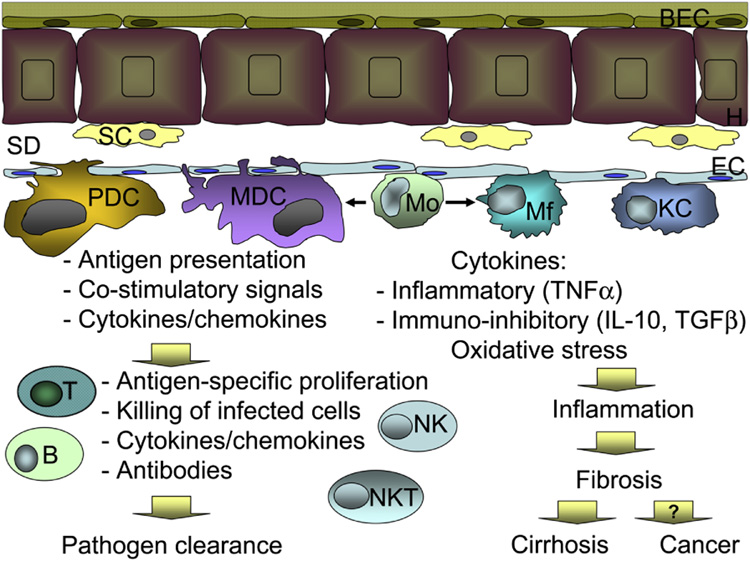
Figure 1. Schematic representation of the immune cells in the liver.
Hepatocytes (H) are lined with biliary endothelial cells (BEC) on the portal facet and stellate cells (SC) in the space of Disse (SD). Endothelial cells (EC) separate the space of Disse from the blood flow. Dendritic cells of plasmacytoid (PDC) and myeloid (MCD) origin, monocytes (Mo), macrophages (Mf) and Kupffer cells (KC) are located in close proximity to endothelial cells. Blood monocytes are immature and can give rise to macrophages or myeloid dendritic cells, depending on the environment. Upon encountering pathogens, derived from either blood stream or infected hepatocytes, MDC and PDCs are primarily responsible for antigen presentation to adaptive immune cells and creation of favorable milieu for antigen presentation, including production of cytokines and availability of co-stimulatory molecules. In turn, adaptive immune cells, including T and B-lymphocytes, natural killer (NK) and NKT cells react with antigen-specific proliferation, cytotoxicity, and production of soluble mediators, such as antibodies or cytokines. Collectively, these events lead to pathogen elimination. Monocytes, macrophages and Kupffer cells also recognize pathogens, however in contrast to dendritic cells, they have a less pronounced effect on the adaptive immunity. Mo, Mf and KCs are potent producers of inflammatory and immunoregulatory cytokines and are powerful sources of free radical with oxidative capacity, thus lead to initiation and maintenance of tissue inflammation. Chronic inflammation, in addition to direct pathogen recognition, activates stellate cells, which in turn produce collagen and favor development of liver fibrosis. At the end stage liver disease, chronic inflammation and fibrosis drive progression to cirrhosis and possibly favor neoplastic transformation and liver cancer.