Bizarre parosteal osteochondromatous proliferation (BPOP), as defined by Nora and colleagues1 in 1983 (also called Nora lesion), is a rare lesion. About 160 cases of BPOP have been presented in the literature to date. The lesion is an exophytic outgrowth from the cortical surface consisting of bone, cartilage and fibrous tissue. It usually affects the proximal and middle phalanges, and the metacarpal or metatarsal bones. The hands are 4 times more commonly affected than the feet;2 however, lesions in the long bones, skull, maxilla and metatarsophalangeal sesamoid have been reported.3–5 The lesion affects patients of any age, but most are in their 20s and 30s with no sex predilection.6 This benign lesion of the bone might be mistaken for malignant processes because of the high frequency of recurrence, the occasional quick growth and atypical histologic appearance. Along with a review of the literature, we discuss the cases of 3 patients with this rare lesion to illustrate the histologic, radiologic and clinical features as well as the different etiologic theories on BPOP.
Case reports
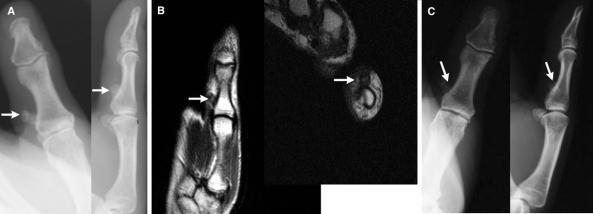
The first patient, a 51-year-old woman, presented to our outpatient clinic with pain and a tender palpable mass at the proximal phalanx of her left thumb (Fig. 1). She reported a recent increase in the size of the mass, and the pain was unremitting and unrelated to activity. She denied any history of injury.
FIG. 1. Imaging results for a 51-year-old woman with bizarre parosteal osteochondromatous proliferation at the proximal phalanx of her left thumb. (A) Anteroposterior and lateral radiographs showing a calcified mass (arrow) on the left thumb attached to the proximal phalanx without alteration of the underlying cortex. (B) Τ1-weighted magnetic resonance images (sagittal, axial) showing a low-signal lesion (arrow) extending from the thumb. There is normal signal intensity of the cortex and the bone marrow of the underlying bone. (C) Anteroposterior and lateral radiographs of an asymptomatic, stable local recurrence (arrow) 16 months after excision.
The second patient, a 37-year-old man, presented with a similar affliction at the proximal phalanx of the third finger on his left hand (Fig. 2). The mass had been slowly enlarging over the previous 6 months and had recently begun to cause discomfort. He had no history of trauma.
FIG. 2. Imaging results for a 37-year-old man with bizarre parosteal osteochondromatous proliferation. (A) Plain radiograph of the left hand showing a dense mass (arrow) extending from the dorsal radial aspect of the third proximal phalanx. (B) Radiograph taken 28 months postoperatively indicating that the man was free from local recurrence. (C) Light micrograph of the lesion consisting of a cartilaginous cap and a poorly developed zone of enchondral ossification (hematoxylin and eosin stain; original magnification × 100). (D) Light micrograph of the osteocartilaginous interface of the lesion showing disorganized cartilage with irregular ossification (hematoxylin and eosin stain; original magnification × 200).
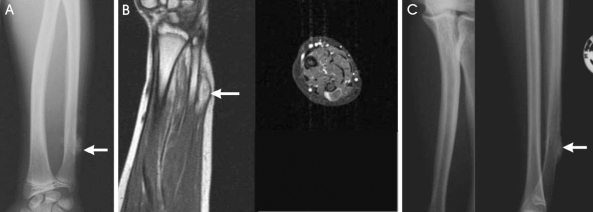
The third patient, a 16-year-old boy, reported pain in his left distal ulna without any traumatic episode. He had been examined by his family doctor. Eight weeks later, he experienced increasing local swelling and persistent pain in his left forearm (Fig. 3). He consulted his family doctor again and was referred to our outpatient clinic.
FIG. 3. Imaging results for a 16-year-old boy with bizarre parosteal osteochondromatous proliferation. (A) Anteroposterior radiograph showing a cortical-based bony excrescence (arrow) of the distal ulna diaphysis. (B) Τ1- and Τ2-weighted magnetic resonance images (sagittal, axial) showing an abnormal mass (arrow) extending around the medial aspect of the distal ulna. Bone marrow, medullary cavity and adjacent soft tissues appear normal. (C) Anteroposterior and lateral radiographs obtained 16 months after second excision.
