Abstract
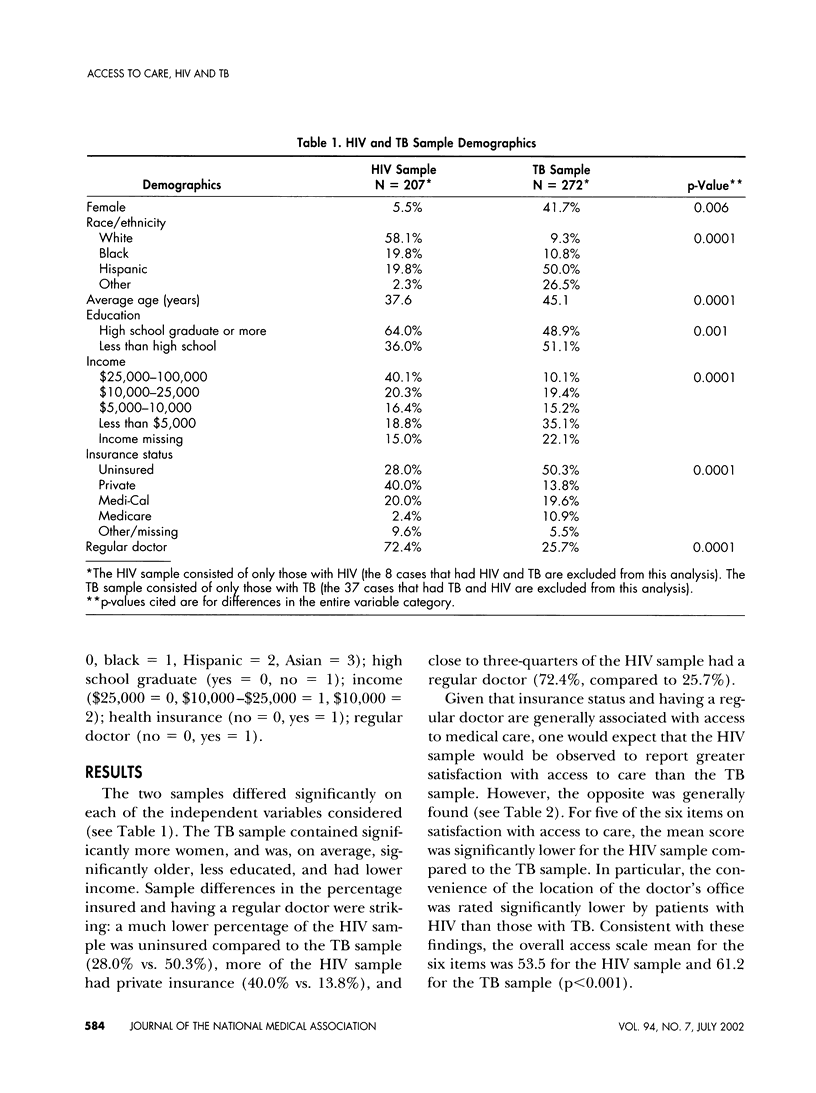
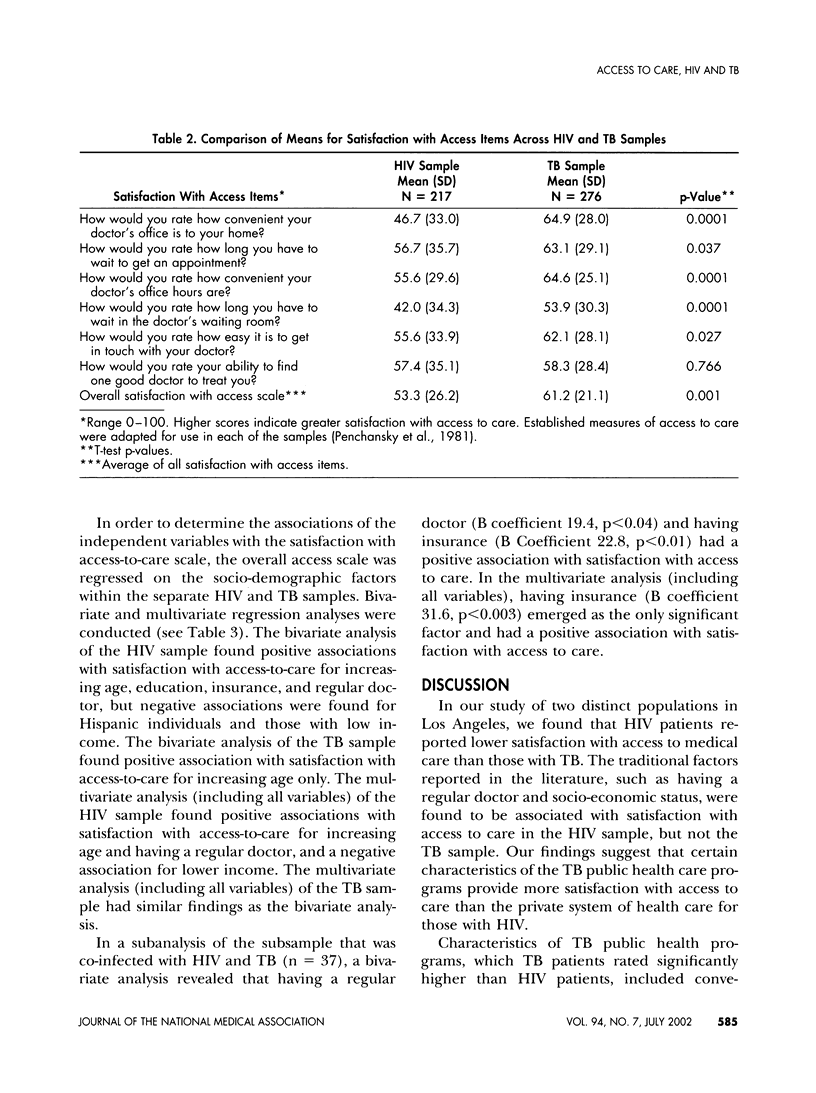
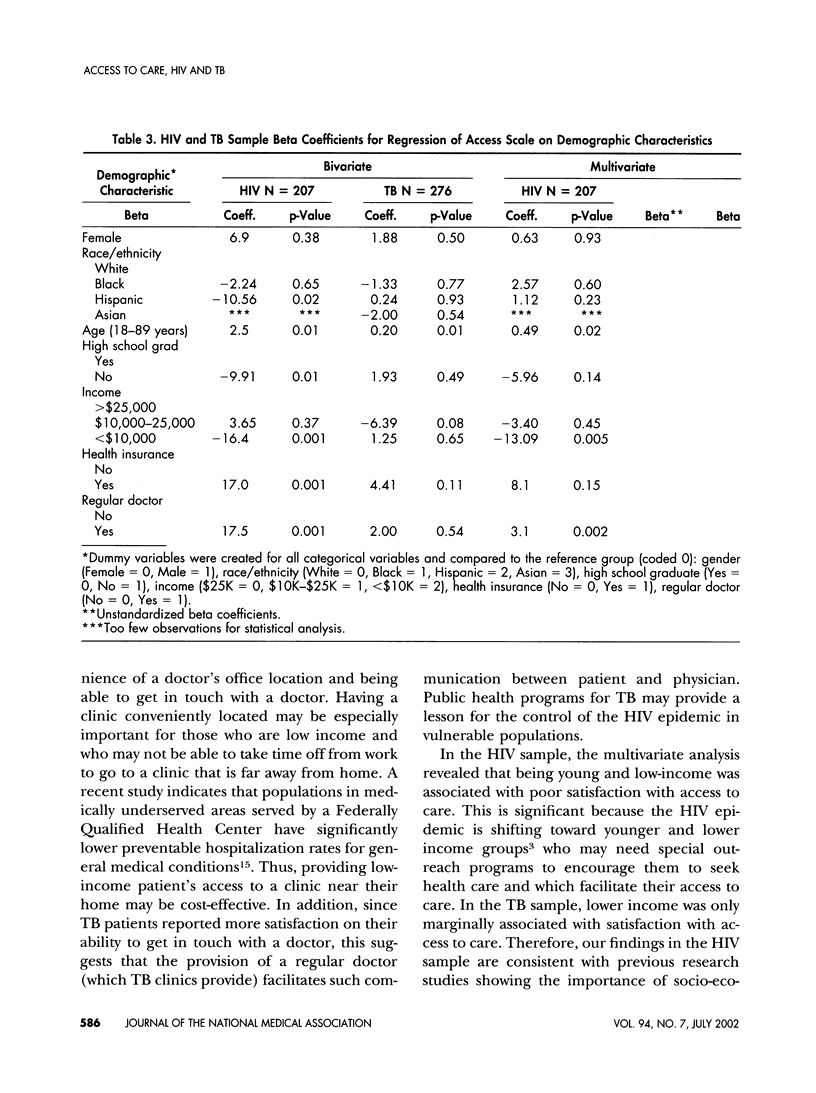
PURPOSE: To examine satisfaction with access to health care in two populations, one with HIV and one with TB, and examine the effect of having a regular doctor and sociodemographic characteristics. DESIGN: Cross-Sectional survey. PATIENTS: A sample of HIV inpatients hospitalized at seven Los Angeles sites (N = 217) and TB outpatients chosen randomly from the Los Angeles County TB Registry Census (N = 313). ANALYSIS: We performed bivariate and multivariate regression analyses of satisfaction with access to care on gender, race/ethnicity, age, education, income, insurance, and having a regular doctor. MAIN OUTCOME MEASURES: A six-item scale of satisfaction with access to care (range 0-100; Cronbach's alpha 0.87). RESULTS: The mean satisfaction with access score for the HIV sample was significantly lower than the TB sample (53.5 vs. 61.2, p<0.001). The HIV sample multivariate analysis (including all the variables) showed that increasing age (p<0.021 and having a regular doctor (p<0.002) were associated with better access, and that low income (p<0.005) was associated with poor access. In the TB sample analysis, only increasing age was associated with better satisfaction with access to care (p< 0.01). CONCLUSION: HIV patients receiving care in the private sector reported less satisfaction with access to care compared to TB patients receiving care in the public health sector. The traditional factors of socio-economic status and having a regular doctor were associated with satisfaction with access-to-care in the HIV sample but not the TB sample. Our findings suggest that certain characteristics of the TB public health programs may explain these differences and suggests that, perhaps, the existence of a similar public health program for vulnerable low-income populations with HIV would improve their satisfaction with access, as well.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brown E. R. Trends in health insurance coverage in California, 1989-1993. Health Aff (Millwood) 1996 Spring;15(1):118–130. doi: 10.1377/hlthaff.15.1.118. [DOI] [PubMed] [Google Scholar]
