Abstract
Contingency management (CM) for drug abstinence has been applied to individuals independently even when delivered in groups. We developed a group CM intervention in which the behavior of a single, randomly selected, anonymous individual determined reinforcement delivery for the entire group. We also compared contingencies placed only on cocaine abstinence (CA) versus one of four behaviors (CA, treatment attendance, group CM attendance, and methadone compliance) selected randomly at each drawing. Two groups were formed with 22 cocaine-dependent community-based methadone patients and exposed to both CA and multiple behavior (MB) conditions in a reversal design counterbalanced across groups for exposure order. The group CM intervention proved feasible and safe. The MB condition improved group CM meeting attendance relative to the CA condition.
Keywords: cocaine abstinence, cocaine abuse, contingency management, drug abuse, treatment attendance
Contingency management (CM) interventions that target urinalysis-verified drug abstinence are among the most effective methods for initiating and maintaining abstinence during drug abuse treatment. In fact, CM was the only treatment identified as being empirically based for both opiate and cocaine drug use disorders by an American Psychological Association independent task force (Chambless et al., 1998; Chambless & Ollendick, 2001).
Stitzer et al. were among the first to use CM procedures for drug abuse treatment, demonstrating the efficacy of CM for reducing supplemental drug use in methadone treatment (Stitzer, Bigelow, & Liebson, 1979, 1980; Stitzer, Bigelow, Liebson, & Hawthorne, 1982). Procedures usually involved collecting two to three urine samples weekly and delivering methadone take-home doses contingent on a drug-negative urine sample (e.g., McCaul, Stitzer, Bigelow, & Liebson, 1984; Stitzer et al., 1982). More recent studies have addressed cocaine use with a token system in which vouchers are exchanged for a variety of goods and services, allowing for a wider selection of reinforcers (Silverman et al., 2007). This voucher-based system was originally developed by Higgins et al. (1993, 1994, 1995) for the drug-free treatment of cocaine abusers and has been extended to a variety of drug-abusing populations, including methadone patients (Silverman et al., 1996), homeless men (Milby et al., 1996, 2003), dually diagnosed substance users (Helmus, Saules, Schoener, & Roll, 2003; Shaner et al., 1997), and women in specialized treatment programs (Elk, Mangus, Rhoades, Andres, & Grabowski, 1998; Jones, Haug, Silverman, Stitzer, & Svikis, 2001; Jones, Haug, Stitzer, & Svikis, 2000; Svikis, Lee, Haug, & Stitzer, 1997). Although CM is recognized as an effective intervention for drug use, community-based treatment providers perceive it as inconsistent with their usual practices, too costly, and too complex (cf. Fals-Stewart & Birchler, 2001; Kirby, Amass, & McLellan, 1999; Kirby, Benishek, Dugosh, & Kerwin, 2006). We surveyed 308 community drug and alcohol treatment providers asking about their perceptions regarding the use of CM and identified several prominent treatment provider objections (Kirby et al., 2006). One objection involved the practice of targeting only one behavior in a CM intervention. Treatment providers usually are concerned that in addition to decreasing drug use, patients work toward treatment goals, attend group sessions, and behave respectfully toward staff and each other. However, a meta-analysis of CM interventions in substance abuse treatment (Griffith, Rowan-Szal, Roark, & Simpson, 2000) noted that targeting a single drug (vs. multiple drugs) resulted in significantly larger effect sizes, suggesting that targeting multiple behaviors simultaneously might be less effective than targeting only one.
Modality of treatment delivery is another inconsistency between CM and the practices of usual care. Group therapy is the most common mode of treatment delivery in community treatment settings (McLellan, 2001), but like the majority of the behavior therapies that have been developed and tested in clinical trials, CM for drug abstinence usually has been delivered individually. Our examination of the drug abuse treatment literature revealed only a few studies in which group CM was used. Petry, Martin, and Finocche (2001) and Petry, Martin, and Simcic (2005) delivered incentives to each individual based on his or her own behavior, even though the incentives were delivered in a group setting. Group CM improved outcomes relative to standard treatment. Liebson, Cohen, and Faillace (1972) used group CM to produce a 20% decrease in frequency of major offenses of alcoholic men living and working in a locked hospital unit. If any group member engaged in inappropriate behavior, a fine was imposed on the entire group.
In other settings there has been a long tradition of using group CM to initiate and maintain change in a variety of behaviors (e.g., Tingstrom, Sterling-Turner, & Wilczynski, 2006). Three types of group CM procedures are described in the literature: (a) independent group CM, (b) dependent group CM, and (c) interdependent group CM (Litow & Pumroy, 1975).
In independent group CM, the same contingency operates for all members of the group, but each member individually accesses reinforcers based solely on his or her own behavior. Petry's studies (Alessi, Hanson, Wieners, & Petry, 2007; Petry & Martin, 2002; Petry et al., 2001, 2005) are examples of independent group CM, in which participants meet as a group but each member earns reinforcement independently of the others.
In dependent group CM, all members of the group receive the same consequence, but the contingency is applied to the behavior of one or more selected group members. For example, the contingency might be set such that the individual in the group who has the poorest treatment attendance earns gift certificates for the entire group each time he or she attends treatment. In this way, all members of the group are dependent on the selected member's performance, and there is essentially no contingency placed directly on the behavior of most members.
In interdependent group CM, each group member's behavior contributes to the determination or has the potential to determine the consequence for the entire group. Interdependent group CM has several variations. In one variant, every member of the group must perform to a criterion for all members to receive the incentive. Liebson et al. (1972) is an example of this variant, in that every member of the group had to have zero infractions for the group to avoid a fine. In a second variant of interdependent group CM, the mean of all members' performances must meet a criterion for the entire group to earn reinforcement. For example, the contingency might specify that 70% of the group members must provide a drug-free urine specimen for the group to earn a prize. In a third variant, the performance of a single, randomly selected group member must meet a criterion for the entire group to earn reinforcement. For example, the urine results of each group member might be recorded on a separate piece of paper and placed in a bowl. One paper is drawn from the bowl, and if it indicates the urine was drug free, all group members earn a prize. In interdependent group CM, the identity of the randomly selected member is not known in advance, and as such, each group member has the potential to determine reinforcement delivery up to the point when the single group member is randomly selected. This differs from a dependent group CM contingency in which the single member who determines the consequence for the entire group is fixed in advance, and as such, the behaviors of other group members do not have the potential to influence reinforcer delivery.
