Abstract
Background
Residential therapeutic communities (TCs) have demonstrated effectiveness, yet for the most part they adhere to a drug-free ideology that is incompatible with the use of methadone. This study used equivalency testing to explore the consequences of admitting opioid-dependent clients currently on methadone maintenance treatment (MMT) into a TC. Methods: The study compared 24-month outcomes between 125 MMT patients and 106 opioid-dependent drug free clients with similar psychiatric history, criminal justice pressure and expected length of stay who were all enrolled in a TC. Statistical equivalence was expected between groups on retention in the TC and illicit opioid use. Secondary hypotheses posited statistical equivalence in the use of stimulants, benzodiazepines, and alcohol, as well as in HIV risk behaviors.
Results
Mean number of days in treatment was statistically equivalent for the two groups (166.5 for the MMT group and 180.2 for the comparison group). At each assessment, the proportion of the MMT group testing positive for illicit opioids was indistinguishable from the proportion in the comparison group. The equivalence found for illicit opioid use was also found for stimulant and alcohol use. The groups were statistically equivalent for benzodiazepine use at all assessments except at 24 months where 7% of the MMT group and none in the comparison group tested positive. Regarding injection- and sex-risk behaviors the groups were equivalent at all observation points.
Conclusions
Methadone patients fared as well as other opioid users in TC treatment. These findings provide additional evidence that TCs can be successfully modified to accommodate MMT patients.
Keywords: therapeutic community, opioid dependence, methadone, residential treatment
1. Introduction
Research has demonstrated that therapeutic communities (TCs) have beneficial effects in decreasing drug use (Simpson and Curry, 1997), and decreasing sexual HIV risk behaviors (Cooperman et al., 2005). An extensive literature on TC treatments for opioid dependence has found that retention in a treatment program is the main marker of a variety of successful outcomes (Carroll and McGinley, 2000; De Leon and Schwartz, 1984; McCaul et al., 2001; Simpson and Curry, 1997). In general the longer a resident remains in treatment, the more likely positive outcomes will occur. Several studies have indentified factors that predict longer retention, including less severe psychiatric illness (Condelli and De Leon, 1993; Eland-Goossensen et al., 1998), involvement with and pressure from the criminal justice system (Eland-Goossensen et al., 1998; Harrison et al., 2007; Sacks et al., 2004), and client expectations about a longer length of treatment (Condelli and De Leon, 1993; Kressel et al., 2000).
In the last decade TCs have modified their approaches to accommodate a variety of special populations, including prisoners (Sacks et al., 2004), women and their children, adolescents (De Leon, 1997), people with HIV/AIDS (Sargent et al., 1999), homeless persons (De Leon et al., 2000; Skinner, 2005) and those with co-occurring mental illness requiring psychiatric medication (Sacks et al., 1997). A small number of TCs have also made modifications to allow clients on methadone maintenance treatment (MMT) into the TC. The primary application of TC methods to MMT patients was led by George De Leon (De Leon et al., 1995). The “Passages” project was a day treatment program based on TC methods that were adapted for patients in methadone clinics. The most comprehensive evaluation of Passages indicated that its clients improved significantly more than comparison subjects on measures of cocaine and heroin use, and those who remained in Passages for at least six months exhibited further positive outcomes.
The use of medically prescribed drugs for substance abuse has been inconsistent with the TC perspective, however (De Leon, 2000). In the TC view, medications that alter emotional or mental states could reinforce the substance abuse and impede recovery. For example, TC staff may view methadone as a threat to the individual and the system as a whole. MMT clients tend to be marginalized and perceived as using a crutch to progress through the treatment process (Greenberg et al., 2007). These beliefs may undermine treatment success among methadone patients, and influence treatment policies. Due to philosophical differences between TCs and methadone programs, TCs often do not admit to treatment patients who are receiving methadone, and very few actually provide MMT services. For example, the National Survey of Substance Abuse Treatment Services (Office of Applied Studies, 2007) found that for residential treatment settings (including halfway houses and TCs) only 3.6% had opioid treatment programs. Similarly, a recent national survey of 380 TCs indicated that less than 10% use methadone (Institute for Behavioral Research, 2005).
Yet methadone is one of the most widely used and extensively evaluated treatments for opioid dependence. Research indicates that opioid-dependent clients treated with methadone tend to fare better than those who are not treated with methadone (Gossop et al., 2000, National Institutes of Health-Center for Disease Control, 1997; Farrell et al., 1994). In addition, the National Consensus Panel on Effective Medical Treatment of Opioid Addiction (1998) calls attention to the need for opioid dependent persons to have access to MMT and recommends expanding the availability of MMT.
The current study explored the effectiveness of admitting opioid-dependent clients currently on MMT into TC treatment. If more TCs are to treat MMT patients, it is vital to document whether MMT patients do as well as opioid users who are not enrolled in MMT, which TCs are accustomed to treating. To examine this question we used equivalence testing (Rogers et al., 1993) to contrast a group of MMT patients to a comparison group of similar non-MMT opioid users. Equivalence testing is a statistical technique often used to show that a new medication is indistinguishable from an approved medication that is the standard of care. In this study, TC treatment for drug-free opioid users represents the usual mode of care. The aim of the study was to learn whether MMT patients would benefit as well from enrollment in a TC. In the context of a TC setting we tested whether outcomes for MMT patients would be indistinguishable from those of opioid dependent patients not enrolled in MMT. Specifically, using a comparison group of opioid-dependent clients with similar psychiatric history, criminal justice pressure and expected length of stay in the TC, we tested the hypotheses that: (1) Retention in the TC would be statistically equivalent between patients receiving or not receiving MMT, and (2) use of illegal opioids would be statistically equivalent in the MMT and comparison groups at assessments up to 24 months from baseline. Secondary hypotheses posited statistical equivalence between the two groups in the use of stimulants, benzodiazepines, and alcohol, as well as in HIV risk behaviors and criminal behaviors. Although medical issues, employment, family issues, alcohol use, and many other factors are also important outcomes, primary hypotheses focused on retention and illegal use of opioids to preserve experiment-wise power.
