after the contrast bolus injection and using an inversion recovery segmented k-space gradient echo pulse sequence (repetition time /echo time msec 7.5/3.8, flip angle 15°, spatial resolution 1.3mm × 1.3mm × 10mm, 8-12 slices, no interslice gap).
Table 1.
Baseline demographic characteristics, cardiac risk factors and angiographic findings of recruited patients (n=37)
| Sex - no. (%) | |
| Male | 27 (73 %) |
| Female | 10 (27 %) |
| Age - yr * | 58 (± 11) |
| Risk factors - no. (%) | |
| Diabetes mellitus | 8 (21 %) |
| Hypertension | 19 (52 %) |
| Hypercholesterolemia | 20 (54 %) |
| Previous MI | 3 (8 %) |
| Current or recent smoker | 23 (62 %) |
| Family history of premature CAD | 10 (27 %) |
| X-ray angiography findings | |
| No CAD >50% | 17 (46 %) |
| Single vessel | 9 (24 %) |
| Two-vessel | 7 (19 %) |
| Three-vessel | 4 (10 %) |
| LAD disease | 12 (33 %) |
| LCX disease | 8 (21 %) |
| RCA disease | 15 (41 %) |
MI = myocardial infarction.
CAD = Coronary artery disease
LAD = left anterior descending coronary artery
LCX = left circumflex coronary artery
RCA = right coronary artery
Analysis
All data were reviewed on a post-processing workstation (ViewForum, Philips Medical Systems, Best, The Netherlands) by an experienced observer (SP, 7 years perfusion MR experience) who was blinded to all clinical information.
In all studies, image quality was graded on a scale between 0-4 (0=non-diagnostic, 1=poor, 2=moderate, 3=good, 4=excellent). Occurrence of artifacts related to the k-t reconstruction, respiratory motion, ECG gating and endocardial dark rim artefact were scored between 0-4 (0=none, 1=minor, 2=moderate, 3=severe, 4=images non-diagnostic). The maximal transmural width of endocardial dark rim artifacts was measured using electronic callipers.
From volunteer data, myocardial signal intensity (SI) curves were derived using commercially available software (MASS, Medis, The Netherlands). Contrast enhancement ratios were calculated as (peak - baseline signal intensity) / baseline signal intensity. The mean values derived for the systolic mid-ventricular section were used for statistical comparisons.
In patients, two observers (JS, 10 years perfusion MR experience and JG, 5 years perfusion MR experience) reported perfusion defects in each segment of the 16 segment American Heart Association model were reported by visual analysis using a scale from 0 to 3 (0 = normal, 1 = probably normal, 2 = probably abnormal, 3 = abnormal). Abnormal perfusion was reported if contrast enhancement in a segment was delayed relative to remote segments or if a transmural enhancement gradient was seen. In case of disagreement between readers, arbitration from a third observer (SP, 5 years perfusion MR experience) was sought. A perfusion score was calculated as the sum of all segmental scores (0-48) for each patient.
Coronary angiography
Within 14 days of the MR examination, all patients underwent biplane X-ray coronary angiography using a standard technique. Angiograms were analysed by quantitative coronary analysis (QCA) (Xelera 1.2 L4 SP1, Philips Medical Systems, Best, The Netherlands) by an independent blinded reviewer (DS, 4 years coronary angiography experience). For this, the outer diameter of the contrast-filled guiding catheter was used for calibration. Coronary lesions were analyzed in several projections and the severity of coronary lesions measured from the minimal lumen diameter and percent diameter stenosis in the most appropriate angiographic view.
Statistics
Continuous data were expressed as the mean ± standard deviation and comparisons between groups were made using two-tailed paired t test. No corrections were made for multiple comparisons. Discrete data were expressed as percentages. Categorical data were compared by the χ2 test. Statistical significance was considered for p <0.05. SNR was not statistically compared, as the results were derived from only four data sets.
