Abstract
Objective
The purpose of the study was to determine the clinical effects of anterior radical debridement on a series of patients with spontaneous spinal infection.
Methods
We retrospectively analyzed the clinical characteristics of 32 patients who underwent surgical treatment from January 2000 to December 2005 in our department. The average follow-up Period was 33.4 months (range, 6 to 87 months). Thirty-two patients presented with the following : 23 cases with pyogenic spondylitis, eight with tuberculous spondylitis and one with fungal spondylitis. The indications for surgery were intractable pain, failure of medical management, neurological impairment with or without an associated abscess, vertebral destruction causing spinal instability and/or segmental kyphosis.
Results
The study included 15 (46.9%) males and 17 (53.1%) females ranging in age from 26 to 75 years (mean, 53.1 years). Diabetes mellitus (DM) and pulmonary Tbc were the most common predisposing factors for pyogenic spondylitis and tuberculous spondylitis. Staphylococcus aureus (13%) was the main organism isolated. The most prevalent location was the lumbar spine (75%). Changes in the pain score, Frankel's classification, and laboratory parameters demonstrated a significant clinical improvement in all patients. However, there were recurrent infections in two patients with tuberculous spondylitis and inappropriate debridement and intolerance of medication and noncompliance. Autologous rib, iliac bone and allograft (fibular) were performed in most patients. However, 10 patients were grafted using a titanium mesh cage after anterior radical debridement. There were no recurrent infections in the 10 cases using the mesh cage with radical debridement.
Conclusion
The findings of this study indicate that surgery based on appropriate surgical indications is effective for the control of spinal infection and prevention of recurrence with anterior radical debridement, proper drug use and abscess drainage.
Keywords: Spinal infection, Spinal instrumentation, Surgical mesh
INTRODUCTION
Spinal infection is an inflammatory process around vertebral body, and it can be extended to epidural space, posterior elements and paravertebral soft tissues. Also, these encompass several entities involving pyogenic (bacterial), granulomatous (tuberculosis or fungal) or parasitic2). In general, hematogenous pyogenic infection of the spine has been reported as either spondylodiscitis or pyogenic osteomyelitis. The most common cause of spinal infections is pyogenic in nature that may present as a spondylitis, discitis, spondylodiscitis, pyogenic facet arthropathy, and epidural abscess. These may coexist in a same patient.
The most common organism reported in such infections is S. aureus. Spondylodiscitis can be treated with minimal invasive surgery, percutaneous transpedicle discectomy, anterior decompression, posterior instrumentation and CT guided percutaneous drainage according to the severity of the infection, presence of neurological deficits and the presence of concomitant psoas or paraspinal abscess. A primary epidural abscess can be treated by a laminectomy, posterior instrumentation and fusion. In addition, pyogenic facet arthropathy can be treated with CT guided percutaneous drainage and antibiotic irrigation. The principle treatment of tuberculous spondylitis is an antituberculous medication, posterior fusion with or without spinal instrumentation and anterior decompression.
Fungal infections generally are noncaseating, acid-fast, negative infections, and commonly occur as opportunistic infections in immunocompromised patients. Most patients do not require surgery and can improve with medical therapy. However, aggressive surgical debridement and stabilization along with antibiotic therapy may occasionally be required. Spinal infections account for less than 4% of all bony infections. However, delay in the diagnosis, misdiagnosis or inadequate treatment can lead to severe neurological deficits, long hospital stays and recurrence of infection. In addition, there are no definitive guidelines for antibiotic therapy, drug therapy after a biopsy, surgical methods or combination therapy. The main goal of treatment is to control the infection, prevent neurological complications and vertebral deformity. The purpose of this study was to analyze the clinical characteristics of surgically managed patients according to the surgical indications and assess the outcome of anterior radical debridement for spinal infections.
MATERIALS AND METHODS
This was a retrospective review of 32 consecutive cases of spontaneous spinal infections including pyogenic, tuberculous, and fungal spondylitis treated at a single institution from January 2000 to December 2005, with a minimum follow-up of 10 months. The average follow-up period was 33.4 months (range, 10 to 87 months). All records were reviewed for the level of spinal involvement, risk factors/comorbidities, culture results, surgical approach, neurological status, laboratory studies, recurrence and standard demographic data. All postoperative spinal infections were excluded from this study. The preoperative diagnosis was based on history, plain radiographs, computed tomography (CT) scans, magnetic resonance imaging (MRI), elevated WBC counts, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP).
