Abstract
We report here, for perhaps the 1st time in the English-language literature, the extent of the territory fed by the anterior bifurcation of the (anomalous) split right coronary artery (RCA). A 64-year-old man presented with an occlusion of the anterior bifurcation of a split RCA—which resulted in an infarct that involved both the inferoseptal left ventricular wall and the anterior right ventricular free wall. Split RCA is the same anomaly as the improperly named “double right coronary artery.” In reality, there are not 2 RCAs, but only split portions of the posterior descending branch of the RCA, with 2 separate proximal courses.
Key words: Coronary vessel anomalies/diagnosis, myocardial infarction/diagnosis/physiopathology
In December 2007, a 64-year-old hypertensive man, a chronic smoker with dyslipidemia, presented at the hospital 6 hours after the onset of chest pain. In the emergency room, an electrocardiogram (ECG) showed a pre-existing right bundle branch block with new Q waves in the inferior leads and ST-segment elevation in the anterior precordial leads (Fig. 1). Cardiac enzymes were elevated (creatine kinase, 702 U/L; creatine kinase MB, 91.1%; cardiac troponin T, 0.344 ng/mL). An echocardiogram on admission showed basal inferior and mid-inferior akinesia with anterior right ventricular wall hypokinesia. The anterior left ventricular wall contracted normally.
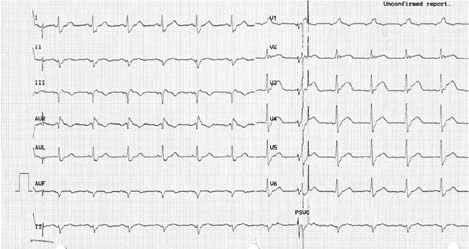
Fig. 1 Electrocardiogram on admission.
Due to the presumptive diagnosis of acute anterior myocardial infarction, the patient was immediately studied by means of coronary angiography, which showed a normal left coronary artery (Fig. 2), a split right coronary artery (RCA) with proximal occlusion of the anterior bifurcation, and no distal filling through collateral vessels (Fig. 3). The posterior subdivision of the RCA led to a small upper posterior descending branch and a large posterolateral branch (Fig. 3). The occluded anterior subdivision was entered and dilated; a 2.75 × 14-mm Endeavor® stent (Medtronic, Inc.; Minneapolis, Minn) was deployed, which resulted in recovery of TIMI-3 flow while antegrade filling of the posterior descending branch showed on angiography (Fig. 4). Follow-up ECGs showed gradual resolution of the ST-T changes (Fig. 5).
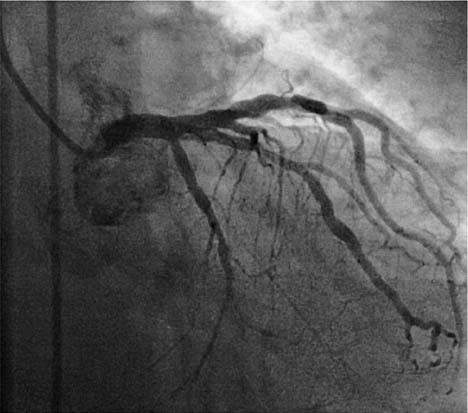
Fig. 2 Angiogram on admission shows near-normal left coronary artery.
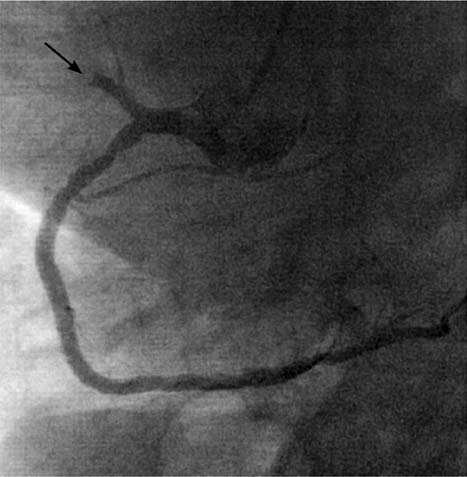
Fig. 3 Angiogram on admission shows total occlusion (arrow) of the split anterior bifurcation of the right coronary artery.
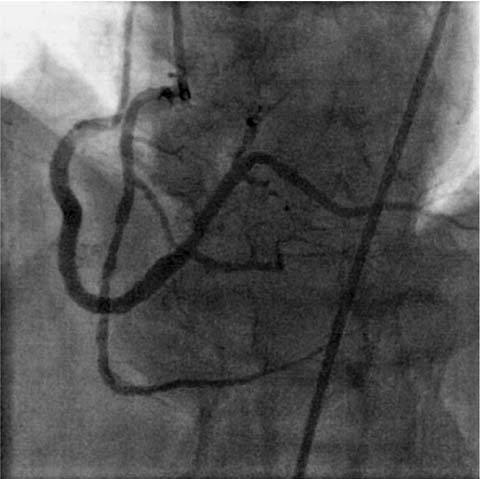
Fig. 4 Immediately after angioplasty, antegrade filling of the more distal posterior descending branch appears upon angiography.