The diagnostic accuracy of visual analysis to detect coronary diameter stenosis > 50%, on QCA of the X-ray angiograms in vessels with a reference diameter of > 2mm was determined by receiver-operator characteristics (ROC) analysis using Analyse-it software (Analyse-it Software Ltd., Leeds, UK). The aggregate perfusion score on a quantitative scale of 0-54 served as the analysis metric.
Results
Comparison between 3.0 Tesla and 1.5 Tesla - volunteer study
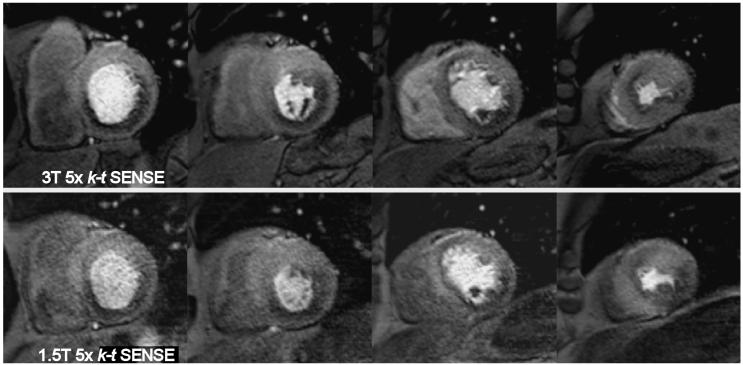
In volunteers, image quality at 3.0 Tesla was high with a mean score of 3.6 (Table 2, Figure 1). Image quality and artifact scores showed no significant differences between 3.0 Tesla and 1.5 Tesla (Table 2, Figure 2). Endocardial dark rim artifacts were small (mean width 1.6mm and 1.5mm at 3.0 and 1.5 Tesla, respectively), in line with the high spatial resolution of the data.
Table 2.
Comparison of 3.0 Tesla and 1.5 Tesla in volunteers (n = 10)
| Image quality (1-4) | Artifact score (1-4) | Artifact width (mm) | CER | SNR * | |
|---|---|---|---|---|---|
|
3.0 Tesla k-t SENSE |
3.6 (±0.3) |
0.5 (±0.2) |
1.6 (±0.3) |
1.1 (±0.4) |
11.6 (±1.5) |
|
1.5 Tesla k-t SENSE |
3.4 (±0.4) |
0.5 (±0.2) |
1.5 (±0.4) |
1.5 (±0.6) |
5.6 (±0.6) |
| p value | 0.37 | 0.67 | 0.52 | 0.012 | n/a |
|
3.0 Tesla SENSE |
3.1 (±0.4) |
1.0 (±0.4) |
2.4 (±0.4) |
1.1 (±045) |
n/a |
|
p value vs. 3.0 Tesla k-t SENSE |
0.04 | 0.02 | <0.001 | 0.96 | n/a |
n=4
CER = contrast enhancement ratio
Upslope = mean upslope of signal-intensity profiles in mid-ventricular section
SNR = myocardial signal-to-noise ratio measured at peak contrast enhancement
Figure 1.
3.0 Tesla k-t SENSE accelerated perfusion MR (3.0/1.0, flip angle, 15°) in a 26 year old healthy volunteer in the equatorial double-oblique short axis orientation. Dynamic images acquired during contrast arrival in a) the right ventricular cavity, b) the left ventricular cavity and c) the myocardium. The high image detail can be appreciated from the definition of RV trabeculation and LV papillary muscles. There is a very small rim of subendocardial dark banding artifact in the anterior wall.
Figure 2.