Surgical therapy for spinal infections was necessary in cases with intractable pain and progression despite sufficient antibiotic therapy, sepsis, neurological impairment with or without an associated abscess, vertebral destruction causing spinal instability and/or segmental kyphosis. In this study, the neurological status was graded according to Frankel's classification. The clinical outcome (pain) was assessed using the visual analog scale (VAS). The radiographic analysis included the preoperative, immediate postoperative and last follow-up assessment of the sagittal profile (kyphotic angle) as measured by the angle between the endplate above and below the infected vertebrae. For statistical comparison, we performed a crosstabs test, and paired t-test using SPSS 12.O for Windows. In all cases, p values less than 0.05 were considered statistically significant.
The surgical technique
Twenty-six of 32 patients underwent surgical debridement and fixation by the anterior approach. Two patients received debridement and fixation by the posterior approach. The remaining four patients underwent debridement and abscess drainage by the posterior approach. The treatment proved to be an excellent method for the early stages of uncomplicated spondylodiscitis. However, it was contraindicated in advanced infections wherein excessive neurocompression or extensive bony destruction has developed1,13). In our study, most patients had advanced stage infections, extensive bone destruction, neural compression and neurological deficits that required anterior decompression. Postoperative kyphosis did not develop in two patients who had been treated with debridement and fixation by posterior approach.
The anterior approach including the transthoracic, thoracoabdominal and retroperitoneal procedures were performed when the infected tissue was mainly located at the anterior or middle column of the spine. The goal of surgery in such cases was to resect all infected and necrotic tissue with a radical debridement. A paravertebral abscess was excised or drained as completely as possible. The spinal canal was cleared of purulent material or infectious debris and then the operative defect was bridged by titanium mesh cages, filled and surrounded with autologous cancellous bone and/or allobone chips, an allograft or autograft and then the anterior instrumentation was added. When the main pathology was located in the posterior column, we performed a posterior approach including debridement, decompression and instrumentation.
When the main pathology was located at L5 and/or the L4 level, we performed a two-staged combined approach. First, an anterior column reconstruction using a bone graft or mesh cage inserted into the autograft was performed, after the corpectomy and discectomy, with radical debridement, decompression and abscess drainage by the anterior approach. About 1 week later, posterior instrumentation and bone grafting were added.
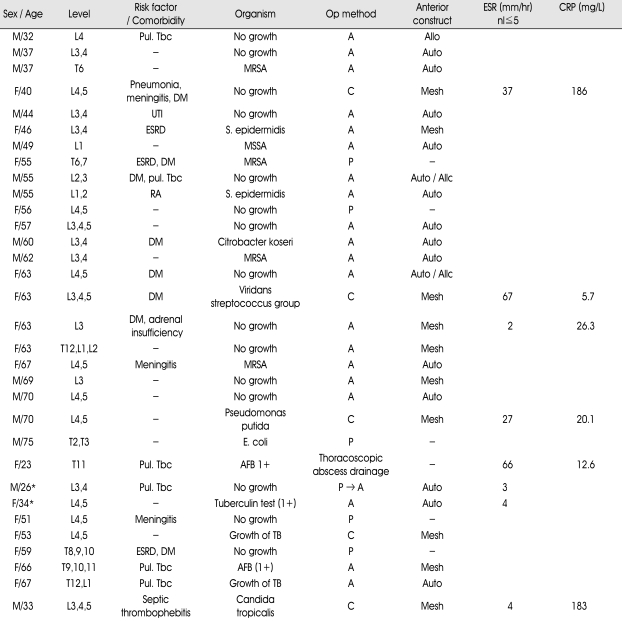
RESULTS (Table 1)
Table 1.
Summary of patient data
*recur, A : Anterior approach, P : Posterior approach, C : Combined approach. pul.Tbc : pulmonary tuberculosis, DM : Diabetes Mellitus, UTI : Urinary Tract Infection, ESRD : End Stage Renal Disease, RA : Rheumatoid Arthritis
Age and gender
The study included 15 (46.9%) male and 17 (53.1%) females patients ranging in age from 26 to 75 years (mean, 53.1 years). Patients in their fifties and sixties accounted for over 56% of cases and there were no significant gender differences. The average age for patients with pyogenic spondylitis was 54.5 years with slight male preponderance, 1.3:1. For tuberculous spondylitis, average age was 51.5 years and females were more common with a rate of 7 : 1. In addition, there was one male patient with fungal spondylitis. No patient was under the age of 20.
Predisposing factors for spinal infections
Most patients with pyogenic spondylitis had diabetes mellitus (7 cases) and other infections (5 cases) such as pneumonia, meningitis and septic thrombophlebitis. Pulmonary tuberculosis (6 cases) was present in most cases with tuberculous spondylitis.