2. Method
2.1. Study Design
We used a two-group longitudinal follow-up design to compare outcomes for TC residents admitted while receiving MMT (n=125) to those of TC residents who were not receiving MMT upon admission (n=106). Participants were not randomized to conditions, but the groups were balanced on variables shown to predict TC retention in prior studies: criminal justice pressure, history of psychiatric hospitalization or suicidal attempt, and expected length of stay. Participants were followed for 24 months after admission to the TC. The primary outcomes included retention in the TC and opioid use.
2.2. Setting and Research Participants
Participants were opioid users admitted to the residential TC treatment program of Walden House, Inc. in San Francisco, CA. They were recruited at admission to the TC from three Walden House adult programs that provided variable planned length of residential treatment, ranging from 45 days to 12 months. All programs provided continuity of treatment, and when residents completed one program they were often transferred to the next level of care in the Walden House system. Thus, while these three sites were the points of initial treatment for research participants, TC treatment was also provided at other sites during the study, for example as participants completed residential treatment and transferred to group living “satellites”, and later to independent living as “outpatients.” TC clients were allowed to continue in MMT while enrolled in the treatment program.
The program has a long history of embracing patients with diverse and challenging needs and has been providing residential treatment options for persons on methadone for over two decades. The TC has made a number of modifications to accommodate the presence of residents receiving methadone (see Greenberg et al., 2007). For example, the program designates a “methadone counselor,” a TC staff member who plays a vital role in the process of facilitating the residential treatment program in modifying its services to accept and treat MMT patients. The methadone counselor offers “methadone sensitivity” training sessions to staff periodically (such as during TC staff training days) and to patients (providing education and confronting stigma about methadone maintenance). The methadone counselor conducts a weekly “methadone therapy group” for residents who are receiving methadone. For patients who choose to attempt withdrawal from methadone, residents have greater access to alternative therapies and medical services. Staff education programs in the TC setting have the potential to increase acceptance of non-abstinence treatment goals and use of pharmacotherapies such as methadone. For example, Andrews et al. (2005) found that TC staff that participated in methadone sensitivity training had greater methadone knowledge and a lower abstinence orientation than those who had not attended the training.
In this study the participants in the MMT group were all patients in San Francisco area methadone maintenance treatment programs at the time they applied for admission to the TC. During residential stay in the TC the patients were escorted to the relevant MMT program to receive treatment, and if they received take-home doses those were stored in a secure medication dispensary at the TC. During the course of the study the San Francisco Department of Public Health began a mobile methadone van program. A common problem for mobile methadone programs has been finding a site that is acceptable to the community (see Besteman and Brady, 1994). As part of the commencement of the van program, the mobile clinic was located for part of the day in the staff parking lot of the Walden House Outpatient program (a few miles from the TC residential programs), and in return for use of the parking lot and a counseling office, the TC residents on methadone were able to transfer to the van program. Once the methadone van was established the participants in treatment had the option of receiving methadone treatment there, and most chose that option.
2.3. Inclusion and Exclusion Criteria
Participants were included in the study if they were residents at Walden House TC treatment centers who qualified for MMT (current use plus confirmation of at least one-year documented history of opioid dependence), admitted to the TC no more than three working days before the research screening interview, willing to allow access to agency records, and willing to participate in follow-up interviews. In addition, participants in the MMT group either had to be enrolled in long-term 180-day methadone detoxification or MMT. Participants were excluded from the study if they were unable to provide informed consent or not qualified for MMT, or if the study was unable to complete a research baseline interview within seven days of their admission to the TC.
2.4. Enrollment Procedures
2.4.1. Recruitment
Screening procedures were adapted from methods developed for a prior study of day treatment conducted at Walden House (Guydish et al., 1998). The project director (SA) trained clinical staff in the program’s intake department to identify participants meeting study criteria, and research staff determined eligibility. The University of California, San Francisco Committee on Human Research approved all procedures, and a Federal Certificate of Confidentiality was obtained to provide an extra level of protection against disclosure.
2.4.2. Balancing the Groups on Factors that Predict Retention
Balancing procedures were designed to assure that the MMT and comparison group participants did not substantially differ on three factors demonstrated to predict retention in TCs: Criminal justice pressure, history of psychiatric hospitalization or suicidal attempt, and expected length of stay. All three variables were dichotomous. Although each factor is conceptually a continuum, it was measured as a “yes-no” dichotomy to allow the TC intake staff to screen new admissions for possible research involvement more easily. Criminal justice pressure was defined as presence of justice system involvement on the client intake form (including court diversion, incarcerated pending trial, on parole, pending sentence, or on probation). Psychiatric hospitalization was screened in a similar fashion; this factor differentiated participants who had ever been hospitalized for psychiatric problems or had made a suicide attempt in their lifetime from those who had not. Expected length of stay was based on the number of days the TC staff expected a participant to remain in the program. The staff estimate was based on knowledge of the client goals and pressures for admission or discharge, as well as the treatment program to which the resident was being admitted. Pilot data suggested that a cutoff score of 180 days distinguished participants who remained in the program for longer versus shorter stays. The project director kept updated information on these factors in the MMT group. As participants accrued, if a disparity of greater than 10% existed between MMT and comparison group on any balancing criterion, the next candidate for the comparison group was not recruited unless the candidate met the under-represented factor.