- Cunningham W. E., Hays R. D., Ettl M. K., Dixon W. J., Liu R. C., Beck C. K., Shapiro M. F. The prospective effect of access to medical care on health-related quality-of-life outcomes in patients with symptomatic HIV disease. Med Care. 1998 Mar;36(3):295–306. doi: 10.1097/00005650-199803000-00007. [DOI] [PubMed] [Google Scholar]
- Cunningham W. E., Mosen D. M., Hays R. D., Andersen R. M., Shapiro M. F. Access to community-based medical services and number of hospitalizations among patients with HIV disease: are they related? J Acquir Immune Defic Syndr Hum Retrovirol. 1996 Dec 1;13(4):327–335. doi: 10.1097/00042560-199612010-00005. [DOI] [PubMed] [Google Scholar]
- Derose K. P., Baker D. W. Limited English proficiency and Latinos' use of physician services. Med Care Res Rev. 2000 Mar;57(1):76–91. doi: 10.1177/107755870005700105. [DOI] [PubMed] [Google Scholar]
- Diamant A. L., Brook R. H., Fink A., Gelberg L. Assessing use of primary health care services by very low-income adults in a managed care program. Arch Intern Med. 2001 May 14;161(9):1222–1227. doi: 10.1001/archinte.161.9.1222. [DOI] [PubMed] [Google Scholar]
- Diaz T., Chu S. Y., Conti L., Nahlen B. L., Whyte B., Mokotoff E., Shields A., Checko P. J., Herr M., Mukhtar Q. Health insurance coverage among persons with AIDS: results from a multistate surveillance project. Am J Public Health. 1994 Jun;84(6):1015–1018. doi: 10.2105/ajph.84.6.1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francis D. P., Anderson R. E., Gorman M. E., Fenstersheib M., Padian N. S., Kizer K. W., Conant M. A. Targeting AIDS prevention and treatment toward HIV-1-infected persons. The concept of early intervention. JAMA. 1989 Nov 10;262(18):2572–2576. [PubMed] [Google Scholar]