Bacteriology of spinal infections
Of the 32 patients with spinal infections, pyogenic spondylitis and granulomatous spondylitis (including eight tuberculous and one fungal spondylitis) were identified in 23 and 9 patients each respectively. Tissue culture data were obtained in all patients; there were no bacterial isolates in 12 patients with pyogenic spondylitis and 6 patients with tuberculous spondylitis. The bacteriological findings revealed staphylococcus aureus as the most common strain in pyogenic spondylitis (four cases, p=0.017). Two patients with isolated tuberculous bacteria were being treated for pulmonary tuberculosis and four patients had a history of treatment for pulmonary tuberculosis.
Clinical symptoms and signs of spinal infection
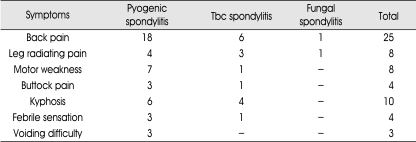
Most patients (78.1%) complained of localized pain around the infection site. Paraparesis was found on presentation in eight patients (25%) and eight patients (25%) had radiating pain. In addition to these clinical symptoms, febrile sensation and kyphosis were diagnosed in 4 and 10 patients each, respectively. The clinical signs and symptoms are detailed in Table 2.
Table 2.
Signs and symptoms of spinal infections
Distribution and number of spinal infections
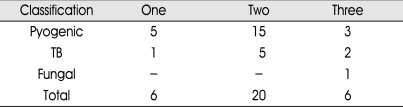
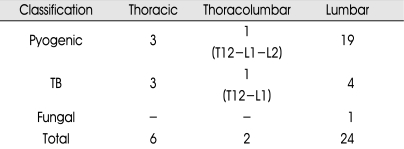
The most common location for the spinal infections was lumbar spine (75%), followed by thoracic spine (18.8%). The number of infected vertebral bodies varied from one to three. Two levels of vertebral body infection were identified in 20 patients (62.5%) followed by one infection site (in 18.8%) and three infection sites (in 18.7%). For pyogenic spondylitis, two and one infection site were identified in 65.2% and 21.8% of patients, respectively. For tuberculous spondylitis, two and three infection sites were identified in 62.5% and 25%, respectively. The number and distribution of spinal infections are detailed in Table 3, 4.
Table 3.
Number of infected vertebral bodies
Table 4.
Distribution of the spondylitis
Laboratory findings
The WBC counts (nl<10.000×106/L), ESR (nl≦5 mm/hr) and CRP (nl≦20 mg/L) were determined for all patients. Only 10 (43.5%) and one (12.5%) patient each, of the 32 patients, had elevated leukocyte counts for pyogenic and tuberculous spondylitis, respectively. There were fewer patients with an increased leukocyte count among the tuberculous spondylitis cases.
The CRP was elevated in 82.6% and 87.5% of patients with pyogenic spondylitis and tuberculous spondylitis, respectively. In addition, the ESR was elevated in 87% and 100% of the patients with pyogenic spondylitis and tuberculous spondylitis, respectively.
The WBC counts averaged 9,786/㎕ (range 5,830-15,820) before surgery, and 6,312/㎕ (range 3,480-8,480) at discharge. The CRP was 63.9 mg/L (range 5-256.9) before surgery, and 17.7 mg/L (range 0.5-53.8) at discharge. The ESR was 48.4 mm/hr (range 2-120) before surgery, and 31.5 mm/hr (range 2-87) at discharge. On discharge, only four patients showed normal ESR and 21 patients showed normal CRP. In general, after a 6-week regimen of IV antibiotics, the patients were discharged with improving clinical symptoms and laboratory findings. They were followed as outpatients on oral antibiotics.
Clinical results
Among the 32 surgically treated patients, 21 were managed by the anterior surgical approach, six by the posterior approach and five by a combined approach. We used autogenous iliac bone, rib and allobone grafts for the reconstruction of the anterior column. However, in 10 patients, we used a titanium mesh cage. The mesh cage was inserted in cases requiring multiple corpectomies and rigid corrections of deformities. Other reason for using mesh cage was that autologous bone grafts have limitations in cases with extensive bone loss and may result in donor site morbidity. In addition, we used the mesh cage for spinal infections based on the results of a recent study2,18) where it was shown that a mesh cage could control spinal infection and minimize risk of subsidence.
The mean visual analog scale (VAS) score was 8.3 before surgery and 2.7 after surgery. Prior to surgery, eight patients had motor weakness. Two patients were classified as Frankel type B, 1 as Frankel type C and five as Frankel type D. After surgery, the neurological status remained unchanged in one patient, and another seven patients improved by 1 Frankel grade. At the last follow-up, one patient was graded as Frankel type C, 1 patient as type D and 5 patients as type E.