2.5. Measures
Research interviews were conducted at baseline and at 6, 12, 18, and 24 months. As a primary measure of substance use, a urine sample was collected at each research interview. Quest Diagnostics, a licensed laboratory in California, conducted urine toxicology screens for amphetamines, barbiturates, benzodiazepines, cannabinoids, cocaine, ethanol, methadone, methaqualone, opioids, phencyclidine, and propoxyphene using enzyme immunoassay.
Self-report measures included the Addiction Severity Index (ASI; McLellan et al., 1992) and the Texas Christian University AIDS Risk Assessment (TCU/ARA; Camacho et al., 1997). Three measures were calculated from the TCU/ARA. Four items for the injection-related risk measure addressed self-reported injection frequency; times used “dirty” needles or syringes (used by others but not sterilized or cleaned with bleach); times shared cooker, cotton or rinse water; and times injected with people who were also injecting. Three items for the sex-related risk measure addressed times having sex without a latex condom with someone who was not a spouse or primary partner, sex while “high” on drugs or alcohol, and vaginal sex. A Concern with AIDS measure was calculated with three items that addressed a belief that one could become exposed to the AIDS virus, a belief that one “really could get AIDS,” and a desire to “make some changes now” to reduce AIDS risks.
We used the TC’s main client database to determine retention in the TC. These numbers were checked against retention logs the research staff updated throughout the study. The research staff calculated retention as the number of days a client remained continuously in treatment from admission to discharge, including residential and satellite care. Because some clients dropped out of treatment and then returned, we regarded treatment as continuous until a client remained out of treatment for 14 days, a criterion that we had used when we previously studied this setting (Guydish et al., 1998). Retention in MMT was based on self-reported methadone use in the past 30 days from the ASI.
2.6. Statistical Methods
As the two groups in this study were not randomized but balanced in three key measures, baseline values were compared using standard two-group tests for proportions and means. Statistical equivalence was examined using a two one-sided confidence interval approach (Bristol, 1999). Under this method the two treatment groups are declared as equivalent if the confidence interval for the difference between the groups is completely within the range defined as plus and minus 20% of the value of the comparison group. This is a standard limit in equivalence testing (Stegner et al., 1996). For the outcomes measured on a binary scale (e.g., urine test results) we tested the proportions drug-positive in each treatment group. Continuously distributed measures were compared using the difference in the group means. Finally, for the survival function for days to end of treatment (reflecting retention in the TC), the equivalence test of Wellek (1993) was used. This tests the full survival function for equivalence as opposed to just the mean number of days in treatment.
Statistical analysis consisted of two stages. In the first stage a test of equivalence was conducted. When statistical equivalence was not established, a traditional test of group differences was conducted in the second stage. Rogers et al. (1993) point out that an equivalency test and a traditional hypothesis test are not mutually exclusive. It is possible to obtain seemingly contradictory findings when an equivalency test suggests that two groups differ, yet a traditional hypothesis test fails to find a statistical difference. In these instances, “the effect is not reliable enough to conclude either a sizable difference or a reliable small difference” (p. 562). In these cases, there is insufficient evidence to arrive at a decision regarding equivalency.
When no statistical equivalence was found, the proportions or means were compared for statistical difference using standard Pearson chi-square test of proportions and t-tests for means.
All tests were considered statistically significant at p < .05. We allocated the Type I error rate as follows: comparisons at baseline were at .05, comparisons at the 6-month assessment (i.e., during treatment) at .05, and the three post-treatment assessments at a total of .05 using a correction based on Bonferroni’s inequality (Hays, 1981). The injection-risk and sex-risk subscale scores from the TCU/ARA had a large percentage of participants scoring at zero (i.e., no risk) at each assessment, thus these two measures were dichotomized into risk vs. no risk.
3. Results
3.1. Preliminary Analyses
Missing data
A total of 231 participants provided baseline data (125 MMT group, 106 comparison group). At the 6-month assessment, 221 (96%) were assessed (95% of MMT group, 96% of comparison group). The follow-up rates for the 12-, 18-, and 24-month assessments were similar: 94%, 90% and 87% for the MMT group and 92%, 91% and 82% for the comparison group. All participants had completed TC treatment by the end of Month 12. Analyses were conducted on all observed data at each assessment. The baseline measures for those who were not assessed past baseline were compared to those who were available for assessment at 12, 18, and 24 months. No significant differences were found on any of the baseline measures, suggesting that participants who completed follow-up assessments did not differ from participants who did not complete follow-up assessments.
Sample demographics at baseline
Demographic characteristics are summarized in Table 1. The only difference that emerged between groups was in living arrangements: Participants in the MMT group were more likely to describe themselves as homeless, while in the last 30 days participants in the comparison group were more likely to have been in an institution.
Table 1.