Two radiologists experienced in musculoskeletal imaging retrospectively reviewed our findings. Preoperatively, the 3 patients underwent radiography, computed tomography (CT), magnetic resonance imaging (MRI), and 99Tc and 201Tl scintigraphy; the clinical and imaging findings were characteristic of BPOP. We performed an incisional biopsy in each patient to confirm the diagnosis. After biopsy, the 3 patients underwent intralesional excision.
Radiologic findings
In all 3 patients, radiographs showed calcified and osseous masses adjacent to the affected bones. The underlying bones had no cortical flaring or structural alteration. The CT scans showed intensely calcified and ossified masses with well defined margins. There was no continuity with the medullary canal of the bones from which the masses originated. The adjacent soft tissue appeared normal, in keeping with the diagnosis of BPOP. The MRI scans showed that the masses were isointense lesions with muscle on T1-weighted images. On T2-weighted images, the surface area of the lesions had high intensity, and the deeper area showed heterogeneous intensity. The 99Tc-and 201Tl scintigraphies demonstrated an abnormal uptake in the lesions of all 3 patients while the uptake in other parts of the body was normal.
Histologic findings
In all 3 patients, the resected specimens were well circumscribed masses. In cross-section, the lesions consisted of a cartilage cap and bone tissue. This structure seemed to correspond with the MRI findings. Histologically, the superficial area of the masses showed fibrocartilaginous tissue with high cellularity. Spindle shaped or stellate small chondrocytes were scattered in a myxoid stroma. The cells varied in size, and some were binucleated. The basal area was composed of immature bony trabeculae with high osteoblastic activity. These formed trabeculae stained mostly deep blue with hematoxylin and eosin (“blue bone”). The spindle cells were arranged loosely among the trabeculae, which were apparently formed by a process of enchondral ossification. The cells showed neither atypical mitoses nor cytological atypia.
Clinical results
Two of the patients experienced local recurrence; it occurred 4 months after excision in the 51-year-old woman and 10 months after excision in the 16-year-old boy. The woman experienced an asymptomatic, stable local recurrence that did not require further surgical intervention. At her most recent follow-up 16 months after surgery, she was free of pain and had no limitation of motion in her thumb. Owing to local affliction and evident progress, we performed a second intralesional excision in the 16-year-old boy. In his case, we excised the pseudocapsule over the cartilage cap and any periosteal tissue beneath the lesion. Sixteen months after the second excision, he was free of any evidence of local recurrence. The local recurrence had histology identical to that of the primary lesion.
At his most recent follow-up 28 months postoperatively, the 37-year-old man was free from local disorders and recurrence.
Discussion
Bizarre parosteal osteochondromatous proliferation is an uncommon reactive mineralizing mesenchymal lesion that typically affects the surfaces of bones in the hands and feet, usually the proximal and middle phalanges, and the metacarpal and metatarsal bones.7 These lesions have a remarkable tendency to recur: recurrence rates between 29% and 55% in a 2-year interval have been reported, and almost half of those patients have had a second recurrence.1,5,8 Nora and colleagues1 presented 35 cases of BPOP with 18 (51%) local recurrences. Meneses and colleagues5 reported a recurrence rate of 55% in a series of 65 patients, and Dhont and colleagues8 reported a recurrence rate of 29% in 24 patients. However, despite a high tendency to recur and a sometimes atypical histologic appearance, no malignant transformation, metastases, deaths or associated systemic diseases have been described so far in patients with BPOP.9
Although BPOP has a characteristic clinical and histologic appearance, it may be confused with other benign and malign lesions. Owing to the parosteal location, BPOP must be distinguished from parosteal osteosarcoma, which is rarely found in the hands and feet.10 The absence of cellular atypia helps to distinguish this lesion from osteosarcoma. The lesion might be mistaken for osteochondroma because of its surface location and cartilaginous component. Osteochondromas are extremely uncommon in the small bones of the distal extremities.2 They show the typical continuity with the medullary canal and the cartilage does not show any signs of atypia. Rybak and colleagues11 presented the cases of 4 patients with pathologically proven BPOP in which cortico–medullary continuity with the underlying bone was demonstrated on imaging. The absence of such a communication has been singled out as a critical imaging feature of BPOP. Rybak and colleagues11 indicated that BPOP could not be identified by radiologic features alone. Histopathologic examination is the best method to identify this lesion and should be performed for definite diagnosis.