Perfusion MR studies from a 32 year old healthy volunteer. One dynamic image in the equatorial double-oblique short axis orientation from each study is shown acquired during contrast arrival in the LV myocardium. a) 3.0 Tesla 2x SENSE (3.0/1.0, flip angle, 15°) accelerated perfusion-MR with a spatial resolution of 2.5 × 2.5 × 10 mm3. b) 3.0 Tesla 5x k-t SENSE accelerated perfusion-MR (3.0/1.0, flip angle, 15°) with a spatial resolution of 1.3 × 1.3 × 10 mm3. c) 1.5 Tesla 5x k-t SENSE accelerated perfusion MR (3.0/1.0, flip angle, 15°) with a spatial resolution of 1.5 × 1.5 × 10 mm3. The higher image detail in both k-t SENSE images can be appreciated. The subendocardial dark rim artefact in the septum in the k-t SENSE images appears much thinner relative to the one in the 2x SENSE image. Visually the data sets at 1.5 Tesla and 3.0 Tesla appear of similar quality.
SNR was increased by a factor of 2.1 at 3.0 Tesla compared with 1.5 Tesla (11.6 ±1.5 vs. 5.6 ± 0.6, at peak signal in left-ventricular myocardium) (Figure 3). Contrast enhancement ratios at 3.0 Tesla were significantly lower than at 1.5 Tesla (1.1 vs. 1.5, p=0.012).
Figure 3.
Signal and noise maps from 5x k-t SENSE perfusion MR (3.0/1.0, flip angle, 15°) at 1.5T (left) and 3.0T (right) obtained in a 28 year old volunteer at similar cardiac levels in the equatorial double-oblique short axis orientation during contrast arrival in the myocardium. Noise maps were generated from a separate zero flip angle scan with reconstruction coefficients inherited from the signal containing, non-zero flip angle acquisition. Spatially varying noise variance is apparent. Highest noise is seen in highly dynamic areas in accordance to theory. Signal-to-noise was determined as the ratio of average absolute signal to standard deviation of the real channel of noise in the myocardial region-of-interests as indicated.
Comparison between 5x k-t SENSE and 2x SENSE at 3.0 Tesla - volunteer study
5x k-t SENSE accelerated high-spatial resolution MR perfusion at 3.0 Tesla yielded higher image quality and thinner endocardial rim artifacts than 2x SENSE accelerated standard-resolution MR perfusion (Table 2, Figure 2). Contrast enhancement ratios were similar for 2x SENSE and 5x k-t SENSE at 3.0 Tesla.
Patient study
The hemodynamic response was comparable between the stress perfusion MR studies at both field strengths. Heart rate increased by 9.2 vs. 8.8 bpm (ns) and systolic blood pressure did not change significantly at either field strength.
Image quality - patient study
The mean image quality scores in patients were 3.7 at 3.0 Tesla (Figure 4) and 3.3 at 1.5 Tesla (p=0.04). Overall artifact scores were similar between the two field strengths (0.7 vs. 0.8, p=0.56). The most commonly observed artifacts were caused by respiratory motion (occurring in 6 patients at 3.0 Tesla and 7 patients at 1.5 Tesla). Endocardial dark rim artifacts were seen in half of the image data sets at both field strengths and only occurred in the data acquired in diastole. As in volunteers, the maximal diameter of these artifacts was approximately one pixel.
Figure 4.
k-t SENSE accelerated adenosine stress perfusion MR studies (3.0/1.0, flip angle, 15°) in the equatorial double-oblique short axis orientation from three patients at 3.0 Tesla. a) The image graded as “excellent” quality shows a small subendocardial perfusion defect in the inferior septum. b) Image graded as “intermediate” image quality shows a perfusion defect in a similar location, but more transmural. c) Image graded as “poor” image quality still allows detection of a large infero-septal perfusion defect.