Based on general research on operant interventions, one might hypothesize that dependent and interdependent group CM should be less effective than individual group CM and possibly detrimental relative to no contingencies. This is because the programmed consequences do not correspond directly to each individual's behavior, and individuals who have recently used drugs may receive reinforcement. Somewhat paradoxically, research in areas other than drug abuse has repeatedly demonstrated that dependent and interdependent group CM interventions are better than no contingencies and are at least equal and often superior to individual CM in producing positive change in the target behavior (Brown & Redmon, 1990; Kelshaw-Levering, Sterling-Turner, Henry, & Skinner, 2000; Lew, Mesch, Johnson, & Johnson, 1986; Lloyd, Eberhardt, & Drake, 1996; Mawhinney & Fellows-Kubert, 1999; Pedalino & Gamboa, 1974; Popkin & Skinner, 2003; Shapiro & Goldberg, 1990; Speltz, Shimamura, & McReynolds, 1982; Theodore, Bray, Kehle, & Jenson, 2001; Turco & Elliott, 1990). One possible reason may be the emergence of corollary or nontargeted cooperative and supportive behaviors, which have been noted in group CM studies conducted with children and adults in a variety of settings (Gresham & Gresham, 1982; Hayes, 1976; Williamson, Williamson, Watkins, & Hughes, 1992). Participants in group CM report that they are influenced more by their peers in dependent and interdependent group CM than they are in independent group CM (McReynolds, Gange, & Speltz, 1981). Unfortunately, negative corollary behaviors such as threatening, scolding, and coercion directed toward poorly performing individuals also have been noted during group CM (e.g., Greenwood & Hops, 1981), but negative effects can be minimized when individual performances are not known to others (McLaughlin, 1981) and the components of the group contingency are selected randomly (e.g., Cashwell, Skinner, Dunn, & Lewis, 1998). For example, recent applications of group CM in classrooms have used conditions that randomly select components such as the target behavior (e.g., disruptions, task completion), the behavioral criteria (i.e., the minimum or maximum times the target behavior must occur for reinforcement delivery), the group contingency (i.e., interdependent vs. dependent), the number of target behaviors, and the reinforcers (Kelshaw-Levering et al., 2000; Popkin & Skinner, 2003). The randomized components help obscure individual performances, and these group CM interventions have resulted in improvements in target behaviors.
The primary purpose of the current study was to develop and test a group CM intervention to target cocaine abstinence of methadone maintenance patients and to determine if this procedure was feasible and safe when applied to drug-dependent individuals. In addition, the study also was designed to address a concern expressed by community-based treatment providers—whether it would be possible to simultaneously address more than one behavior in a CM program. We elected to use an interdependent group contingency with randomized components because it would allow us to simultaneously address multiple target behaviors and obscure individual performances, thus minimizing negative corollary behaviors.
Method
Participants and Setting
Participants were 22 opiate-dependent adult methadone maintenance patients receiving intensive outpatient treatment at a community-based treatment program. Inclusion criteria were the following: use of cocaine (evidenced by providing cocaine-positive urine at study intake or cocaine use as documented by clinic records in the past 30 days), a diagnosis of cocaine abuse or dependence (determined by the psychoactive substance use disorder section of the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders; American Psychiatric Association, 2000), a stable daily dose of methadone ≥ 60 mg, enrollment in intensive outpatient therapy at the methadone clinic (3-hr session, three times weekly), agreement to be videotaped, and ability to fully participate in the study protocol (e.g., physically able to provide urine specimens, available at the appointed CM group times). Potential participants were referred to the study by clinic staff and screened for inclusion by research assistants. A total of 62 patients were referred to the study; research assistants were able to locate and screen 41 of these patients for eligibility, and 31 met the inclusion criteria. Of the 10 who did not meet criteria, 5 had no cocaine use in the past 30 days, 1 did not receive a diagnosis of cocaine abuse or dependence, 2 had a methadone dose that was too low, 1 was retracted by the clinic staff, and 1 was not able to participate at the scheduled CM group time. In addition, 6 patients were eligible but did not complete enrollment. In all, 25 participants were enrolled into the study. Prior to the intervention, 3 participants became ineligible (1 was discharged from the clinic, 1 transferred out of intensive outpatient therapy, and 1 could no longer attend at the scheduled CM group time), leaving 22 participants who participated in interventions and therefore were included in analyses. During the intervention 4 participants from Group 1 were discontinued from treatment at the clinic, and 1 was incarcerated. We examined the data with these individuals included and excluded from the analyses, and there were no meaningful differences. For the purposes of data analyses and presentation, we have included the data provided by these participants until they discontinued treatment. Participant characteristics are provided in Table 1; there were no significant differences between the two groups on demographic characteristics or drug use.
Table 1.
Participant Characteristics at Intake
| Entire sample | Group 1 | Group 2 | p value | |
| Mean age (range) | 42 (23–59) | 41 (23–54) | 43 (30–59) | .607 |
| Female n (%) | 6 (27.3) | 3 (25) | 3 (30) | 1.00* |
| Education n (%) | .323* | |||
| Less than high school | 5 (22.7) | 4 (33.3) | 1 (10) | |
| High school or greater | 13 (72.2) | 8 (66.7) | 9 (90) | |
| Marital status n (%) | .244** | |||
| Married or cohabiting | 1 (4.5) | 1 (8.3) | 0 (0) | |
| Divorced or separated | 7 (31.8) | 5 (41.7) | 2 (20) | |
| Single | 14 (63.6) | 6 (50) | 8 (80) | |
| Employed n (%) | 1 (4.5) | 1 (8.3) | 0 (0) | 1.00* |
| Income n (%) | .666* | |||
| Less than $10,000 | 13 (59.1) | 8 (66.7) | 5 (50) | |
| $10,000 or greater | 9 (40.9) | 4 (33.3) | 5 (50) | |
| Ethnicity n (%) | .455* | |||
| Hispanic | 1 (4.5) | 0 (0) | 1 (10) | |
| Not Hispanic | 21 (95.5) | 12 (100) | 9 (90) | |
| Race n (%) | .329** | |||
| Black | 12 (54.5) | 6 (50) | 6 (60) | |
| White | 9 (40.9) | 6 (50) | 3 (30) | |
| Other | 1 (4.5) | 0 (0) | 1 (10) | |
| Mean drug use (range) | ||||
| Days of cocaine use in month prior to intake | 16 (2–30) | 16 (2–30) | 15 (3–29) | .809 |
| Years of lifetime cocaine use | 10 (1–28) | 10 (2–22) | 11 (1–28) | .925 |
| Years of lifetime opiate use | 12 (2–31) | 13 (2–31) | 10 (2–18) | .456 |
Fisher's exact test.
Likelihood ratio test.
The treatment program provided daily methadone medication to about 1,000 patients to block the effects of illegal opiate use. Treatment was provided in a group format and was based primarily on psychoeducational and 12-step treatment models. The group CM intervention was implemented in a group room (3.4 m by 5.2 m) used exclusively for research purposes. Two authorized institutional review boards approved all procedures.
Behavioral Definitions and Data Collection
To address the question of whether contingencies could be placed on multiple behaviors simultaneously, we addressed three behaviors in addition to the primary target behavior of cocaine use. These behaviors were selected by a community advisory board consisting of representatives from each methadone treatment program in the city in which the study was conducted and subsequently approved by the clinical staff at the treatment program that hosted the study. They were (a) attendance at intensive outpatient treatment sessions, (b) attendance at the group CM meetings, and (c) adherence to the methadone dosing schedule. The four target behaviors were defined and measured as follows.