Other benign, non-neoplastic lesions like periostitis ossificans may also simulate BPOP. This florid, reactive periostitis affects the bones of the hands in most patients, although other parts of the skeleton cannot be excluded. Turret exostosis is a dome-shaped parosteal bone proliferation located on the dorsal aspect of the phalanges. It has been proposed that BPOP, florid periostitis and turret exostosis are all part of the same lesional spectrum.12,13 The lesion may represent an intermediate lesion between florid reactive periostitis and turret exostosis. Florid reactive periostitis may progress to BPOP, as described by Dorfman and colleagues.12
Horiguchi and colleagues6 report the expression of basic fibroblastic growth factor in nearly all chondrocytes: chondromedulin-I in the tissue of the cartilaginous cap and vascular endothelial growth factor only in the large chondrocytes near the osteocartilaginous interface of the lesion. Their findings suggest that the processes occurring in the cartilaginous cap of BPOP are similar to those of enchondral ossification in the growth plate, concluding that BPOP is a reparative process after periosteal injury. Immunohistochemical and molecular analysis strengthened this assumption. However, most patients do not report a history of previous trauma. Moreover, if BPOP is a reactive lesion, its remarkable tendency to recur after excision is difficult to explain. Orui and colleagues7 reported the case of 1 patient wtih BPOP that occurred 2 years after bilateral leg erythema nodosum. Systemic or focal inflammation might have been responsible. Zambrano and colleagues9 presented the cases of 3 patients with subungual (Dupuytren) exotosis and of 2 patients with BPOP. Their findings of consistent chromosomal rearrangements indicate that BPOP is a neoplastic, rather than reactive, process. The cytogenetic analysis of 5 patients with BPOP by Nilsson and colleagues14 showed a balanced translocation t(1;17) (q32;q21). To investigate the specificity of this reciprocal translocation, they screened the karyotypes of more than 43 000 neoplasms and found no identical translocation. It seems to be a recurrent and pathogenetically significant aberration in BPOP. Endo and colleagues15 described the case of a 39-year-old woman with BPOP arising in the proximal phalanx of her third toe. Their cytogenentic analysis is comparable with the findings of Nilsson and colleagues.14 The occurrence of a translocation, as mentioned previously, supports the assumption that a neoplastic process may be the etiologic agent.
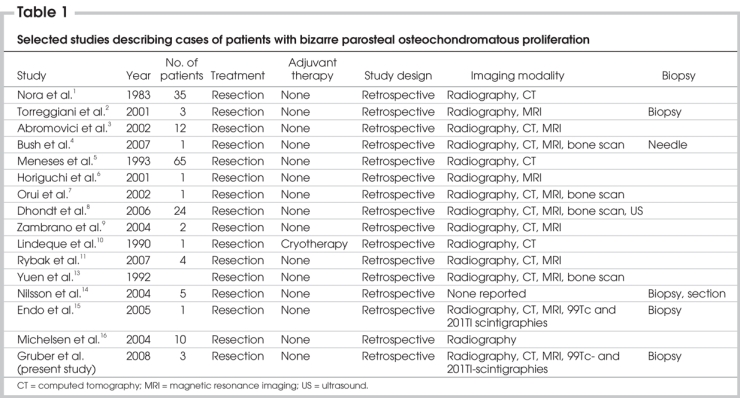
The true prevalence of BPOP is difficult to assess because most lesions are reported in case studies2–4,6,7,9,11,14–16 and because larger, mostly histologic studies1,5,8 are retrospective (Table 1). Therefore, further work is needed to fully elucidate the etiology of BPOP.
Table 1
Excision is the recommended therapy of symptomatic BPOP. Intralesional excision seems to have a great potential for local recurrence, but it preserves stability without decortication of the affected bone. En bloc negative margin excision by the excision of the pseudocapsule over the lesion and any periosteal tissue beneath the lesion and the decortication of any areas in the underlying host bone that appear abnormal has been shown to be beneficial in preventing local recurrence.16 Wide resection could possibly lead to segmental amputation because of the anatomic conditions in the long bones of the fingers and toes, and it cannot be recommended as first-line surgical treatment.
Owing to high local recurrence rates and a lack of adjuvant therapy options, the Nora lesion will continue to pose a challenge for orthopedic surgeons and clinical research. Therefore, treatment and follow-up care of this rare bone tumour should take place in cancer centres.