Diagnostic accuracy - patient study
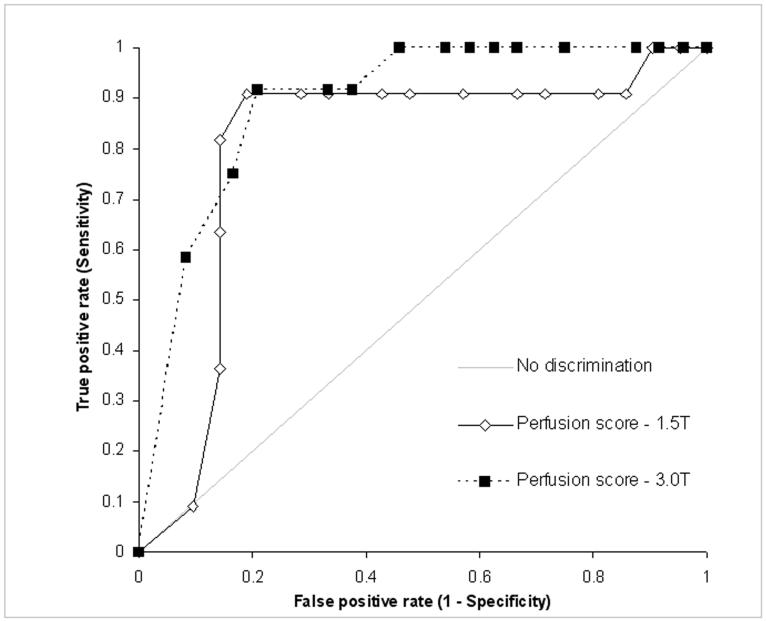
The diagnostic accuracy of visual perfusion MR analysis to detect coronary stenosis was not significantly different between 3.0 Tesla and 1.5 Tesla (AUC of ROC curve 0.89 vs. 0.80, respectively, p=0.21, Figure 5, 6, 7).
Figure 5.
Receiver operator characteristics curve of visual analysis of perfusion MR at 3.0 Tesla and 1.5 Tesla for the detection of >50% diameter coronary artery stenosis on quantitative coronary angiography. The area under the ROC curve was 0.89 at 3.0 Tesla and 0.80 at 1.5 Tesla, p=0.21 for comparison between 3.0 and 1.5 Tesla).
Figure 6.
3.0 and 1.5 Tesla k-t SENSE accelerated adenosine stress perfusion MR studies (3.0/1.0, flip angle, 15°) in a 65 year old patient with suspected CAD. Four sections in the double-oblique short axis orientation from base (left) to apex (right) were acquired. Both data sets have similar diagnostic content, but image quality at 3.0 Tesla is superior. The data sets show inferior and lateral ischemia in the basal and mid-cavity section and anteroseptal ischemia in the apical sections. Coronary angiography revealed three vessel disease with an occluded right coronary artery, a high-grade stenosis in the circumflex artery and sequential lesions in the left anterior descending artery.
Figure 7.

Tesla late-gadolinium enhanced (7.5/3.8, flip angle, 15°) (a) and k-t SENSE accelerated adenosine stress perfusion MR images (3.0/1.0, flip angle, 15°) (b) from a 58 year old patient with known CAD. One short axis slice at the apical level is shown. The patient had a previous apical myocardial infarction (arrows in a) and aneurysm. The very high spatial resolution and image contrast permits the detection of peri-infarct ischemia in the apical septum (arrow in b).
Discussion
This study has shown that k-t SENSE accelerated perfusion MR imaging at 3.0 Tesla is feasible and robust in volunteers and patients. Compared with 1.5 Tesla, SNR was improved although this was not statistically tested due to small sample size, while contrast enhancement was lower at 3.0 Tesla. Diagnostic accuracy to detect CAD was similar between the two field strengths. Compared with 2x SENSE, spatial resolution and image quality of k-t SENSE perfusion MR were higher and dark rim artifacts reduced.
It has previously been shown that k-t SENSE can be used to accelerate perfusion MR imaging at rest and at 1.5 Tesla (14). Our study demonstrates that the method can also be applied at 3.0 Tesla and during pharmacological stress. Only two of 37 patient studies (5%) had to be excluded from analysis, one because of a reconstruction error and one because of imaging artifacts. Image quality was high in volunteers and patients. k-t SENSE accelerated perfusion MR at 3.0 Tesla thus appears feasible for clinical use.