Cocaine Abstinence
Participants provided urine specimens under research staff observation three times weekly (Monday, Wednesday, and Friday) throughout the study. All urine samples were temperature and adulterant tested to ensure veracity, then immediately screened for the presence of the cocaine metabolite benzoylecgonine via One Step test strips, which identify samples with benzoylecgonine levels below 300 ng/ml as cocaine negative. Participants were informed immediately of their urinalysis results. If a participant failed to attend the treatment program on the scheduled urine-testing day or refused to provide a sample, the urine was considered to be positive for the purposes of administering contingencies unless the participant was granted a verified excused absence by the clinic or study staff. During baseline, all participants received $5.00 in gift cards for each unadulterated specimen, irrespective of the urinalysis result. Initially we did not plan to provide payment for simply submitting urine samples during CM conditions, believing the contingency on cocaine abstinence would sustain adequate sample provision. We discovered with Group 2, who began their first CM phase prior to Group 1, that this procedure did not result in adequate urine-collection rates. Therefore $2.00 payments were instituted for each unadulterated urine sample, irrespective of urinalysis result, beginning at Session 43 for Group 2 and from initiation of CM for Group 1.
Treatment Attendance
As part of preestablished clinical treatment plans, each patient was scheduled for three group sessions each week. Attendance data for these sessions were collected directly from each participant's assigned counselor on a weekly basis using study-provided forms. These data are reported as percentage of participants attending group sessions. To assess data reliability, attendance was intermittently observed and recorded by research staff during the first 3 months of the intervention. Research staff conducted 33 observations (4% of group sessions), and 30 were in agreement with the counselor reports (91%). The proportion of interobserver agreement observations was lower than desired because counselors limited access to group sessions due to concerns about the privacy of group members who were not research participants.
Group CM Meeting Attendance
After arrival at the CM group meeting, the research assistant recorded the participant as present. Participants who arrived after the group drawing had begun were counted as absent for the purposes of data collection and contingencies. These data are reported as percentage of participants who attended the group CM sessions.
Methadone Dosing Compliance
To assess adherence to methadone dosing schedules, data were collected directly from clinic records. For each participant, research staff recorded dates dosed. These data are reported as percentage of participants who were dosed each day since the last group CM session. Methadone dosing is administered via a computerized system that receives directly entered physician prescriptions and creates dispensing orders for nurses who then electronically record the dosing administration. Records are cross-checked daily against inventory and audited at least annually by the federal Drug Enforcement Agency. This system results in an error rate of less than 0.01%.
Procedure
Two groups were formed from the 22 participants. They were composed from multiple treatment groups so as to minimize any influence from preexisting relationships or events that had occurred in the groups. Reversal designs were used with Group 1 (n = 12), who received conditions in an ABCBC order, and Group 2 (n = 10) who experienced conditions in the counterbalanced ACBCB order, with (A) baseline, (B) cocaine abstinence (CA), and (C) multiple behavior (MB) conditions. Condition changes were implemented based on visual inspection of the group's cocaine use for stability, defined as no apparent upward or downward trend. At least three data points were required per condition.
Baseline
After consenting to the study, participants immediately entered a baseline condition in which they submitted urine specimens for testing but did not attend any CM group meetings. Once a stable cocaine-use baseline was established, participants attended their assigned group for three baseline group meetings. At these three meetings, the group leader reviewed the rules and guidelines for prize bowl drawings, administered preference assessments for prizes, and informed group members about the rules for the next CM condition to be implemented (i.e., CA or MB).
General Group Meeting Procedures
Group meetings were scheduled so that they would occur within 1 hr before or after the participant's intensive outpatient treatment sessions. Each group met three times weekly for 10 to 30 min. Group meetings began within 5 min of the scheduled starting time to reinforce timely group attendance. During both CA and MB conditions, those who arrived after the drawing procedures had begun could not participate that day.
As participants assembled in the group room prior to the start of the CM group meeting, they had the opportunity to interact socially and inspect prize selections, which were locked in a glass-front cabinet. During CM conditions, administration of the contingencies and delivery of reinforcers were the only activities scheduled for CM group meetings.
All procedures for administering the contingencies and the reinforcement schedule were managed through the use of a series of drawings. Before beginning the drawings for the day, the group leader described the specific drawing procedures and provided concrete examples of how participants might improve their chances of earning a prize (e.g., the more people who become clean and stay clean, the more likely that everyone will earn prizes). A CM group session could involve draws from up to seven bowls: One was a name bowl that was constructed as participants arrived at the group meeting and contained wooden tiles, each one bearing the name of a participant present that day. Names were drawn from this bowl to determine which participant would make the next draw. The participant whose name was drawn made a single draw from a bowl. If more draws were required, another name was pulled from the name bowl to determine who would make the next draw. To increase participation, once a name was drawn from the bowl, it was not replaced until all other names were drawn.
Up to five bowls were used to determine whether or not the group would receive reinforcement on that day. These bowls are described in the procedures specific to each condition below.
The last bowl was the prize bowl, which was prepared prior to the group meeting and was used to implement the same intermittent probabilistic schedule of reinforcement used in both CM conditions described below. When reinforcement was earned, draws from the prize bowl determined the magnitude of reinforcement earned and consisted of 500 wooden tiles of the following size and proportions (as specified by Petry et al., 2005): 250 “good job” (indicating no prize), 219 small prizes ($1.00 to $3.00), 30 large prizes ($20.00), and 1 jumbo prize ($80.00). Each time they earned reinforcement, group members made four draws from the prize bowl. When they earned reinforcement across three consecutive meetings, they made five bonus draws at the third meeting (i.e., total of nine prize draws). At the next meeting they returned to four draws, but if they continued to earn reinforcement over three more consecutive meetings, the number of bonus draws escalated by one (i.e., 10 draws at the sixth meeting [four regular and six bonus]; 11 draws at the ninth [four regular and seven bonus], etc.). If they failed to earn reinforcement at a meeting, no prize bowl drawings occurred that day, and the total number of bonus draws earned at the next bonus drawing was reset to five, from which it could again escalate following the same rules.
Participants were required to follow standard drawing procedures used to discourage cheating (e.g., looking for specific tiles, palming desirable tiles to produce again in future draws). Participants were asked to remove outer clothing and demonstrate that their hands were empty prior to making a draw. They looked away from the bowl when drawing and selected only one tile at a time. That tile was placed on the table in front of the group leader and then participants again demonstrated that their hands were empty.
After all drawings from the prize bowl were completed, the group leader and a research assistant distributed prize menus to participants. The prize menu listed possible options within each category of prize (small, large, jumbo): five options for small prizes, three for large prizes, and two for jumbo prizes were offered on each menu. Participants absent from a meeting were not eligible for any prizes won at that meeting unless they had an excused absence with valid documentation. Excused group members were eligible to select prizes at the next meeting.
CA Condition
Cocaine abstinence was the only behavior to which contingencies were applied in the CA condition. For each participant who provided a cocaine-free sample, a wooden tile indicating that reinforcement had been earned was placed in the group's abstinence bowl. For each participant who provided a cocaine-positive sample or failed to provide a sample, a wooden tile indicating that no reinforcement had been earned was placed in the abstinence bowl. In the case of an excused absence, no wooden tile was placed in the abstinence bowl. If the participant failed to provide valid written documentation for the excused absence, a no-reinforcement tile was placed in the abstinence bowl at the next meeting. Abstinence bowls were constructed prior to each group meeting to obscure individual performances. At each group CM meeting, the participant whose name was drawn from the name bowl would randomly select a single tile from the abstinence bowl. This tile determined whether the group had earned draws from the prize bowl for that session.