Among patients treated surgically, two experienced a recurrence of infection after a complete course of treatment. They had worsening clinical features and laboratory findings, as well as abnormal MRI findings. Two patients had tuberculous spondylitis; one was being treated for three months previously for pulmonary tuberculosis. This patient was treated with an anterior approach with partial corpectomy using an autograft. During imaging evaluation, a psoas abscess was noted to have progressed compared to the previous imaging findings. The patient was treated by percutaneous drainage and antituberculous medication. The other patient was treated with antibiotics before presenting with a positive tuberculin test. After about 3-weeks of medication for the TB, the patient was treated with a posterior surgical approach because of an extensive epidural abscess including spondylitis.
This case had a recurrence 5 months after surgery and was treated with an anterior radical re-operation and TB medication. The cause of the recurrence was likely the partial corpectomy and an incomplete debridement initially; the decision not to perform a radical debridement, medication intolerance and patient noncompliance after discharge may also have contributed to the treatment failure. However, there was no recurrence of infection in the 10 cases where the titanium mesh cage was used with radical treatment.
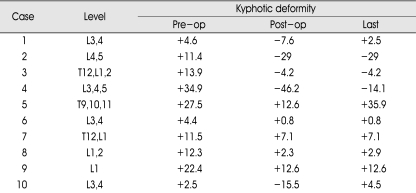
Radiographic results (Table 5, 6)
Table 5.
Change of sagittal alignment in patients with preoperative kyphotic deformity by anterior reconstruction
(+ : kyphotic angle, - : lordotic angle)
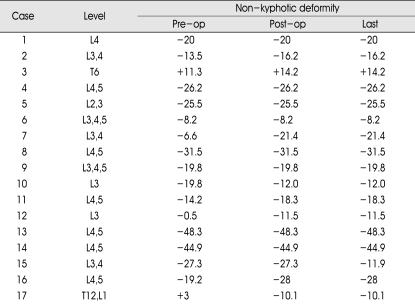
Table 6.
Change of sagittal alignment in patients with preoperative non-kyphotic deformity by anterior reconstruction
(+ : kyphotic angle, - : lordotic angle)
To assess the sagittal plane deformity, kyphotic angles were measured between the endplates above and below the infected vertebrae, and compared to normal sagittal angles of the same spinal segment4). If the angle demonstrated a lordotic curve (normal for the lumbar and cervical spine), the results were recorded as no kyphotic deformity. For the thoracic spine, comparison with normal sagittal angles of the same spinal segment4) were associated with bone rarefaction and vertebral body collapse. Ten patients had preoperative kyphotic deformities due to failure of the anterior column. Immediately postoperatively, all patients demonstrated correction of the kyphosis. At the last follow-up, three patients showed minimal loss of the lordotic angle and five patients did not show any change of the lordotic angle. Only two patients with osteoporosis showed progression of the kyphosis compared to the preoperative kyphosis, but they had no clinical symptoms. In 22 patients who did not show kyphosis preoperatively, the correction of the postoperative kyphosis was maintained. The average difference thus measured was 40.3° (range 12° to 102.9°) before surgery. After surgery, the average difference of the angle improved to 19° (range 0.1° to 40.8°). At the last follow-up, there were some loss of the surgical correction ; the mean difference in the angle was 27.7° (range 3.3° to 53.9°). A progression of kyphosis was present only with the anterior approach, and this was thought to be associated with subsidence in the anterior construct and osteoporosis.
The difference between the preoperative and immediate postoperative angles was statistically significant (p=0.009). In addition, the difference between the immediate postoperative evaluation and the last follow-up assessment of the angles was statistically significant (p=0.026).
DISCUSSION
Before the use of antibiotics and chemotherapy, mortality in patients with infections of the spine and contiguous tissue was 40-70 percent7). Advances in medical therapy since the 1960s have dramatically altered the natural history of these diseases. Today, spinal infections are relatively rare, accounting for only two to four percent of all osteomyelitis infections, and mortality is estimated to be 1-2%, depending on the patient group and the infectious agent7).
Many spinal infections are preceded by infectious elsewhere (e.g. urinary tract infection, meningitis, pneumonia, septic thrombophlebitis) as observed in the current study. Predisposing factors that compromise the immune system, such as diabetes mellitus, rheumatoid arthritis, end stage renal disease, or chronic steroid use, render the host more susceptible to spinal infections. In addition to these predisposing factors, intravenous drug abuse, ankylosing spondylitis and trauma may also play role in development of spondylodiscitis and epidural abscess1,3,6,8,13).