Similar to the previous volunteer study at 1.5 Tesla we invested the faster data acquisition into higher in-plane spatial resolution (14). Recently, Gebker et al. have employed a related method, k-t broad-use linear acquisition speed-up (k-t BLAST), to boost the temporal resolution of perfusion MR imaging at 1.5 Tesla (15) while maintaining in-plane spatial resolution at a conventional 2.6 × 2.6 mm2. The ability to invest the speed-up provided by k-t acceleration flexibly is a particular appeal of this method, but its best use needs to be established in a systematic comparison.
Compared with 1.5 Tesla, k-t SENSE perfusion-MR at 3.0 Tesla improved overall image quality in patients and yielded a doubled SNR. Two previous studies have reported similar SNR increases for 3.0 Tesla using conventional gradient-echo pulse sequences (1, 5). These results are in line with the theoretical expectations. In contrast to previous reports, we estimated noise from additional zero-flip angle noise maps, because the spatial dependence of noise amplification prevents conventional noise estimation in parallel imaging applications. We have found SNR estimations using difference methods unreliable owing to residual cardiac and respiratory motion between successive image frames.
Contrast enhancement ratios were lower at 3.0 Tesla than at 1.5 Tesla in our study. This finding may be related to the decreased relaxation rate of unenhanced tissue and the reduced relaxivity of the contrast agent with increasing field strength (16). Contrast at 3.0 Tesla may be further reduced by insufficient magnetization saturation due to increased B1 inhomogeneities and likely inaccuracies in power optimization (17). The use of adiabatic or multi-pulse saturation schemes seems therefore necessary at 3.0 Tesla and needs to be considered for future work. Notably, some previous reports have suggested the opposite effect of higher field strength on contrast enhancement, reporting increases at 3.0 Tesla (1,5). A reason for these discrepant observations could be that different contrast agents were used, which may behave differently at the two field strengths. We used the high-relaxivity agent Gadobutrolum in the current study, while previous reports used other agents (1,5).
The diagnostic accuracy of perfusion MR at 3.0 Tesla was similar to 1.5 Tesla with an area under the ROC curve of 0.89 and 0.80, respectively. A previous study by Cheng et al. reported comparable areas under the ROC curve of 0.87 and 0.78 for perfusion MR with a gradient echo pulse sequence at 3.0 Tesla and 1.5 Tesla, respectively (15). The high SNR, image quality and diagnostic accuracy achieved in these two studies suggests that perfusion MR may benefit in particular from higher magnetic field strength. Larger studies will be needed to confirm the trend for higher diagnostic accuracy seen in the current studies.
Compared with the 2x SENSE method, which afforded a more conventional spatial resolution, high-resolution k-t SENSE perfusion MR at 3.0 Tesla resulted in higher image quality and less dark rim artifacts in volunteers, similar to the previous study at 1.5 Tesla. At an average width of 1.6mm, these artifacts posed no diagnostic impediment. In patients the high spatial resolution and image quality helped to delineate the transmural extent of ischemia, subtle pathologies such as peri-infarct ischemia could be detected and multi-vessel disease reliably identified. As a result of the good image quality, diagnostic performance of visual perfusion analysis was high and the area under the ROC curve of 0.89 at 3.0 Tesla compares favorably with the published literature for both visual and quantitative perfusion MR analysis (6-9).
In this study we elected to acquire 4 short axis slices with a temporal resolution of 2 heart beats and restrict data acquisition to mid-systole and mid-diastole. At an acquisition time per slice of 120ms, it would have been possible to acquire more slices or achieve a higher temporal resolution. This approach was unrelated to the use of k-t SENSE and was chosen to minimize the effects of cardiac motion on the acquired data so that other sources of artifacts could be better evaluated. It is possible however that the low temporal resolution may have affected the diagnostic performance of the study.
Several authors have recently investigated the use of balanced steady state free precession (SSFP) pulse sequences for MR perfusion imaging and have reported SNR gains compared with other gradient echo methods. At 3.0 Tesla in particular, such pulse sequences are prone to artifacts, so that a non-balanced gradient echo application was chosen in the present work (18). The combination of k-t SENSE and balanced SSFP is however appealing and should be evaluated in future studies.