Background characteristics of participants by treatment condition
| Variable | MMT
(n=125) |
Comparison
(n=106) |
P Level |
|---|---|---|---|
| Age in years | 40.2 +/− 10.11 | 39.4 +/− 9.48 | n.s |
| Men (%) | 64 | 61 | |
| Ethnicity (%) | n.s. | ||
| African-American/Black | 28 | 35 | |
| Asian/Pacific Islander | 0 | 1 | |
| Hispanic | 9 | 7 | |
| Caucasian | 54 | 44 | |
| Other | 7 | 9 | |
| Multiple | 2 | 4 | |
| Education (%) | n.s. | ||
| Some high school | 36 | 25 | |
| Completed high school/GED | 64 | 75 | |
| Marital status (%) | n.s. | ||
| Married | 9 | 16 | |
| Divorced | 41 | 35 | |
| Never married | 51 | 49 | |
| Sexual Orientation (%) | n.s. | ||
| Homosexual/gay/lesbian | 1 | 3 | |
| Heterosexual | 91 | 91 | |
| Bisexual | 8 | 7 | |
| Occupation (%) | n.s. | ||
| Professional/technical | 5 | 9 | |
| Managerial/Administrative | 2 | 1 | |
| Sales | 7 | 5 | |
| Clerical/office | 10 | 15 | |
| Craft [skilled trade] | 14 | 17 | |
| Operative [not transportation] | 6 | 2 | |
| Transportation operative | 5 | 5 | |
| Laborer [unskilled] | 17 | 16 | |
| Private household worker | 2 | 1 | |
| Service Worker | 23 | 22 | |
| Military | 1 | 0 | |
| Never employed | 7 | 9 | |
| Annual Income | n.s. | ||
| LT $10,000 | 68 | 72 | |
| Living Situation | .029 | ||
| House/apartment [rent/own] | 9 | 8 | |
| House/apartment [another’s] ½ way house/therapeutic comm. | 24 | 23 | |
| Room/hotel/motel | 14 | 9 | |
| Homeless | 29 | 18 | |
| Institution (jail, hospital) | 14 | 32 | |
| Other | 1 | 0 | |
| History of Psychiatric Hospitalization or Suicide Attempt | 29% | 32% | n.s. |
| Expected to remain in TC >180 days | 46% | 45% | n.s. |
| Criminal Justice Pressure | 56% | 68% | n.s. |
Continuous variables are expressed as mean +/− standard deviation.
All percentages rounded to nearest whole number.
Balancing factors
As shown in Table 1, the MMT group did not differ statistically from the comparison group on psychiatric history, expected stay in the TC beyond 180 days, or criminal justice pressure.
Baseline Measures
The study groups were equivalent on toxicology screens for illicit opioids (11%, MMT versus 9%, comparison), cocaine (4%, MMT versus 3%, comparison), stimulants (4%, MMT versus 3%, comparison) benzodiazepines (6%, MMT versus 5%, comparison); no urine toxicology screens tested positive for alcohol. Insufficient evidence exists to make a decision regarding statistical equivalence for Concern for AIDS measure on the TCU/ARA, and mean self-reported days of heroin use. For these outcomes, the test of statistical equivalence failed to reject the hypothesis of nonequivalence, yet a traditional test of group differences also failed to reach statistical significance.
Methadone Treatment
Participants in the MMT group were more likely to report receiving methadone on the ASI than the comparison group at baseline (95% vs. 12%) and at 6-month (81% vs. 11%), 12-month (77% vs. 18%), 18-month (72% vs. 19%), and 24-month (70% vs. 30%) follow-ups. This pattern of findings is relatively consistent with participants’ study group and suggests that participants in the MMT group tended to adhere to a methadone-dispensing regimen while comparison group participants did not use methadone. The linear increase from baseline over follow-ups to 24 months in the use of methadone among comparison group participants is statistically significant (Cochran-Armitage Z= -3.42, p < .001).
3.2. Hypothesis Testing
Hypothesis 1, Retention in the TC
The mean number of days in treatment was 166.5 for the MMT group and 180.2 for the comparison group; the median was 109.0 and 159.5 days, respectively. A plot of the survival curves with confidence interval bounds is shown in Figure 1.
Fig. 1.
Survival curves show days of retention in treatment are equivalent for both groups
The two survival functions are statistically equivalent (X2W = 0.23, p < .0001), which supports the first hypothesis.
The mean days in treatment (instead of the entire survival curve) were also compared for equivalence using the standard confidence interval approach. The two groups were equivalent on this measure as well. At the 12-month assessment 193 (84%) of participants were no longer enrolled in any Walden House treatment program, and the remaining participants were enrolled in a WH treatment program, specifically 8 (3%) were enrolled in outpatient treatment, 12 (5%) were enrolled in residential treatment, and 18 (8%) were enrolled in a satellite treatment program.
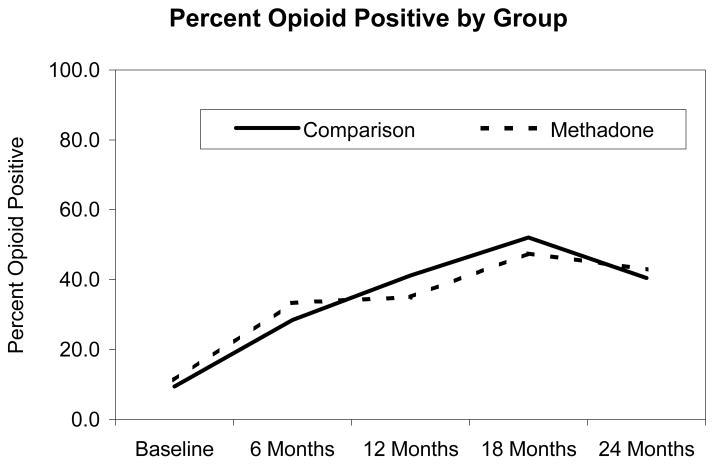
Hypothesis 2, Opioid use
As shown in Figure 2, for each of the assessments, the proportion of the MMT group testing positive for illicit opioids was statistically equivalent to the proportion in the comparison group.