The most commonly isolated organism in this study was staphylococcus aureus (13%). This finding is different from most reported literature, with staphylococcus aureus accounting for 42% to 84% of the isolated organisms5,9,17,25,27,30,33,34), followed in frequency by Streptococcus species and gram-negative bacilli3,6,9,17,22,25,26,34). Negative cultures were obtained 52% of the time in the current study, a rate inconsistent with 20-30% of other investigations9,15,33). Three explanations have been given for this : concurrence of antibiotics administration before biopsy11), small-bore biopsy needle precluding a satisfactory retrieval of tissue samples31,32), and the natural healing of intervertebral disc infection as postulated by Fraser10). According to Fraser's theory10,11), vascular granulation tissue from the vertebral subchondral plate invades and resorbs the infected disc space, enabling the infected region to heal spontaneously after approximately 6 weeks, thus leading to negative cultures. This also explains why spinal infections can have a self-limited course in uncompromised hosts. In our study, most patients were previously treated with antibiotics before transfer to our hospital.
Most patients complained of pain at the infection site, buttock pain and radiating pain. In addition to these symptoms, the diagnosis was associated with kyphosis, febrile sensation and neurological deficits. Pyogenic spondylitis had a more aggressive course than tuberculous spondylitis and had more severe clinical symptoms. However, the symptoms presented and the pattern of progression varied according to the location of the infection.
The thoracic canal is very narrow and filled mostly with the spinal cord. In addition, the thoracic spine has a kyphotic angle. The blood supply to the spinal cord is not abundant, therefore, infection of the thoracic spine can result in serious neurological deficits such as paraplegia23,28,35). Among eight patients with thoracic spine infection in our study, five patients presented with severe complications such as motor weakness and voiding difficulty.
The WBC count typically is not elevated in patients with a spinal infection5,8,9,24,25,30,33,34). The leukocyte count was elevated in 43.5% and 12.5% of cases with pyogenic and tuberculous spondylitis, respectively. However, the ESR and CRP levels were more sensitive to the presence of a spinal infection (Elevated ESR=84% and CRP=84%). These parameters, when elevated, represent "red flag" for a more serious condition.
Tuberculous spondylitis is characterized by slowly progressive constitutional symptoms at early stages; symptoms include weakness, malaise, night sweats, fever, and weight loss. Pain is a late symptom associated with bone collapse and paralysis. Laboratory studies frequently suggest a chronic disease; findings include anemia, hypoproteinemia and mild ESR elevation.
The cornerstone of nonsurgical treatment, for uncomplicated pyogenic spondylitis, is intravenous (IV) antibiotics followed by oral antibiotics, along with spinal immobilization. Therapy of less than 4-week duration is associated with a 25% relapse rate30). Therefore, we used a 6-week treatment regimen with IV antibiotics followed by 6 weeks of oral medication to provide an extra margin of safety. Consideration of the site of infection is important for treatment decisions. For example, a spondylodiscitis requires a longer duration of treatment than a discitis and a spondylitis. The criteria for antibiotic therapy discontinuation were : 1) abatement of the spinal pain with disappearance of the inflammatory pattern; 2) normal body temperature; 3) normal CRP and/or ESR values; and 4) stabilization or improvement in the disk and vertebral abnormalities on plain radiographs20). For tuberculous spondylitis, antituberculous drugs including INH, RFP, EMB and PZA were used for 9 months of treatment after surgery. Normalization of the CRP occurred 1 or 2 weeks after surgery. Treatment was discontinued when the CRP was within normal limits and the clinical examination supported the absence of infection. The patients did well following these regimens.
The examination used to decide whether to discontinue IV antibiotics and TB medication included Gallium bone scan and MRI, as well as ESR and CRP, which were the most useful and cost-effective. Although Imaging studies are important for treatment decisions, they do not show the status of current infection; images suggesting infection remain after the active infection has been treated. Therefore, treatment may be considered successful when the ESR levels decrease to below 2/3 of the levels at the baseline, before treatment, discontinuation of the antibiotics when the ESR and CRP are within normal range.
In 1911, Hibbs14) described the treatment of tuberculous spinal infections by posterior fusion, but this method could not prevent progressive kyphosis. Many authors9,18,19,24,25) have shown the value of anterior surgical debridement in pyogenic and tuberculous spondylitis. Hodgson et al15) demonstrated the efficacy of surgical treatment on Potts disease and laid down the surgical principles of the treatment thereof. However, surgical treatment and the technique used are still controversial.
Generally, we believe that the posterior decompression and fusion approach is better than the anterior approach for the following reasons. The technique is simpler than the anterior method and the fusion rate is higher; in addition, it can be performed with a severe kyphosis, in a patient with a poor general condition and in cases where the anterior fusion has failed. However, the associated risks of the posterior approach include kyphosis and the possibility of incomplete removal of the infection1,7).