Our study was limited by the fact that due to differences in gradient performance, the spatial resolution at 3.0 Tesla was slightly higher than at 1.5 Tesla. This difference was corrected for in the SNR calculation. It is unlikely that the small difference had a substantial effect on other measurements.
Conclusions
k-t SENSE accelerated high-resolution perfusion MR at 3.0 Tesla is feasible and improves SNR and image quality compared with 1.5 Tesla. Artifacts and diagnostic accuracy are similar for the two field strengths. Compared with perfusion MR at lower spatial resolution, image quality is improved and artifacts are reduced.
Acknowledgments
Grant support
This work was supported by Philips Medical Systems, Best, The Netherlands and by a Wellcome Trust fellowship to Dr. Plein (WT078288). The authors thank Bayer Schering Pharma AG for financial support and for providing the contrast agent.
Footnotes
- k-space and time domain undersampling with sensitivity encoding (k-t SENSE) can be used to accelerate myocardial perfusion MR imaging at 3.0 Tesla.
- Compared with 1.5 Tesla, k-t SENSE accelerated perfusion MR imaging at 3.0 Tesla improves SNR and yields similar diagnostic accuracy to detect significant coronary artery stenosis.
- Using the acceleration provided by k-t SENSE to improve spatial resolution yields high image quality and reduces image artifacts compared with perfusion MR at lower resolution.
- The combination of k-t SENSE acceleration with acquisition at high field strength offers a promising tool for improved detection of coronary artery stenosis by perfusion MR imaging.
References
- 1.Cheng AS, Pegg TJ, Karamitsos TD, Searle N, Jerosch-Herold M, Choudhury RP, Banning AP, Neubauer S, Robson MD, Selvanayagam JB. Cardiovascular magnetic resonance perfusion imaging at 3-tesla for the detection of coronary artery disease: a comparison with 1.5-tesla. J Am Coll Cardiol. 2007;49:2440–9. doi: 10.1016/j.jacc.2007.03.028. [DOI] [PubMed] [Google Scholar]
- 2.Araoz PA, Glockner JF, McGee KP, et al. 3 Tesla MR imaging provides improved contrast in first-pass myocardial perfusion imaging over a range of gadolinium doses. J Cardiovasc Magn Reson. 2005;7:559–64. doi: 10.1081/jcmr-200060622. [DOI] [PubMed] [Google Scholar]
- 3.Gutberlet M, Noeske R, Schwinge K, et al. Comprehensive cardiac magnetic resonance imaging at 3.0 Tesla: feasibility and implications for clinical applications. Invest Radiol. 2006;41:154–67. doi: 10.1097/01.rli.0000195840.50230.10. [DOI] [PubMed] [Google Scholar]
- 4.Gutberlet M, Spors B, Grothoff M, et al. Comparison of different cardiac MRI sequences at 1.5 T/3.0 T with respect to signal-to-noise and contrast-to-noise ratios—initial experience. Rofo. 2004;176:801–8. doi: 10.1055/s-2004-813220. [DOI] [PubMed] [Google Scholar]
- 5.Theisen D, Wintersperger BJ, Huber A, Dietrich O, Reiser MF, Schonberg SO. Myocardial perfusion imaging with Gadobutrol: a comparison between 3 and 1.5 Tesla with an identical sequence design. Invest Radiol. 2007;42:499–506. doi: 10.1097/RLI.0b013e3180339981. [DOI] [PubMed] [Google Scholar]