Fig. 2.
Illicit opioid use increases over time for both groups
3.3 Supplementary Analyses
Other drug use
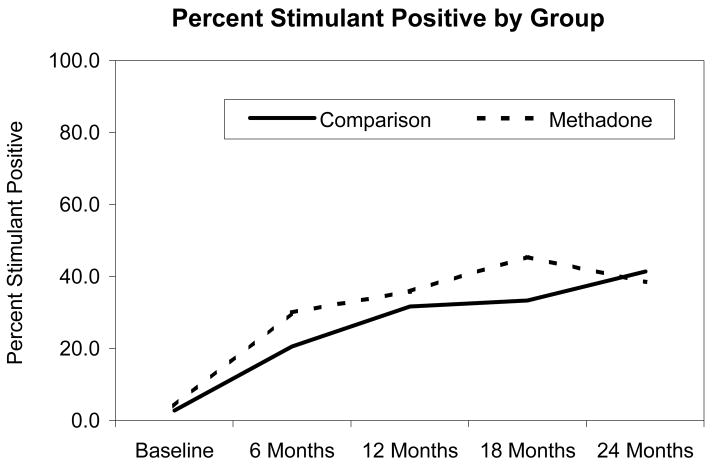
As shown in Figure 3, statistical equivalence was also found for stimulant use (defined as testing positive for either cocaine or amphetamines).
Fig. 3.
Stimulant use increases over time for both groups
Tests of equivalence were also conducted for the presence of benzodiazepines and alcohol even though the observed proportions testing positive were close to zero. The groups were statistically equivalent for benzodiazepine at all assessments except at 24 months where 7% of the MMT group and none in the comparison group tested positive (p < .05). No participant tested positive for alcohol at intake, and the groups were equivalent at all other assessments.
HIV risk behaviors
Between group comparisons on the dichotomized TCU/ARA injection-risk measure and sex-risk measure were equivalent across time. At baseline, about 46% in both groups engaged in risky injection behavior. The rate of risky injection behavior decreased to approximately 24% at 6 months and was sustained at 24 months. About 37% of the participants in both groups engaged in risk sex behavior across the 24 months of the study.
The Concern for AIDS measure was not equivalent at the 18-month assessment only, with the MMT group having a lower scale score, but because traditional tests of group differences were not statistically significant, there is insufficient evidence to make a statistical decision on the 18-month assessment.
4. Discussion
In this study, equivalence testing was used to determine whether MMT patients were indistinguishable from patients who were not receiving MMT at a TC. TCs are not accustomed to treating opioid-dependent patients on MMT. TCs traditionally emphasize abstinence rather than maintenance on opioids, and even medically prescribed methadone is viewed as a mood-altering drug that reinforces substance dependence and impedes recovery. Many staff may view MMT as a threat to the environment of the TC. Despite these potential obstacles to treatment, however, our findings suggest that the MMT clients fare as well as non-MMT clients.
MMT clients did not differ from non-MMT clients on key outcome variables, including retention in the TC, illicit opioid use, alcohol use, stimulant use, benzodiazapine use (with the exception of the 24-month follow-up), and injection- and sex-risk behaviors at all follow-up assessments. These findings suggest that the TC was modified to the point that MMT clients can be integrated successfully into an environment that is usually opposed toward patients taking methadone.
The 24-month longitudinal study design allowed for the examination of long-term treatment effects. Multiple assessments up to 24 months after admission, with excellent follow-up rates, provide a longer-term view than most previous studies of TC residents. Of the published studies that have examined TC treatment outcomes, for example, only three have followed patients up to 24 months (Condelli and De Leon, 1993; Wexler et al., 1999; De Leon et al., 2000).
A substantial proportion of participants in both groups did not return to illicit opioid use, and of the clients in MMT, many continued to use methadone. Across the follow-up periods, however, the proportion of participants who used illicit opioids increased steadily. At 18 months, a large proportion of clients were no longer enrolled in the TC yet a subgroup used illicit opioids. This subgroup of illicit-opioid using participants may have benefited from better availability of extended treatment or aftercare services. For example, it may be useful to identify the point at which clients had returned to illicit opioid use, reassess motivation for treatment and actively link them to treatment, such as in the Recovery Management Checkup intervention developed by Scott and Dennis (Scott et al., 2005).
It is noteworthy that more than two-thirds of the MMT patients were receiving MMT at each follow-up point. Since methadone use is viewed as inconsistent with TC philosophy and may possibly be seen as a threat by some treatment staff, MMT patents may have felt pressure to discontinue MMT, yet a substantial proportion of MMT participants reported using methadone during the 24 months after enrollment in the study. Additionally, from study admission to the 24-month follow-up interview a significant increase appeared in the proportion of comparison group participants receiving methadone. These findings suggest that many clients in the comparison group also perceived advantages to being on MMT.
Our MMT treatment rates are in the upper range of methadone retention rates reported in recent studies; 1-year retention rates ranged from 25% to more than 70% (Rowan-Szal et al., 2000; Neufeld et al., 2008; Deck and Carlson, 2005). The relatively high MMT participation rates and new entrants into methadone treatment observed in this study suggest an acceptance of and commitment to MMT among clients receiving services in a TC setting. We caution, however, that the data are point prevalence enrollment self-reported by study participants and do not always reflect continuous retention in a single MMT program.