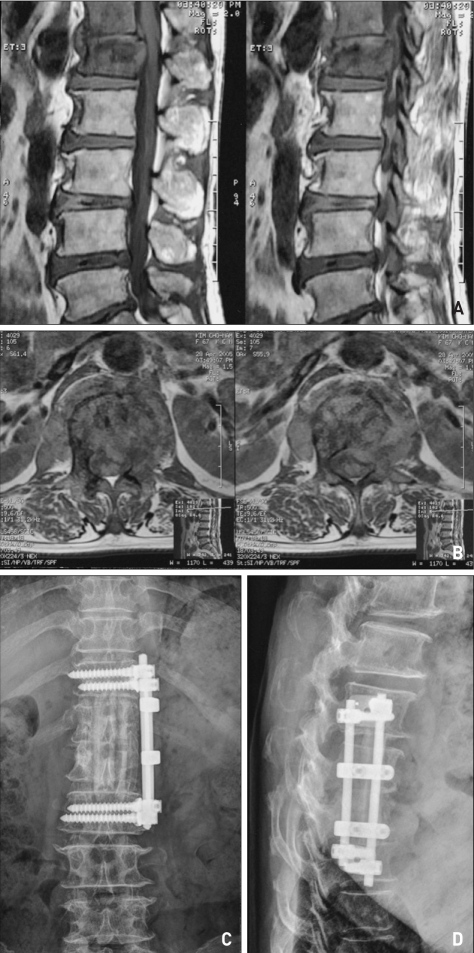
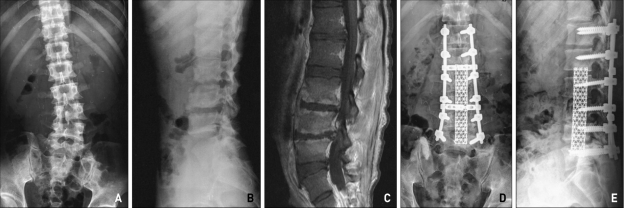
Anterior decompression and fusion with instrumentation is the procedure of choice for spondylodiscitis complicated by severe deformity and a neurological deficit, or by epidural abscess or granulation tissue causing neurocompression, producing a much better outcome than noninstrumented fusions with decompression or laminectomy alone27). In addition, radical debridement with resection of all infected and necrotic disc and bony tissue can be performed by anterior column support. In our cases, anterior column reconstruction was performed with autogenous bone (rib, iliac bone) and allograft (Fig. 1); however, in 10 patients the procedure was performed with a titanium mesh cage (Fig. 2). The goal of using the titanium mesh cage with bone grafts instead of a structural bone graft alone is that the cage with bone grafts may provide a more secure, accurate and dependable correction of the deformity than a bone graft alone. The cage provides a more rigid fixation construct and minimizes the risk of graft subsidence or dislodgement, that are well-documented complications when structural bone grafts alone are used. For treatment of a spinal infection, the instrumentation introduces a high risk for foreign material causing persistence and recurrence of infection and adherence of bacteria12). Many experimental studies suggest that Mycobacterium tuberculosis, unlike bacteria, has low adherence to stainless steel and forms less polysaccharide biofilms2). In our study, 7 pyogenic and 3 tuberculous spondylitis cases, with an inserted mesh cage, showed no recurrence of infection. In addition, reports have shown that if there is thorough removal of the infection and radical debridement, in addition to effective TB drug treatment and effective antibiotics, the recurrent risk for infection is very low after surgery9,14,18,19).
Fig. 1.
Tuberculous spondylitis with paraspinal and epidural abscess formation at the T12-L1 level on enhanced magnetic resonance imaging (A, B). Reconstruction using rib and allograft with solid fusion and stability with the anterior approach on plain radiographs (C, D).
Fig. 2.
Plain radiographs of pyogenic spondylitis with scoliosis, bony erosion at L3,4,5 (A, B). Magnetic resonance imaging of pyogenic spondylitis with severe enhanced vertebral body involvement, L3/4/5 (C). Postoperative plain radiograph of the combined approach (D, E). Mesh insertion and screw fixation were performed. The patient presented with lower extremity weakness. After four months of treatment, the patient could walk without assistance.
According to a recent study, the instrumentation used for surgery improved the spinal instability and resulted in early ambulation even with an active spinal infection2,20). In our study, two patients had a recurrence of infection. For these two patients, one patient was treated with posterior decompression and instrumentation. The other one was treated by an anterior decompression with bone fusion. The likely cause of the recurrence was incomplete debridement of infected tissue and/or incomplete drainage of a psoas abscess in the case where a posterior approach was performed. Another cause could have been insufficient TB medications. All patients with anterior decompression used for radical debridement and mesh grafting showed definite improvement; they were ambulatory with osseous union, had improvement of their kyphosis and absence of recurrent infection. The instrumentation provided most patients with the ability to ambulate within 5 days after surgery; this was because of the early spinal stability that resulted from prevention of displacement of the fusion graft. These patients had an early return to their activities of daily living.