Contributors: Drs. Gruber, Giessauf, Leithner and Clar designed the study. Drs. Giessauf and Zacherl acquired the data, which Drs. Gruber, Bodo and Windhager analyzed. Drs. Gruber, Giessauf and Clar wrote the article, which Drs. Leithner, Zacherl, Bodo and Windhager reviewed. All authors provided final approval for publication.
Competing interests: None declared.
Accepted for publication May 8, 2008
Correspondence to: Dr. C. Giessauf, Department of Surgery, District Hospital of Weiz, Franz-Pichler Strasse 85, 8160 Weiz, Austria; christian_giessauf@yahoo.de
References
- 1.Nora FE, Dahlin DC, Beabout JW. Bizarre parosteal osteochondromatous proliferations of the hands and feet. Am J Surg Pathol 1983;7:245-50. [DOI] [PubMed]
- 2.Torreggiani WC, Munk PL, Al-Ismail K, et al. MR imaging features of bizarre parosteal osteochondromatous proliferation of bone (Nora's lesion). Eur J Radiol 2001;40:224-31. [DOI] [PubMed]
- 3.Abramovici L, Steiner GC. Bizarre parosteal osteochondromatous proliferation (Nora's lesion): a retrospective study of 12 cases, 2 arising in long bones. Hum Pathol 2002;33:1205-10. [DOI] [PubMed]
- 4.Bush JB, Reith JD, Meyer MS. Bizarre parosteal osteochondromatous proliferation of the proximal humerus: case report. Skeletal Radiol 2007;36:535-40. [DOI] [PubMed]
- 5.Meneses MF, Unni KK, Swee RG. Bizarre parosteal osteochondromatous proliferation of bone (Nora's lesion). Am J Surg Pathol 1993;17:691-7. [DOI] [PubMed]
- 6.Horiguchi H, Sakane M, Matsui M, et al. Bizarre parosteal osteochondromatous proliferation (Nora's lesion) of the foot. Pathol Int 2001;51:816-23. [DOI] [PubMed]
- 7.Orui H, Ishikawa A, Tsuchiya T, et al. Magnetic resonance imaging characteristics of bizarre parosteal osteochondromatous proliferation of the hand: a case report. J Hand Surg [Am] 2002;27:1104-8. [DOI] [PubMed]
- 8.Dhondt E, Oudenhoven L, Khan S, et al. Nora's lesion, a distinct radiological entity? Skeletal Radiol 2006;35:497-502. [DOI] [PubMed]
- 9.Zambrano E, Nose V, Perez-Atayde AR, et al. Distinct chromosomal rearrangements in subungual (Dupuytren) exostosis and bizarre parosteal osteochondromatous proliferation (Nora lesion). Am J Surg Pathol 2004;28:1033-9. [DOI] [PubMed]
- 10.Lindeque BG, Simson IW, Fourie PA. Bizarre parosteal osteochondromatous proliferation of a phalanx. Arch Orthop Trauma Surg 1990;110:58-60. [DOI] [PubMed]
- 11.Rybak LD, Abramovici L, Kenan S, et al. Cortico-medullary continuity in bizarre parosteal osteochondromatous proliferation mimicking osteochondroma on imaging. Skeletal Radiol 2007;36: 829-34. [DOI] [PubMed]
- 12.Dorfman HD, Czerniak B. Bone tumors. St. Louis (MO): Mosby; 1998.
- 13.Yuen M, Friedmann L, Orr W, et al. Proliferative periosteal processes of phalanges; a unitary hypothesis. Skeletal Radiol 1992; 21:301-3. [DOI] [PubMed]
- 14.Nilsson M, Domanski HA, Mertens F, et al. Molecular cytogenetic characterization of recurrent translocation breakpoints in bizarre parosteal osteochondromatous proliferation (Nora's lesion). Hum Pathol 2004;35:1063-9. [DOI] [PubMed]
- 15.Endo M, Hasegawa T, Tashiro T, et al. Bizarre parosteal osteochondromatous proliferation with a t(1;17) translocation. Virchows Arch 2005;447:99-102. [DOI] [PubMed]
- 16.Michelsen H, Abramovici L, Steiner G, et al. Bizarre parosteal osteochondromatous proliferation (Nora's lesion) in the hand. J Hand Surg [Am] 2004;29:520-5. [DOI] [PubMed]