Regarding secondary hypotheses, stimulants (cocaine and methamphetamine) were the most frequently used illicit drugs after illicit opioids, and the MMT and non-MMT groups showed equivalent use. Other drugs and alcohol were used less frequently.
The results of this study should be considered in light of design limitations. Participants were not randomly assigned to treatment conditions. Thus, participants self-selected to receive MMT, which may reflect a higher perceived need for MMT, commitment to MMT, knowledge of methadone treatment services, and acceptance of methadone treatment as an important part of their recovery. The finding that the majority of MMT patients were in MMT treatment at follow-up interviews up to 24 months provides further evidence of their commitment to this treatment modality. This strong commitment to MMT may have protected these clients from antithetical views toward MMT by some TC clients or staff. MMT clients without this strong commitment may not have fared as well in other TC settings. In addition, the TC environment of the treatment program examined in this study may not extend to other TC programs. The TC had years of experience with incorporating methadone patients into the milieu, and the program made modifications to allow TC residents to receive MMT (see Greenberg et al., 2007), thus findings from this study may not extend to TCs that have policies excluding or discouraging methadone maintenance treatment. In addition, our study did not gather information on short-term interruptions of TC treatment (under 14 days), which could overstate the TC retention rates and make the results less generalizable. Research shows that shorter dropout between initial dropout and first readmission is a predictor of longer retention when clients return to the TC later ( De Leon and Schwartz, 1984). Similarly, the findings for non-MMT group may not generalize to TCs that do not allow MMT. Allowing MMT patients may have impacted non-MMT residents in unknown ways. For example, the linear increase in methadone use by the comparison group may reflect positive perceptions of MMT that they acquired during their stay in the TC. Thus, additional studies are needed to assess the impact of integration of MMT services in the TC setting, specifically the impact on patients and staff.
Although the study has limitations, results suggest that methadone patients can benefit from TC treatment and respond as well as a comparison group matched on psychiatric history, criminal justice pressure and expected length of stay. Because traditional TCs have had unfavorable views about methadone treatment and a belief that the use of methadone treatment by those in the TC would pose a threat to the entire community, it was reasonable to raise the question of whether TC residents receiving MMT would have equivalent treatment outcomes to those not receiving methadone treatment in a modified TC setting. While the TC had prior experience in treating patients on methadone, the present study created a unique opportunity to increase the population of patients on methadone maintenance therapy during the course of the study. In preparation for the influx of methadone patients, the TC developed specific strategies to educate both staff and clients about methadone treatment and to address the unique treatment needs of methadone patients (Greenberg et al., 2007).
There remain significant barriers to overcome before a large number of programs will treat MMT patients in the TC setting. In addition to challenges about treatment philosophy, values, and attitudes toward methadone there is also additional cost. In this case the TC collaborated with the community’s mobile methadone program, allowing residents already on MMT to continue receiving methadone without cost to them in trade for providing parking and office space at the Walden House outpatient program. Similar opportunities may not be available in other communities. We also point out that evidence of equivalent effectiveness has not been the driving force in shaping the substance abuse treatment network. Thus, there are both scientific and practical limitations to this work, and considerably more research, policy change, and positive treatment experiences will be needed for system change to occur.
The results of the present study provide evidence that the implementation of these staff, patient, and therapeutic adaptations allowed methadone patients to be successfully integrated into the TC setting. These findings are consistent with those of De Leon et al. (1995) demonstrating that suitably modified TCs can be employed successfully with methadone maintenance patients. Perfas and Spross (2007) contend that the traditional drug-free orientation of TCs has been changing rapidly in response to the need to treat co-occurring disorders, and a key issue is to accept current health care realities without compromising the unique qualities of the TC approach. That said, persuading TCs to change their philosophy is only one step in incorporating MMT into the TC setting. Organizational change must also be addressed. For example, TC programs may not have the medical staff and resources to store methadone, and it may be difficult to identify MMT programs willing to work as partners with a TC to provide methadone. Despite these barriers, the results of the present study suggest that TC treatment programs may want to consider expanding their reach to accommodate patients receiving opioid replacement therapy such as methadone.
Acknowledgments
The authors express gratitude to the staff and patients of Walden House, Inc. and the Opiate Treatment Outpatient Program (Division of Substance Abuse and Addiction Medicine, San Francisco General Hospital). We are grateful for the participation of the late Alfonso Acampora, Debby Caruso, TeChieh Chen, Jongserl Chun, Chuck Deutschmen, Don Frazier, Ali Hall, Nancy Haug, Jennifer Hettema, Rod Libbey, Steve Myers, Larry Nelson, Bayley Raiz, and Yong Song, in carrying out the study and Kevin Ahern for data management.
Grant Support
This project was supported by NIH Research Grants, primarily R01DA014922, as well as P50DA09253 (San Francisco Treatment Research Center), U10DA15815 (CA-AZ Clinical Trials Network Node), and K01DA00408 for Dr. Masson.
Footnotes
Author Responsibilities
James L. Sorensen
Conceptualized the study, led the research team through the project, and drafted the manuscript, and reviewed the final manuscript prior to submission.
Siara Andrews
Supervised the collection of data, implemented follow-up methods, and reviewed the final manuscript prior to submission.