CONCLUSION
Surgery in patients with the appropriate surgical indications is effective for the control of spinal infections, post-infection kyphosis and severe back pain with anterior radical debridement. Anterior radical debridement of infected tissue and medical treatment with effective agents for an appropriate duration improve the clinical outcome and reduce the recurrence of infection and unsatisfactory results. However, further studies with a long term follow-up and a larger patient population are needed to confirm our findings.
References
- 1.Alexander G, Hadjipavlov AG, Mader JT, Necessary JT, Muffoletto AJ. Hematogenous pyogenic spinal infections and their surgical management. Spine. 2000;25:1668–1679. doi: 10.1097/00007632-200007010-00010. [DOI] [PubMed] [Google Scholar]
- 2.Bak KH, Cheng JH, Kim JM, Kim CH, Kim SB. Titanium mesh cage for anterior stabilization in tuberculous spondylitis : is it safe? J Korean Neurosurg Soc. 2006;40:412–418. [Google Scholar]
- 3.Baker AS, Ojemann RG, Swartz MN, Richardson EP. Spinal epidural abscess. N Engl J Med. 1975;293:463–468. doi: 10.1056/NEJM197509042931001. [DOI] [PubMed] [Google Scholar]
- 4.Bernhardt M, Bridwell KH. segmental analysis of the sagittal plane alignment of the normal thoracic and lumbar spines and thoracolumbar junction. Spine. 1989;14:717–721. doi: 10.1097/00007632-198907000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Borowski AM, Crow WH, Hadjipavlou AG, Chaljub G, Mader J, Cesani F, et al. Interventional radiology case conference : the University of Texas Medical Branch. Percutaneous management of pyogenic spondylodiskitis. AJR Am J Roentgenol. 1998;170:1587–1592. doi: 10.2214/ajr.170.6.9609179. [DOI] [PubMed] [Google Scholar]
- 6.Collert S. Osteomyelitis of the spine. Acta Orthop Scand. 1977;48:283–290. doi: 10.3109/17453677708988770. [DOI] [PubMed] [Google Scholar]
- 7.Crenshaw AH. Campbell's Operative Orethopedics. 8th ed. Saint Louis: The CB Mosby company; 1992. pp. 3802–3823. [Google Scholar]
- 8.Digby JM, Kersley JB. Pyogenic nontuberculous spinal infection. J Bone Joint Surg Br. 1979;61:47–55. doi: 10.1302/0301-620X.61B1.370121. [DOI] [PubMed] [Google Scholar]
- 9.Emery SE, Chan DP, Woodward HR. Treatment of hematogenous pyogenic vetebral osteomyelitis with anterior debridement and primary bone grafting. Spine. 1989;14:284–291. [PubMed] [Google Scholar]
- 10.Fraser RD, Osti OL, Vernon-Roberts B. Discitis after discography. J Bone Joint Surg Br. 1987;68:26–35. doi: 10.1302/0301-620X.69B1.3818728. [DOI] [PubMed] [Google Scholar]
- 11.Fraser RD, Osti OL, Vernon-Roberts B. Iatrogenic discitis : the role of intravenous antibiotics in prevention and treatment : an experimental study. Spine. 1989;14:1025–1032. doi: 10.1097/00007632-198909000-00018. [DOI] [PubMed] [Google Scholar]
- 12.Gristina AG, Costerton JW. Bacterial adherence and glycocalyx and their role in musculoskeletal infection. Orthop Clin North Am. 1985;15:517–535. [PubMed] [Google Scholar]
- 13.Hadjipavlov AG, Crow WN, Borowski A, Mader JT, Adesokan A, Jensen RE. Percutaneous transpedicular discectomy and drainage in pyogenic spondylodiscitis. Am J Orthop. 1998;27:188–197. [PubMed] [Google Scholar]
- 14.Hibbs RA. An operation for progressive spinal deformities. NY Med J. 1911;93:1013. [Google Scholar]
- 15.Hodgson AR, Stock FE, Fang HS, Ong GB. The operative approach and pathological findings in 412 patients with Pott's disease of the spine. Br J Surg. 1960;48:172–178. doi: 10.1002/bjs.18004820819. [DOI] [PubMed] [Google Scholar]
- 16.Jung SW, Cho BS, Rhee DY. Surgical treatment of tuberculous spondylitis. J Korean Neurosurg Soc. 1997;26:384–393. [Google Scholar]