MB Condition
In the MB condition, contingencies were applied to four behaviors: cocaine abstinence, group treatment attendance, CM group attendance, and medication adherence. Data from the previous week were used for group treatment attendance and medication compliance because clinic data were not immediately available. Similar to the CA condition, tiles indicating reinforcement and no reinforcement were placed in each of the four different behavior bowls based on each individual's performance on that behavior. The abstinence, treatment attendance, and medication compliance bowls were constructed prior to each meeting. The group CM attendance bowl was constructed as the participants arrived for the session. This was the only behavior for which individual performances could not be obscured. At each group CM meeting, a single draw was made from a target behavior bowl that contained four tiles (one for each of the four behaviors) and determined the behavior to which the contingency would be applied for that day. Then a single draw was made from the specified behavior bowl to determine whether or not the group had earned draws from the prize bowl for that session.
Safety Measures
Because negative corollary behaviors such as threatening, scolding, and coercion directed toward poorly performing individuals have been noted during group CM (e.g., Greenwood & Hops, 1981) and because group CM rarely had been conducted with a substance-abusing population, we took three safety precautions to make sure that the procedures were not putting group members at increased risk for aggression or abuse by their fellow group members. First, reinforcement and no-reinforcement tiles did not indicate the name of the participant who contributed that tile so that individual performances were not known to others (McLaughlin, 1981). Second, we monitored threatening or coercive interactions between group members by videotaping the CM meeting starting prior to the arrival of the first participant to each group session and continuing until all participants exited the group room. Also, each week every participant completed a four-item confidential survey that asked if they had experienced any negative or coercive interactions with other members of the group. Videotapes and surveys were monitored as they were collected, and any instances of negative interactions were discussed with participants and reported as adverse events to both of the institutional review boards monitoring the study.
Group Leader Training and Intervention Integrity
The first group leader was a masters-level staff member with extensive experience in implementing CM interventions in drug treatment settings. She was trained through readings, didactic instruction, and review of videotapes of the group sessions to reinforce positive group interactions, to address negative interactions immediately by reminding participants of the group rule that negative comments are not allowed, and to follow up privately with participants who gave or received negative comments. Once she was able to implement procedures with integrity, several bachelors-level staff members were trained in the procedure using didactic instruction, passive observation, coleading, and finally leading groups with feedback from the first group leader. The new leader then assumed the leadership responsibilities independently while the original group leader was present. Finally, the newly trained staff member conducted the group sessions independently. All videotaped group sessions were reviewed for procedural integrity by one of the investigators.
Results
Cocaine Abstinence
Figure 1 presents the percentage of cocaine-free urine samples submitted by participants in Group 1 and Group 2, respectively. To provide the most conservative assessment of drug use, scheduled urine samples that were not submitted by the participant were assumed to be positive; however, we also examined the data by omitting missing samples from the calculation of the numerator and denominator, and the patterns did not change appreciably, suggesting that any shifts that may appear across conditions are not a function of missing data. Although both groups showed modest increases in cocaine abstinence compared to baseline when first exposed to the MB condition, there were no clear reversals between CA and MB conditions and changes were often delayed relative to the onset of conditions.
Figure 1.
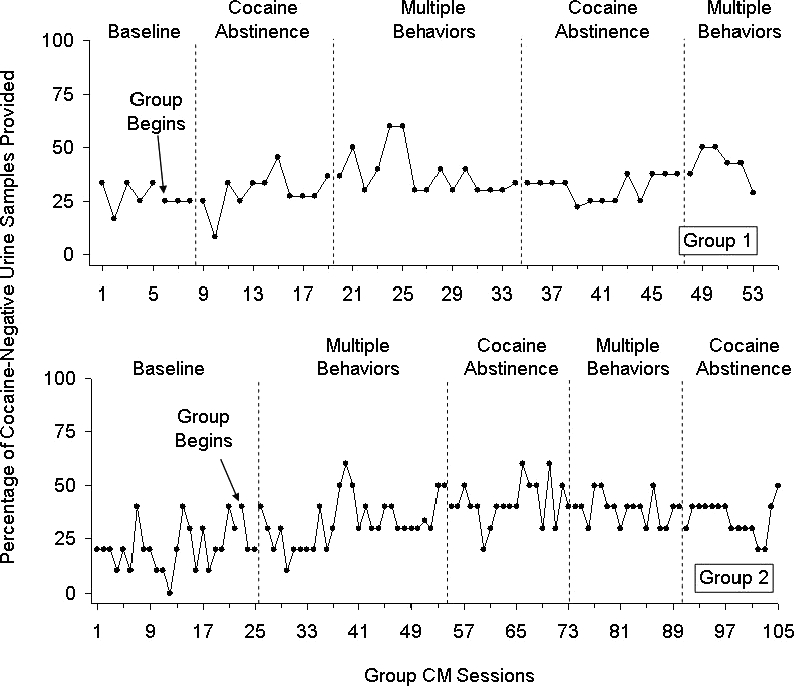
The percentage of participants in Group 1 and Group 2 who submitted cocaine-free urine samples across baseline and CM conditions.
Figure 2 presents the individual cocaine abstinence data for participants in Group 1 and Group 2, respectively. In these graphs each line represents the cocaine urinalysis results of an individual, and results are generally ordered from participants achieving the most cocaine abstinence (heavy black lines) during the study to those achieving the least. Examination of the individual results shows that 11 of 22 participants (50%) showed some increase in cocaine abstinence during the first exposure to a group CM intervention, either by initiating the first instance of cocaine abstinence or by initiating a longer duration of continuous cocaine abstinence (Participants 3, 7, 9, 11, and 12 in Group 1 and Participants 2, 3, 5, 8, 9, 10 in Group 2). Changes in cocaine abstinence do not always occur immediately after introduction of an intervention because among heavy cocaine users, it can take up to several weeks for the cocaine metabolite to clear the urine (Preston, Silverman, Schuster, & Cone, 1997; Vandevenne, Vandenbussche, & Verstraete, 2000). Only 1 participant clearly showed a pattern of increasing drug use after introduction of the group CM contingencies (Participant 8 in Group 1).
Figure 2.
Cocaine urinalysis results across consecutively scheduled urine samples for individual participants in Group 1 (n = 12) and Group 2 (n = 10). Within each panel, each horizontal line represents the cocaine urinalysis results of 1 participant. The heavy portions of each line represent cocaine-negative urinalysis results, the thin portions of each line represent cocaine-positive results, and the blank portions of each line represent missing urine samples. Lines that terminate before reaching the right axis indicate that the participant did not complete the study. Within each panel, participants are arranged from those who showed the least abstinence (fewest cocaine-negative urine samples) on the bottom to those with the most abstinence at the top.