- Gelberg L., Andersen R. M., Leake B. D. The Behavioral Model for Vulnerable Populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000 Feb;34(6):1273–1302. [PMC free article] [PubMed] [Google Scholar]
- Guendelman S., Wagner T. H. Health services utilization among Latinos and white non-Latinos: results from a national survey. J Health Care Poor Underserved. 2000 May;11(2):179–194. doi: 10.1353/hpu.2010.0719. [DOI] [PubMed] [Google Scholar]
- Higgs Z. R., Bayne T., Murphy D. Health care access: a consumer perspective. Public Health Nurs. 2001 Jan-Feb;18(1):3–12. doi: 10.1046/j.1525-1446.2001.00003.x. [DOI] [PubMed] [Google Scholar]
- Merzel C. Gender differences in health care access indicators in an urban, low-income community. Am J Public Health. 2000 Jun;90(6):909–916. doi: 10.2105/ajph.90.6.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller L. G., Asch S. M., Yu E. I., Knowles L., Gelberg L., Davidson P. A population-based survey of tuberculosis symptoms: how atypical are atypical presentations? Clin Infect Dis. 2000 Feb;30(2):293–299. doi: 10.1086/313651. [DOI] [PubMed] [Google Scholar]
- Mosen D. M., Wenger N. S., Shapiro M. F., Andersen R. M., Cunningham W. E. Is access to medical care associated with receipt of HIV testing and counselling? AIDS Care. 1998 Oct;10(5):617–628. doi: 10.1080/09540129848479. [DOI] [PubMed] [Google Scholar]
- Porco T. C., Small P. M., Blower S. M. Amplification dynamics: predicting the effect of HIV on tuberculosis outbreaks. J Acquir Immune Defic Syndr. 2001 Dec 15;28(5):437–444. doi: 10.1097/00042560-200112150-00005. [DOI] [PubMed] [Google Scholar]
- Sendi P., Palmer A. J., Gafni A., Battegay M. Highly active antiretroviral therapy: pharmacoeconomic issues in the management of HIV infection. Pharmacoeconomics. 2001;19(7):709–713. doi: 10.2165/00019053-200119070-00001. [DOI] [PubMed] [Google Scholar]