- 6.Al-Saadi N, Nagel E, Gross M, Bornstedt A, Schnackenburg B, Klein C, Fleck E. Noninvasive detection of myocardial ischemia from perfusion reserve based on cardiovascular magnetic resonance. Circulation. 2000;101:1379–83. doi: 10.1161/01.cir.101.12.1379. [DOI] [PubMed] [Google Scholar]
- 7.Schwitter J, Nanz D, Kneifel S, Bertschinger K, Buchi M, Knusel PR, Marincek B, Luscher TF, von Schulthess GK. Assessment of myocardial perfusion in coronary artery disease by magnetic resonance: a comparison with positron emission tomography and coronary angiography. Circulation. 2001;103:2230–5. doi: 10.1161/01.cir.103.18.2230. [DOI] [PubMed] [Google Scholar]
- 8.Lee DC, Simonetti OP, Harris KR, Holly TA, Judd RM, Wu E, Klocke FJ. Magnetic resonance versus radionuclide pharmacological stress perfusion imaging for flow-limiting stenoses of varying severity. Circulation. 2004;6(110):58–65. doi: 10.1161/01.CIR.0000133389.48487.B6. [DOI] [PubMed] [Google Scholar]
- 9.Giang TH, Nanz D, Coulden R, Friedrich M, Graves M, Al-Saadi N, Luscher TF, von Schulthess GK, Schwitter J. Detection of coronary artery disease by magnetic resonance myocardial perfusion imaging with various contrast medium doses: first European multi-centre experience. Eur Heart J. 2004;25:1657–65. doi: 10.1016/j.ehj.2004.06.037. [DOI] [PubMed] [Google Scholar]
- 10.Pruessmann KP, Weiger M, Scheidegger MB, Boesiger P. SENSE: sensitivity encoding for fast MRI. Magn Reson Med. 1999 Nov;42(5):952–62. [PubMed] [Google Scholar]
- 11.Wiesinger F, Boesiger P, Pruessmann KP. Electrodynamics and ultimate SNR in parallel MR imaging. Magn Reson Med. 2004;52(2):376–90. doi: 10.1002/mrm.20183. [DOI] [PubMed] [Google Scholar]
- 12.Tsao J, Boesiger P, Pruessmann KP. k-t BLAST and k-t SENSE: dynamic MRI with high frame rate exploiting spatiotemporal correlations. Magn Reson Med. 2003 Nov;50(5):1031–42. doi: 10.1002/mrm.10611. [DOI] [PubMed] [Google Scholar]
- 13.Baltes C, Kozerke S, Hansen MS, Pruessmann KP, Tsao J, Boesiger P. Accelerating cine phase-contrast flow measurements using k-t BLAST and k-t SENSE. Magn Reson Med. 2005 Dec;54(6):1430–8. doi: 10.1002/mrm.20730. [DOI] [PubMed] [Google Scholar]
- 14.Plein S, Ryf S, Schwitter J, Radjenovic A, Boesiger P, Kozerke S. Dynamic contrast-enhanced myocardial perfusion MRI accelerated with k-t SENSE. Magn Reson Med. 2007;58:777–85. doi: 10.1002/mrm.21381. [DOI] [PubMed] [Google Scholar]
- 15.Gebker R, Jahnke C, Paetsch I, et al. MR myocardial perfusion imaging with k-space and time broad-use linear acquisition speed-up technique: feasibility study. Radiology. 2007;245:863–71. doi: 10.1148/radiol.2453061701. [DOI] [PubMed] [Google Scholar]
- 16.Trattnig S, Pinker K, Ba-Ssalamah A, Nöbauer-Huhmann IM. The optimal use of contrast agents at high field MRI. Eur Radiol. 2006;16:1280–7. doi: 10.1007/s00330-006-0154-0. [DOI] [PubMed] [Google Scholar]
- 17.Kim D, Gonen O, Oesingmann N, Axel L. Comparison of the effectiveness of saturation pulses in the heart at 3T. Magn Reson Med. 2008;59:209–15. doi: 10.1002/mrm.21423. [DOI] [PubMed] [Google Scholar]
- 18.Wieben O, Francois C, Reeder SB. O. Cardiac MRI of ischemic heart disease at 3T: potential and challenges. Eur J Radiol. 2008;65:15–28. doi: 10.1016/j.ejrad.2007.10.022. [DOI] [PubMed] [Google Scholar]