The individual results also show that participants who displayed the least cocaine abstinence during baseline were less likely to increase abstinence during the group CM intervention. Among participants with no evidence of abstinence during baseline (n = 9), only 1 (Participant 5, Group 2) showed increased abstinence during the group CM intervention (11%). All those with limited evidence of abstinence during baseline (i.e., ≤ 25% of baseline urines; n = 5) showed periods of increased abstinence during CM (100%), and all but 2 with moderate to good abstinence (i.e., > 25% of baseline urines; n = 8) showed fairly long durations of abstinence during the group CM conditions (75%). This finding is consistent with results from studies in which CM was delivered independently to individuals, showing that patients who enter treatment cocaine-positive are less likely to respond to CM (Stitzer, Peirce, et al., 2007; Stitzer, Petry, et al., 2007).
Other Behaviors
Group Treatment Attendance
Figure 3 presents the percentage of individuals who attended their group treatment sessions for Groups 1 and 2, respectively. Although Group 1 showed an overall mean increase in group treatment attendance when first exposed to the MB condition and Group 2 had an overall mean decrease when first exposed to the CA condition, there were no clear reversals between conditions. After the initial increase, attendance remained high for Group 1, and after the initial decrease, Group 2's attendance continued to vary widely between 50% and 100%.
Figure 3.
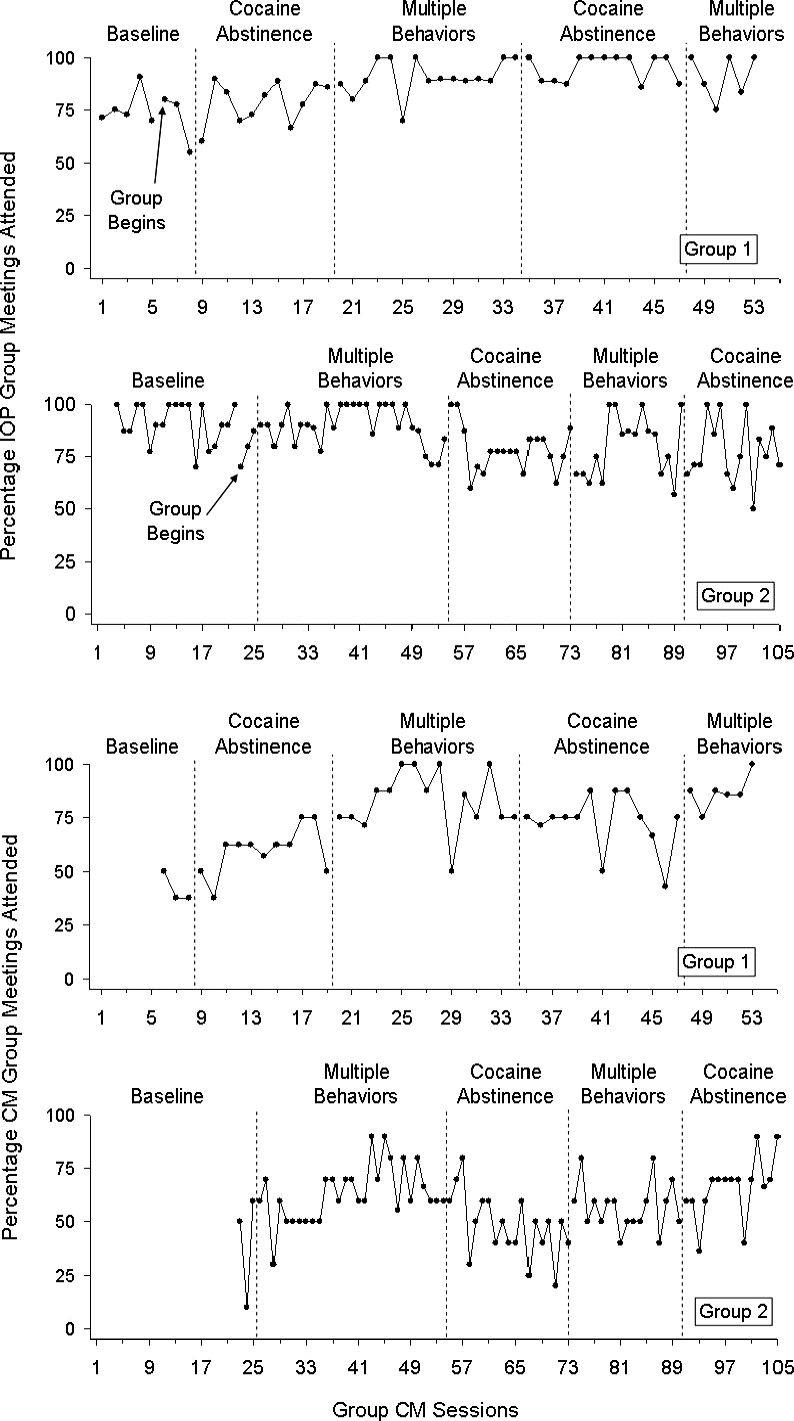
The percentage of participants in Group 1 and Group 2 who attended scheduled intensive outpatient treatment sessions across baseline and CM conditions (top); the percentage of participants in Group 1 and Group 2 who attended group CM meetings during baseline and CM conditions (bottom).
Group CM Attendance
Figure 3 also presents the percentage of individuals who attended the group CM sessions for Groups 1 and 2, respectively. In Group 1, the MB condition produced better overall attendance than the CA condition, and reversals were discernible, although group CM attendance did not fully reverse during the second CA condition to the lower levels seen in the first CA condition. Group 2 showed a similar pattern until the second CA condition, in which the improvements seen in the second MB condition were maintained.
Adherence to Methadone Dosing Schedule
Although methadone adherence was identified as a behavior of concern by our advisory panel and the clinic staff, mean methadone adherence was between 90% and 98% throughout the study for both groups. The means and standard deviations for methadone adherence by group and condition are available from the first author.
Prize Distribution
Table 2 shows the distribution of prizes by group and by CM condition. Overall, participants in Group 1 earned prize draws on a greater proportion of sessions during the MB condition (M = 85%) than during the CA condition (M = 50%). This also was true for Group 2 during the first MB condition (72%), but during the second MB condition (41%), the proportion was similar to that of the two CA conditions (M = 43%). Participants received at least one prize on 96% of the sessions in which prize drawings were earned. The mean value of prizes won did not correspond directly to the proportion of sessions in which draws were earned; however, the mean values tended to be lower when the proportion of sessions receiving prizes was lower. The last two columns of Table 2 show that overall, participants received prizes when their urine tested cocaine negative (Group 1 M = 49%, Group 2 M = 50%) about as often as when it was cocaine positive. In three of the four MB conditions, participants were more likely than not to receive prizes when they were cocaine abstinent, but in all remaining conditions abstinence was followed by a prize on only about one quarter (24%) to one half (52%) of the times it occurred.
Table 2.