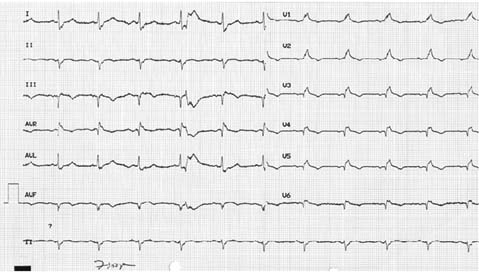
Fig. 5 Two days after angioplasty, an electrocardiogram shows that ST-T changes are beginning to resolve.
Discussion
The ECG continues to be a useful clinical tool during an acute myocardial infarction, in order to locate the infarct region, to evaluate the extent of the damage, and to elaborate upon markers of prognostic value. Generally, it is stated that an anterior myocardial infarction is manifested by ST-segment elevation in the anterior precordial leads. In addition, elevation in leads V1 through V3 would indicate proximal occlusion of the left anterior descending coronary artery,1 especially when this elevation is associated with ST-segment depression in inferior leads.2 On the other hand, inferior myocardial infarction—when associated with ST-segment elevation in lead III greater than in lead II and with ST-segment depression in leads I and aVL—would indicate occlusion of the RCA.3,4 Additional ST-segment elevation in leads V3R and V4R would favor proximal occlusion of the RCA,3 invariably involving branches of the free wall of the right ventricle. Occasionally, an isolated proximal occlusion of the RCA with right ventricular infarction can mimic an anterior myocardial infarction.5
In our patient, the left coronary system was normal and the acute marginal and conus branches were part of the anterior bifurcation of the RCA, while the right precordial leads did not show ST-segment elevation. Therefore, ST-segment elevation of the anterior “left” ventricular leads must have been related to the occlusion of the right ventricular branches.
We conclude that this case shows, as we report here for perhaps the 1st time in the English-language medical literature, the extent of the territory fed by the anterior bifurcation of the split RCA: the infarct involved both the inferior and anterior right ventricular free walls.
Coronary anomalies were recently and extensively reviewed in Angelini's textbook dedicated to that subject.6 Split RCA was reported as the most common (1.23% of 1,950 cases) type of coronary anomaly in a large catheterization-laboratory population, which was studied prospectively with clearly established diagnostic criteria.6 Split RCA was defined as an RCA that featured a split posterior descending branch, with the anterior subdivision of the RCA leading to the distal portion of the posterior descending branch (which serves the posterior septum and the inferior wall of the left ventricle), but also leading to the anterior free wall of the right ventricle. The other (posterior) bifurcation of the RCA maintains a course in the atrioventricular groove and forms the uppermost portion of the posterior descending branch. The length of each of the 2 posterior descending branches varies from patient to patient: in our patient, the anterior subdivision of the RCA was apparently the larger one, and its occlusion resulted in the aforementioned infarct both of the anterior free wall of the right ventricle and of the inferior wall of the left ventricle.
Split RCA is the same anomaly, anatomically, as the improperly named “double right coronary artery.”7,8 In reality, there are not 2 RCAs, but only split portions of the posterior descending branch of the RCA, with 2 separate proximal courses.
Footnotes
Address for reprints: Fadi J. Sawaya, MD, La Vista Walk, Apt. 1243, 2300 La Vista Road, Atlanta, GA 30324. E-mail: fad_sawaya@hotmail.com
References
- 1.Engelen DJ, Gorgels AP, Cheriex EC, Ophuis AJ, Dassen WR, et al. Value of the electrocardiogram in localizing the occlusion site in the left anterior descending coronary artery in acute anterior myocardial infarction. J Am Coll Cardiol 1999; 34(2):389–95. [DOI] [PubMed]
- 2.Tamura A, Kataoka H, Mikuriya Y, Nasu M. Inferior ST segment depression as a useful marker for identifying proximal left anterior descending artery occlusion during acute anterior myocardial infarction. Eur Heart J 1995;16(12):1795–9. [DOI] [PubMed]
- 3.Lopez-Sendon J, Coma-Canella I, Alcasena S, Seoane J, Gamallo C. Electrocardiographic findings in acute right ventricular infarction: sensitivity and specificity of electrocardiographic alterations in right precordial leads V4R, V3R, V1, V2, and V3. J Am Coll Cardiol 1985;6(6):1273–9. [DOI] [PubMed]
- 4.Zimetbaum PJ, Josephson ME. Use of the electrocardiogram in acute myocardial infarction. N Engl J Med 2003;348(10): 933–40. [DOI] [PubMed]
- 5.Halkett JA, Commerford PJ, Millar RS. Right ventricular infarction mimicking extensive anterior infarction. Chest 1986; 90(4):617–9. [DOI] [PubMed]
- 6.Angelini P, Villason S, Chan AV Jr, Diez JG. Normal and anomalous coronary arteries in humans. In: Angelini P, editor. Coronary artery anomalies: a comprehensive approach. Baltimore: Lippincott Williams & Wilkins; 1999. p. 27–79.
- 7.Gulel O, Yazici M, Durna K, Demircan S. A rare coronary anomaly: double right coronary artery. Clin Cardiol 2007;30 (6):309. [DOI] [PMC free article] [PubMed]
- 8.Erbagci H, Davutoglu V, Turkmen S, Kizilkan N, Gumusburun E. Double right coronary artery: review of literature. Int J Cardiovasc Imaging 2006;22(1):9–11. [DOI] [PubMed]