- 17.Kemp HBS, Jackson JW, Jeremiah JD, Hall AJ. Pyogenic infections occurring primarily in intervertebral discs. J Bone Joint Surg Br. 1973;55:698–714. [PubMed] [Google Scholar]
- 18.Kim BJ, Ko HS, Lim Y, Seo JG, Ju SG, Jeun TH. The clinical study of tuberculous spondylitis. J Korean Orthop. 1993;6:2221–2232. [Google Scholar]
- 19.Kim YH, Song JK, Shin H. A clinical analysis of surgically managed tuberculous spondylitis. J Korean Neurosurg Soc. 1997;26:223–234. [Google Scholar]
- 20.Kuklo TR, Potter BK, Bell RS, Moquin RR, Rosner MK. Single-stage treatment of pyogenic spinal infection with titanium mesh cages. J Spinal Disord Tech. 2006;19:376–382. doi: 10.1097/01.bsd.0000203945.03922.f6. [DOI] [PubMed] [Google Scholar]
- 21.Legrand E, Flipo RM, Guggenbuhl P, Masson C, Maillefert JF, Soubrier M, et al. Management of nontuberculous infectious discitis. Treatment used in 110 patients admitted to 12 teaching hospitals in France. J Bone Joint Spine. 2001;68:504–509. doi: 10.1016/s1297-319x(01)00315-3. [DOI] [PubMed] [Google Scholar]
- 22.Leys D, Lesoin F, Viaud C, Pasquier F, Rousseaux M, Jomin M, et al. Decreased morbidity from acute bacterial spinal epidural abscesses using computed tomography and nonsurgical treatment in selected patients. Ann Neurol. 1985;17:350–355. doi: 10.1002/ana.410170408. [DOI] [PubMed] [Google Scholar]
- 23.Menezes AH, Sonntag VKH. Principles of spinal surgery. New York: The McGraw-Hill company; 1996. pp. 1453–1464. [Google Scholar]
- 24.Musher DM, Thorsteinsson SB, Minuth JN, Luchi RJ. Vertebral osteomyelitis. Arch Intern Med. 1979;136:105–110. [PubMed] [Google Scholar]
- 25.Osenbach RK, Hitchon PW, Menezes AH. diagnosis and management of pyogenic vertebral osteomyelitis in adults. Surg Neurol. 1990;33:266–275. doi: 10.1016/0090-3019(90)90047-s. [DOI] [PubMed] [Google Scholar]
- 26.Poletti CE, Hesselink JR, Richardson EP, Mark VH, Boyd RJ, Shahani BT. Case records of the Massachusetts General Hospital : case 12-1982. N Engl J Med. 1982;306:729–737. doi: 10.1056/NEJM198203253061208. [DOI] [PubMed] [Google Scholar]
- 27.Rath SA, Neff U, Schneider O, Richter HP. Neurosurgical management of thoracic and lumbar vertebral osteomyelitis and discitis in adults : a review of 43 consecutive surgically treated patients. Neurosurgery. 1996;38:926–933. doi: 10.1097/00006123-199605000-00013. [DOI] [PubMed] [Google Scholar]
- 28.Rothman RH, Simeone FA. The Spine. 3rd ed. W.B Saunders Company; 1992. [Google Scholar]
- 29.Sapico FL. Microbiology and antimicrobial therapy of spinal infections. Orthop Clin North Am. 1996;27:9–13. [PubMed] [Google Scholar]
- 30.Sapico FL, Montgomerie JZ. Pyogenic vertebral osteomyelitis : report of nine cases and review of the literature. Rev Infect Dis. 1979;1:754–776. doi: 10.1093/clinids/1.5.754. [DOI] [PubMed] [Google Scholar]
- 31.Stoker DJ, Kissin CM. Percutaneous vertebral biopsy : a review of 135 cases. Clin Radiol. 1985;36:569–577. doi: 10.1016/s0009-9260(85)80235-x. [DOI] [PubMed] [Google Scholar]
- 32.Taylor TK, Dooley BJ. Antibiotics in the management of postoperative disc space infections. Aust N Z J Surg. 1978;48:74–77. doi: 10.1111/j.1445-2197.1978.tb05810.x. [DOI] [PubMed] [Google Scholar]
- 33.Torda AJ, Gottlieb T, Bradbury R. Pyogenic vertebral osteomyelitis : analysis of 20 cases and review. Clin Infect Dis. 1995;20:320–328. doi: 10.1093/clinids/20.2.320. [DOI] [PubMed] [Google Scholar]
- 34.Waldvogel FA, Papageorgiou PS. Osteomyelitis : the past decade. N Engl J Med. 1980;303:360–370. doi: 10.1056/NEJM198008143030703. [DOI] [PubMed] [Google Scholar]
- 35.Weinstein JN, Wiesel SW. The Lumbar Spine. W.B saunders Company; 1990. [Google Scholar]