Kevin L. Delucchi
Designed and supervised the conduct of data analyses, participated in writing or revision of the manuscript, and reviewed the final manuscript prior to submission.
Brian Greenberg
Led the clinical team that provided the therapeutic community intervention, participated in writing or revision of the manuscript, and reviewed the final manuscript prior to submission.
Joseph Guydish
Provided ongoing advice and technical guidance in scientific conduct of the investigation, participated in writing or revision of the manuscript, and reviewed the final manuscript prior to submission.
Carmen L. Masson
Provided ongoing advice and technical guidance in collection of service-related data, participated in writing and revision of the manuscript and reviewed the final manuscript prior to submission.
Michael Shopshire
Assisted in interpretation of study findings, co-wrote and revised many sections of the manuscript, and reviewed the final manuscript prior to submission.
Conflict of interest
No conflict declared.
References
- Andrews S, Sorensen JL, Guydish J, Delucchi K, Greenberg B. Knowledge and attitudes about methadone maintenance among staff working in a therapeutic community. J Maintenance in the Addictions. 2005;3(1):47–59. doi: 10.1300/J126v03n01_05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Besteman KJ, Brady JV. Implementing mobile drug abuse treatment: The implementation of innovative approaches. In: Fletcher BW, Inciardi JA, Horton AM, editors. Drug abuse treatment: The implementation of innovative approaches. Westport, CT: Greenwood; 1994. pp. 33–42. [Google Scholar]
- Bristol DR. Clinical equivalence. J Biopharm Stat. 1999;9:549–561. doi: 10.1081/bip-100101195. [DOI] [PubMed] [Google Scholar]
- Camacho LM, Bartholomew NG, Joe GW, Simpson DD. Maintenance of HIV risk reduction among injection opioid users: a 12 month posttreatment follow-up. Drug Alcohol Depend. 1997;47:11–18. doi: 10.1016/s0376-8716(97)00056-2. [DOI] [PubMed] [Google Scholar]
- Carroll JF, McGinley JJ. An agency follow-up outcome study of graduates from four inner-city therapeutic community programs. J Subst Abuse Treat. 2000;18:103–118. doi: 10.1016/s0740-5472(99)00036-7. [DOI] [PubMed] [Google Scholar]
- Condelli WS, De Leon G. Fixed and dynamic predictors of client retention in therapeutic communities. J Subst Abuse Treat. 1993;10:11–16. doi: 10.1016/0740-5472(93)90093-h. [DOI] [PubMed] [Google Scholar]
- Cooperman NA, Falkin GP, Cleland C. Changes in women’s sexual risk behaviors after therapeutic community treatment. AIDS Educ Prev. 2005;17:157–169. doi: 10.1521/aeap.17.3.157.62901. [DOI] [PubMed] [Google Scholar]
- Deck D, Carlson MJ. Retention in publicly funded methadone maintenance treatment in two western states. J Behav Health Serv Res. 2005;32:43–60. doi: 10.1007/BF02287327. [DOI] [PubMed] [Google Scholar]
- De Leon G, editor. Community as method: Therapeutic communities for special populations and special settings. Westport, CT: Praeger; 1997. [Google Scholar]
- De Leon G. The therapeutic community. New York: Springer; 2000. [Google Scholar]
- De Leon G, Stains GL, Perlis TE, Sacks S, McKendrick K, Hilton R, Brady R. Therapeutic community methods in methadone maintenance (Passages): an open clinical trial. Drug Alcohol Depend. 1995;37:45–57. doi: 10.1016/0376-8716(94)01057-r. [DOI] [PubMed] [Google Scholar]
- De Leon G, Sacks S, Staines G, McKendrick K. Modified therapeutic community for homeless mentally ill chemical abusers: Treatment outcomes. Am J Drug Alcohol Abuse. 2000;26:461–480. doi: 10.1081/ada-100100256. [DOI] [PubMed] [Google Scholar]
- De Leon G, Schwartz S. Therapeutic communities: What are the retention rates? Am J Drug Alcohol Abuse. 1984;10:267–284. doi: 10.3109/00952998409002785. [DOI] [PubMed] [Google Scholar]
- Eland-Goossensen AM, van de Goor IAM, Benschop AJ, Garretsen HFL. Profiles of heroine addicts in different treatment conditions and in the community. J of Psychoactive Drugs. 1998;3:11–20. doi: 10.1080/02791072.1998.10399666. [DOI] [PubMed] [Google Scholar]
- Farrell M, Ward J, Mattick R, Hall W, Stimson GV, DesJarlais D, Gossop M, Strang J. Fortnightly review: Methadone maintenance treatment in opiate dependence: A review. British Medical Journal. 1994;309:997–1001. doi: 10.1136/bmj.309.6960.997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gossop M, Marsden J, Stewart D, Rolfe A. Patterns of improvement after methadone treatment: 1 year follow-up results from the national treatment outcome research study. Drug Alcohol Depend. 2000;60:275–286. doi: 10.1016/s0376-8716(00)00109-5. [DOI] [PubMed] [Google Scholar]
- Greenberg B, Hall DH, Sorensen JL. Methadone maintenance therapy in residential therapeutic community settings: Challenges and promise. J Psychoactive Drugs. 2007;39:203–210. doi: 10.1080/02791072.2007.10400606. [DOI] [PubMed] [Google Scholar]