Prize Distribution by Group and Phase
| Condition | Number of sessions | Percentage (n) of sessions that |
||
| Earned draws | Received ≥1 prize | Mean prize value per session ($) | ||
| Group 1 | ||||
| CA | 11 | 45 (5) | 45 (5) | 11.45 |
| MB | 15 | 87 (13) | 87 (13) | 12.40 |
| CA | 13 | 54 (7) | 46 (6) | 6.62 |
| MB | 6 | 83 (5) | 83 (5) | 11.00 |
| Group 2 | ||||
| MB | 29 | 72 (21) | 72 (21) | 11.24 |
| CA | 19 | 33 (6) | 33 (6) | 2.44 |
| MB | 17 | 41 (7) | 35 (6) | 1.65 |
| CA | 15 | 53 (8) | 47 (7) | 7.20 |
| Cumulative number of times any participant | Percentage of prizes received while cocaine abstinent (vs. positive) c/a | Percentage of times when abstinent and prize received (vs. not received) c/b | ||
| Received ≥1 prizea | Was cocaine abstinentb | Received ≥1 prize while abstinentc | ||
| 25 | 54 | 13 | 52 | 24 |
| 90 | 48 | 41 | 46 | 85 |
| 35 | 33 | 17 | 49 | 52 |
| 32 | 19 | 16 | 50 | 84 |
| 128 | 84 | 60 | 47 | 71 |
| 27 | 70 | 16 | 59 | 23 |
| 29 | 62 | 18 | 62 | 29 |
| 50 | 47 | 17 | 34 | 36 |
Note. CA = cocaine abstinence; MB = multiple behavior. Superscripted letters indicate the numerator and denominator used to calculate the percentages in the last two columns.
Safety
Only two adverse events involving threatening or coercive interactions occurred during the study and appeared to be related to the group CM procedures. In one case, a participant who had recently drawn a no-prize tile from the prize bowl was approached by 2 group members who attempted to intimidate her, saying that the next time she drew from the bowl, she had better pick a tile that indicated a prize had been earned. Note that the participant in this case was being threatened regarding the result of a random prize bowl draw rather than for behavior under her control (such as remaining abstinent or attending group). The second adverse event occurred when 1 participant told the research assistant that during group meetings, a fellow group member was making negative comments regarding their chances for reinforcement and that he would “knock out” that participant if it happened again. Neither of these events was the result of one group member coercing another to improve the behaviors targeted by the contingencies.
Discussion
The results of the current study suggest that it is feasible to develop and apply interdependent group CM interventions with drug-dependent individuals. The intervention appeared to be acceptable to participants with a study retention rate of 77.3%, which compares favorably with retention rates reported in a multisite CM clinical trial that was conducted in similar community-based methadone treatment programs (64.8% to 67.1% retained; Peirce et al., 2006). Participants appeared to be able to understand the procedures, frequently indicating that they knew in advance which bowl would be drawn from next, and implementing the draws was time efficient (i.e., the entire group CM session lasted 10 to 30 min). This study also suggests that group CM procedures can be safely applied with drug-dependent individuals, with no detected occurrences of physical aggression and only two occurrences of mild threats during the course of the study.
For at least one group (Group 1), the MB condition appeared to produce increases in group CM meeting attendance relative to baseline and the CA condition, suggesting that group CM is potentially efficacious with some behaviors. Unfortunately, it had no discernible effect on cocaine abstinence, group treatment attendance, or medication compliance. Cocaine abstinence data from individual participants were consistent with previous research, suggesting that baseline drug use may influence responding to CM (Stitzer, Peirce, et al., 2007; Stitzer, Petry, et al., 2007).
Examining the correspondence between receiving prizes and cocaine abstinence revealed that prizes generally were received about as often when participants were cocaine abstinent as when they were cocaine positive. As such, it is not surprising that the CM conditions had little influence on cocaine use. By contrast, prizes were never received when a participant was absent from group CM because participants had to attend the group CM meeting to receive a prize. This contingency was in place under all CM conditions, whether or not group CM attendance was reinforced directly. As such, it might be considered surprising that group CM attendance reached its highest points in three of the four MB conditions. This may have occurred because the density of reinforcement was generally higher in MB conditions than in CA conditions. The one exception was the second MB condition in Group 2, which did not result in a higher density of reinforcement and did not produce sessions with the highest attendance.
Although the effects of the group CM contingency were modest and limited to group CM attendance, they are potentially quite important. The majority of methadone treatment patients are injection drug users who are at high risk for HIV infection. Participation in a methadone program is a protective factor against HIV seroconversion, and data suggest that the addition of basic counseling to methadone dosing is associated with better outcomes. This suggests that if group CM were applied in the context of standard group counseling sessions, it could result in increases in the amount of counseling patients receive and produce improved patient outcomes. In this context, even modest increases in attendance could be clinically meaningful if they can produce life-saving outcomes related to HIV seroconversion.
A concern about using a group CM intervention is the risk of positively reinforcing drug use during the group contingency. In other words, an individual in the group who continues to use drugs receives prizes (based on the drug abstinence of another member of the group), and the prizes function to reinforce his or her drug use. Although prizes generally were received about as often when participants were cocaine abstinent as when they were cocaine positive, inspection of individual data suggests that it did not appear that this contingency functioned to reinforce drug use, in that only 1 participant clearly showed an increase in drug use over the course of the study.
Even though the results of this pilot study suggest that the group CM intervention is feasible, they pose more questions than answers. It is not yet clear whether or how the interdependent group CM procedures might be altered to be efficacious in increasing drug abstinence. It is possible that the intervention would be more likely to influence abstinence if the density of reinforcement were increased (e.g., continuous schedule of reinforcement) or with other variations of interdependent group contingencies (e.g., requiring that every member of the group provide at least one drug-free sample per week for all members to receive the incentive). Finally, it remains possible that group CM contingencies will not be successful in initiating abstinence for the majority of group members as long as it is possible for participants to receive reinforcement when they have not exhibited the target behavior.
There are at least three limitations of this study. First, differences in effects between the CA and MB conditions on group CM attendance were modest at best, and the effects of one condition may have carried over to subsequent conditions. Second, the counterbalanced design that was used to examine sequencing effects was probably premature; a simple comparison of group CM to baseline might have provided clearer information at this early stage of intervention development. Third, our initial developmental work studied only one type of dependent group contingency administered on only one schedule of reinforcement. Future studies should examine other dependent contingency arrangements administered using other schedules of reinforcement.
In summary, this study is the first application of an interdependent group CM intervention during drug abuse treatment. Further studies are needed to determine if the efficacy of the intervention can be improved. In addition, future studies will need to compare interdependent group contingencies to no contingencies and to individual contingencies. This would best allow assessment of group CM's relative effectiveness in initiating and sustaining abstinence and determination of whether group CM has any advantages relative to the individual CM procedures that have been proven to be so efficacious.
Acknowledgments
This research was supported in part by a grant from National Institute on Drug Abuse to Kimberly C. Kirby (R01DA019932). We are indebted to Christopher Skinner for his conceptualization of random components in group CM interventions and to Nancy Petry for sharing her experience in managing CM prize exchanges with groups of drug-dependent participants. We are also indebted to the staff and patients at Parkside Recovery in Philadelphia for collaborating with us and participating in our research. The first and second authors contributed equally to this study; a coin flip determined the order of authorship.
References
- Alessi S.M, Hanson T, Wieners M, Petry N.M. Low-cost contingency management in community clinics: Delivering incentives partially in group therapy. Experimental and Clinical Psychopharmacology. 2007;15((3)):293–300. doi: 10.1037/1064-1297.15.3.293. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed., text rev.) Washington, DC: Author; 2000. [Google Scholar]
- Brown N, Redmon W.K. The effects of a group reinforcement contingency on staff use of unscheduled sick time. Journal of Organizational Behavior Management. 1990;10:3–17. [Google Scholar]
- Cashwell C.S, Skinner C.H, Dunn M, Lewis J.C. Group reward programs: A humanistic approach. Journal of Humanistic Education and Development. 1998;37:47–53. [Google Scholar]
- Chambless D.L, Baker M.J, Baucom D.H, Beutler L.E, Calhoun K.S, Crits-Christoph P, et al. Update on empirically validated therapies, II. The Clinical Psychologist. 1998;51((1)):3–16. [Google Scholar]
- Chambless D.L, Ollendick T.H. Empirically supported psychological interventions: Controversies and evidence. Annual Review of Psychology. 2001;52:685–716. doi: 10.1146/annurev.psych.52.1.685. [DOI] [PubMed] [Google Scholar]
- Elk R, Mangus L, Rhoades H, Andres R, Grabowski J. Cessation of cocaine use during pregnancy: Effects of contingency management interventions on maintaining abstinence and complying with prenatal care. Addictive Behaviors. 1998;23:57–64. doi: 10.1016/s0306-4603(97)00020-8. [DOI] [PubMed] [Google Scholar]
- Fals-Stewart W, Birchler G.R. A national survey of the use of couples therapy in substance abuse treatment. Journal of Substance Abuse Treatment. 2001;20((4)):277–283. doi: 10.1016/s0740-5472(01)00165-9. [DOI] [PubMed] [Google Scholar]
- Greenwood C.R, Hops H. Group-oriented contingencies and peer behavior change. New York: Plenum; 1981. [Google Scholar]
- Gresham F.M, Gresham G.N. Interdependent, dependent, and independent group contingencies for controlling disruptive behavior. The Journal of Special Education. 1982;16:101–110. [Google Scholar]
- Griffith J.D, Rowan-Szal G.A, Roark R.R, Simpson D.D. Contingency management in outpatient methadone treatment: A meta-analysis. Drug & Alcohol Dependence. 2000;58:55–66. doi: 10.1016/s0376-8716(99)00068-x. [DOI] [PubMed] [Google Scholar]
- Hayes L.A. The use of group contingencies for behavioral control: A review. Psychological Bulletin. 1976;83:628–648. [PubMed] [Google Scholar]
- Helmus T.C, Saules K.K, Schoener E.P, Roll J.M. Reinforcement of counseling attendance and alcohol abstinence in a community-based dual-diagnosis treatment program: A feasibility study. Psychology of Addictive Behavior. 2003;17:249–251. doi: 10.1037/0893-164X.17.3.249. [DOI] [PubMed] [Google Scholar]
- Higgins S.T, Budney A.J, Bickel W.K, Badger G.J, Florian E, Foerg D.O. Outpatient behavioral treatment for cocaine dependence: One-year outcome. Experimental and Clinical Psychopharmacology. 1995;3:205–212. [Google Scholar]
- Higgins S.T, Budney A.J, Bickel W.K, Foerg F.E, Donham R, Badger G.J. Incentives improve outcome in outpatient behavioral treatment of cocaine dependence. Archives of General Psychiatry. 1994;51:568–576. doi: 10.1001/archpsyc.1994.03950070060011. [DOI] [PubMed] [Google Scholar]
- Higgins S.T, Budney A.J, Bickel W.K, Hughes J.R, Foerg F, Badger G. Achieving cocaine abstinence with a behavioral approach. American Journal of Psychiatry. 1993;150((5)):763–769. doi: 10.1176/ajp.150.5.763. [DOI] [PubMed] [Google Scholar]
- Jones H.E, Haug N, Silverman K, Stitzer M.L, Svikis D. The effectiveness of incentives in enhancing treatment attendance and drug abstinence in methadone-maintained pregnant women. Drug and Alcohol Dependence. 2001;61((3)):297–306. doi: 10.1016/s0376-8716(00)00152-6. [DOI] [PubMed] [Google Scholar]
- Jones H.E, Haug N.A, Stitzer M.L, Svikis D.S. Improving treatment outcomes for pregnant drug-dependent women using low-magnitude voucher incentives. Addictive Behaviors. 2000;25:263–267. doi: 10.1016/s0306-4603(98)00119-1. [DOI] [PubMed] [Google Scholar]
- Kelshaw-Levering K, Sterling-Turner H.E, Henry J.R, Skinner C.H. Randomized interdependent group contingencies: Group reinforcement with a twist. Psychology in the Schools. 2000;37((6)):523–533. [Google Scholar]
- Kirby K.C, Amass L, McLellan A.T. Disseminating contingency-management research to drug abuse treatment practitioners. In: Higgins S.T, Silverman K, editors. Motivating behavior change among illicit-drug abusers: Contemporary research on contingency-management interventions. Washington, DC: American Psychological Association; 1999. pp. 327–344. [Google Scholar]
- Kirby K.C, Benishek L.A, Dugosh K.L, Kerwin M.L.E. Substance abuse treatment providers' beliefs and objections regarding contingency management: Implications for dissemination. Drug and Alcohol Dependence. 2006;85:19–27. doi: 10.1016/j.drugalcdep.2006.03.010. [DOI] [PubMed] [Google Scholar]
- Lew M, Mesch D, Johnson D.W, Johnson R. Positive interdependence, academic, and collaborative-skills group contingencies, and isolated students. American Educational Research Journal. 1986;23((3)):476–488. [Google Scholar]
- Liebson I, Cohen M, Faillace L.A. Group fines: Technique for behavioral control in a token economy. Psychological Reports. 1972;30:895–900. [Google Scholar]
- Litow L, Pumroy D.K. A brief review of classroom group-oriented contingencies. Journal of Applied Behavior Analysis. 1975;8:341–347. doi: 10.1901/jaba.1975.8-341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lloyd J.W, Eberhardt M.J, Drake G.P. Group versus individual reinforcement contingencies within the context of group study conditions. Journal of Applied Behavior Analysis. 1996;29:189–200. doi: 10.1901/jaba.1996.29-189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mawhinney T.C, Fellows-Kubert C. Positive contingencies versus quotas: Tele-marketers exert counter control. Journal of Organizational Behavior Management. 1999;91:35–55. [Google Scholar]
- McCaul M.E, Stitzer M.L, Bigelow B.E, Liebson I. Contingency management interventions: Effects on treatment outcome during methadone detoxification. Journal of Applied Behavior Analysis. 1984;17:35–43. doi: 10.1901/jaba.1984.17-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin T.F. The effects of individual and group contingencies on reading performance of special education students. Contemporary Educational Psychology. 1981;6:76–79. [Google Scholar]