- Guydish J, Werdegar D, Sorensen JL, Clark W, Acampora A. Drug abuse day treatment: A randomized clinical trial comparing day and residential treatment programs. J Consult Clin Psychol. 1998;66:280–289. doi: 10.1037//0022-006x.66.2.280. [DOI] [PubMed] [Google Scholar]
- Hays WL. Statistics. 3. New York: Holt, Rinehart and Winston; 1981. [Google Scholar]
- Harrison SR, Toriello P, Pavluck A, Ellis R, Pedersen E, Gaiennie R, Kissinger P. The impact of a brief induction on short-term continuation in a therapeutic community. Am J Drug Alcohol Abuse. 2007;33:147–153. doi: 10.1080/00952990601091135. [DOI] [PubMed] [Google Scholar]
- Institute for Behavioral Research. National Treatment Center Study, Summary report No. 9: A National Sample of Therapeutic Communities. Athens, GA: Institute for Behavioral Research, University of Georgia; 2005. [Google Scholar]
- Kressel D, De Leon G, Palij M, Rubin G. Measuring client clinical progress in therapeutic community treatment the therapeutic community Client Assessment Inventory, Client Assessment Summary, and Staff Assessment Summary. J Subst Abuse Treat. 2000;19:267–272. doi: 10.1016/s0740-5472(00)00108-2. [DOI] [PubMed] [Google Scholar]
- McCaul ME, Svikis DS, Moore RD. Predictors of outpatient treatment retention: patient versus substance use characteristics. Drug Alcohol Depend. 2001;62:9–17. doi: 10.1016/s0376-8716(00)00155-1. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, Pettinatti H, Argerion M. The fifth edition of the Addiction Severity Index. J Subst Abuse Treat. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- National Institutes on Health-Centers for Disease Control. NIH consensus statement. Bethesda, MD: National Institutes of Health; 1997. Effective medical treatment of heroin addiction. [Google Scholar]
- National Consensus Panel on Effective Medical Treatment of Opioid Addiction. JAMA. 1998;280:1936–1943. [PubMed] [Google Scholar]
- Neufeld K, King V, Peirce J, Kolodner K, Brooner R, Kidorf A comparison of 1-year substance abuse treatment outcomes in community syringe exchange participants versus other referrals. Drug Alcohol Depend. 2008;97:122–129. doi: 10.1016/j.drugalcdep.2008.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of Applied Studies. DASIS Series: S-39. (SMA) 07-4296. Rockville, MD: Department of Health and Human Services, Substance Abuse and Mental Health Services Administration; 2007. National Survey of Substance Abuse Treatment Services (N-SSATS): 2006. Data on substance abuse treatment facilities. [Google Scholar]
- Perfas FB, Spross S. Why the concept-based therapeutic community can no longer be called drug-free. J Psychoactive Drugs. 2007;39:69–79. doi: 10.1080/02791072.2007.10399866. [DOI] [PubMed] [Google Scholar]
- Rogers JL, Howard KI, Vessey JT. Using significance tests to evaluate equivalence between two experimental groups. Psychol Bull. 1993;113:553–565. doi: 10.1037/0033-2909.113.3.553. [DOI] [PubMed] [Google Scholar]
- Rowan-Szal GA, Chatham LR, Simpson DD. Importance of identifying cocaine and alcohol dependent methadone clients. Am J Drug Alcohol Abuse. 2000;9:38–50. doi: 10.1080/10550490050172218. [DOI] [PubMed] [Google Scholar]
- Sacks S, Sacks J, De Leon G, Bernhardt A, Staines G. Modified therapeutic community for mentally ill chemical abusers: Background; influences; program description; preliminary findings. Subst Use Misuse. 1997;32:1217–1259. doi: 10.3109/10826089709035472. [DOI] [PubMed] [Google Scholar]
- Sacks S, Sacks JY, McKendrick K, Banks S, Stommel J. Modified TC for MICA offenders: Crime outcomes. Behav Sci Law. 2004;22:477–501. doi: 10.1002/bsl.599. [DOI] [PubMed] [Google Scholar]
- Sargent R, Sorensen JL, Greenberg B, Evans G, Acampora AP. Residential detoxification for substance abusers with HIV/AIDS: Walden House detoxification program. J Subst Abuse Treat. 1999;16:87–95. doi: 10.1016/s0740-5472(98)00013-0. [DOI] [PubMed] [Google Scholar]
- Scott CK, Dennis ML, Foss MA. Utilizing recovery management checkups to shorten the cycle of relapse, treatment entry, and recovery. Drug Alcohol Depend. 2005;78:325–338. doi: 10.1016/j.drugalcdep.2004.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson DD, Curry SJ. Drug abuse treatment outcome study (DATOS) Psychol Addict Behav. 1997;11:211–337. [Google Scholar]
- Skinner DC. A modified therapeutic community for homeless persons with co-occurring disorders of substance abuse and mental illness in a shelter: An outcome study. Subst Use Misuse. 2005;40:483–497. doi: 10.1081/ja-200052429. [DOI] [PubMed] [Google Scholar]
- Stegner BL, Bostrom AG, Greenfield TK. Equivalence testing for use in psychosocial and services research: An introduction with examples. Evaluation and Program Planning. 1996;19:193–198. [Google Scholar]
- Wellek S. A log-rank test for equivalence of two survivor functions. Biometrics. 1993;49:877–881. [PubMed] [Google Scholar]
- Wexler HK, De Leon G, Thomas G, Kressel D, Peters J. The Amity Prison TC evaluation : Reincarceration outcomes. Crim Justice Behav. 1999;26:147–167. [Google Scholar]