- McLellan A.T. Moving toward a third generation of contingency management studies in the drug abuse treatment field. Experimental and Clinical Psychopharmacology. 2001;9((1)):167–171. doi: 10.1037/1064-1297.9.1.29. [DOI] [PubMed] [Google Scholar]
- McReynolds W.T, Gange J.J, Speltz M.L. Effects of multiple individual and group operant contingencies on student performance. Education and Treatment of Children. 1981;4((3)):227–241. [Google Scholar]
- Milby J.B, Schumacher J.E, Raczynski J.M, Caldwell E, Engle M, Michael M, et al. Sufficient conditions for effective treatment of substance abusing homeless persons. Drug and Alcohol Dependence. 1996;43:39–47. doi: 10.1016/s0376-8716(96)01286-0. [DOI] [PubMed] [Google Scholar]
- Milby J.B, Schumacher J.E, Wallace D, Frison S, McNamara C, Usdan S, et al. Day treatment with contingency management for cocaine abuse in homeless persons: 12-month follow-up. Journal of Consulting and Clinical Psychology. 2003;71((3)):619–621. doi: 10.1037/0022-006x.71.3.619. [DOI] [PubMed] [Google Scholar]
- Pedalino E, Gamboa V.U. Behavior modification and absenteeism: Intervention in one industrial setting. Journal of Applied Psychology. 1974;59:694–698. [Google Scholar]
- Petry N.M, Martin B. Low-cost contingency management for treating cocaine- and opioid-abusing methadone patients. Journal of Consulting and Clinical Psychology. 2002;70((2)):398–405. doi: 10.1037//0022-006x.70.2.398. [DOI] [PubMed] [Google Scholar]
- Petry N.M, Martin B, Finocche C. Contingency management in group treatment: A demonstration project in an HIV drop-in center. Journal of Substance Abuse Treatment. 2001;21((2)):89–96. doi: 10.1016/s0740-5472(01)00184-2. [DOI] [PubMed] [Google Scholar]
- Petry N.M, Martin B, Simcic F., Jr Prize reinforcement contingency management for cocaine dependence: Integration with group therapy in a methadone clinic. Journal of Consulting and Clinical Psychology. 2005;73((2)):354–359. doi: 10.1037/0022-006X.73.2.354. [DOI] [PubMed] [Google Scholar]
- Popkin J, Skinner C.H. Enhancing academic performance in a classroom serving students with serious emotional disturbance: Interdependent group contingencies with randomly selected components. School Psychology Review. 2003;32((2)):282–295. [Google Scholar]
- Preston K.L, Silverman K, Schuster C.R, Cone E.J. Assessment of cocaine use with quantitative urinalysis and estimation of new uses. Addiction. 1997;92((6)):717–727. [PubMed] [Google Scholar]
- Shaner A, Roberts L.J, Eckman T.A, Tucker D.E, Tsuang J.W, Wilkins J.N, et al. Monetary reinforcement of abstinence from cocaine among mentally ill patients with cocaine dependence. Psychiatric Services. 1997;48:807–810. doi: 10.1176/ps.48.6.807. [DOI] [PubMed] [Google Scholar]
- Shapiro E.S, Goldberg R. In vivo rating of treatment acceptability by children: Group size effects in group contingencies to improve spelling performance. Journal of School Psychology. 1990;28:233–250. [Google Scholar]
- Silverman K, Higgins S.T, Brooner R.K, Montoya I.D, Cone E.J, Schuster C.R, et al. Sustained cocaine abstinence in methadone maintenance patients through voucher-based reinforcement therapy. Archives of General Psychiatry. 1996;53((5)):409–415. doi: 10.1001/archpsyc.1996.01830050045007. [DOI] [PubMed] [Google Scholar]
- Silverman K, Wong C.J, Needham M, Diemer K.N, Knealing T, Crone-Todd D, et al. A randomized trial of employment-based reinforcement of cocaine abstinence in injection drug users. Journal of Applied Behavior Analysis. 2007;40:387–410. doi: 10.1901/jaba.2007.40-387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Speltz M.L, Shimamura J.W, McReynolds W.T. Procedural variations in group contingencies: Effects on children's academic and social behaviors. Journal of Applied Behavior Analysis. 1982;15:533–544. doi: 10.1901/jaba.1982.15-533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stitzer M.L, Bigelow G.E, Liebson I. Reducing benzodiazepine self-administration with contingent reinforcement. Addictive Behaviors. 1979;4((3)):245–252. doi: 10.1016/0306-4603(79)90034-0. [DOI] [PubMed] [Google Scholar]
- Stitzer M.L, Bigelow G.E, Liebson I. Reducing drug use among methadone maintenance clients: Contingent reinforcement for morphine-free urines. Addictive Behaviors. 1980;5((4)):333–340. doi: 10.1016/0306-4603(80)90007-6. [DOI] [PubMed] [Google Scholar]
- Stitzer M.L, Bigelow G.E, Liebson I.A, Hawthorne J.W. Contingent reinforcement for benzodiazepine-free urines: Evaluation of a drug abuse treatment intervention. Journal of Applied Behavior Analysis. 1982;15:493–503. doi: 10.1901/jaba.1982.15-493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stitzer M.L, Peirce J, Petry N.M, Kirby K, Roll J, Krasnansky J, et al. Abstinence-based incentives in methadone maintenance: Interaction with intake stimulant test results. Experimental and Clinical Psychopharmacology. 2007;15((4)):344–350. doi: 10.1037/1064-1297.15.4.344. [DOI] [PubMed] [Google Scholar]
- Stitzer M.L, Petry N, Peirce J, Kirby K, Killeen T, Roll J, et al. Effectiveness of abstinence-based incentives: Interaction with intake stimulant test results. Journal of Consulting and Clinical Psychology. 2007;75((5)):805–811. doi: 10.1037/0022-006X.75.5.805. [DOI] [PubMed] [Google Scholar]
- Svikis D.S, Lee J.H, Haug N.A, Stitzer M.L. Attendance incentives for outpatient treatment: Effects in methadone- and nonmethadone-maintained pregnant drug dependent women. Drug and Alcohol Dependence. 1997;48:33–41. doi: 10.1016/s0376-8716(97)00101-4. [DOI] [PubMed] [Google Scholar]
- Theodore L.A, Bray M.A, Kehle T.J, Jenson W.R. Randomization of group contingencies and reinforcers to reduce classroom disruptive behavior. Journal of School Psychology. 2001;39((3)):267–277. [Google Scholar]
- Tingstrom D.H, Sterling-Turner H.E, Wilczynski S.M. The good behavior game: 1969–2002. Behavior Modification. 2006;30((2)):225–253. doi: 10.1177/0145445503261165. [DOI] [PubMed] [Google Scholar]
- Turco T.L, Elliott S.N. Acceptability and effectiveness of group contingencies for improving spelling achievement. Journal of School Psychology. 1990;28:27–37. [Google Scholar]
- Vandevenne M, Vandenbussche H, Verstraete A. Detection time of drugs of abuse in urine. Acta Clinica Belgica. 2000;55((6)):232–333. doi: 10.1080/17843286.2000.11754319. [DOI] [PubMed] [Google Scholar]
- Williamson D.A, Williamson S.H, Watkins P.C, Hughes H.H. Increasing cooperation among children using dependent group-oriented reinforcement contingencies. Behavior Modification. 1992;16((3)):414–425. [Google Scholar]



