Abstract
Background
There is limited knowledge of the development of IgE-antibody levels over time in childhood, with respect to persistency and co-sensitization to specific inhalant allergens.
Methods
Data from 2033 children participating in the BAMSE birth cohort was used. Background factors and clinical parameters were obtained and IgE antibody (ab) levels to eight common airborne allergens were measured (≥0.35 kUA/L) when the children were 4 and 8 years of age.
Results
Between 4 and 8 years the proportion of children sensitized to any of the inhalant allergens tested increased from 15% to 25%. At 4 years IgE-ab to birch and cat dominated, whereas at the age of 8, there was a considerable increase in the proportion of sensitization to timothy and dog. Except for mites and moulds, IgE-ab levels to all aeroallergens increased significantly between 4 and 8 years among those already sensitized at 4. Transient sensitization to inhalant allergen was uncommon. Furthermore, sensitization to birch pollen at 4 years increased the risk for becoming sensitized to timothy, cat and dog later in life. Such an association was not observed among those sensitized primarily to animal dander.
Conclusions
There is a prominent process of sensitization at pre-school age to inhalant allergens, and in Northern Europe sensitization to birch pollen early in life seems to be important for this process. Such a process has a probable impact on the development of allergic disease in the growing child.
Cite this as: A. Asarnoj, E. Östblom, I. Kull, G. Lilja, G. Pershagen, G. Hedlin, M. van Hage and M. Wickman, Clinical and Experimental Allergy, 2008 (38) 1507–1513.
Keywords: allergy, BAMSE, childhood, IgE, sensitization
Introduction
At least one-fourth of all Swedish children are affected by symptoms related to allergic disease such as asthma, eczema, allergic rhinitis and food hypersensitivity [1]. Allergic sensitization, i.e. IgE-antibodies (ab) to common food and inhalant allergens, is closely related to symptoms and further development of allergic diseases [2–6]. Sensitization to aeroallergens is often preceded by sensitization to food allergens. However, the development of IgE-ab to aeroallergens may appear early in life, in particular among children with asthma [7–10]. Increased IgE-ab levels to food and inhalant allergens, in particular to mites, cat and dog, in young children have been shown to increase the risk of allergic disease later in childhood [6, 11]. Furthermore, the sum of allergen-specific IgE-ab has been demonstrated to be higher among children with symptomatic allergic disease [4]. In a recent paper, elevated concentrations of IgE-ab to grass pollen increased the probability and severity of rhinitis in 5-year-old children [12]. However, data on changes of IgE sensitization among children over time, in terms of the prevalence and levels of allergen-specific IgE-ab are limited. Available studies on this topic have evaluated sensitization in a limited number of children and/or are based on high-risk populations [6, 13].
The aim of this study was to assess changes in the prevalence of IgE-ab and IgE-ab levels to inhalant allergens between 4 and 8 years of age in a large population-based birth cohort (BAMSE).
Materials and methods
Study subjects
The BAMSE study is an unselected population-based birth cohort study of 4089 children (75% of the original target population) born during 1994–1996 in representative, defined areas in Stockholm, Sweden. Study design, enrolment, criteria for inclusion and procedures for data collection have been described elsewhere [14]. Briefly, data on different background factors such as allergic heredity, various exposures and other family circumstances were obtained by parental questionnaires when the children were 2–3 months of age. When the child was 1, 2, 4 and 8 years of age the parents answered detailed questionnaires on symptoms of allergic disease and key exposures. All children with completed questionnaires at 4 and 8 years of age were invited to a clinical testing. Blood was drawn from 70% (n=2614) and 65% (n=2461) of the children at 4 and 8 years of age, respectively. In 2033 children, blood samples were obtained at both 4 and 8 years of age. These children constitute the basis for the analysis presented in this paper. Definitions of symptoms (asthma, rhinitis and eczema) used in the BAMSE cohort have been described elsewhere [15]. Permission for the study was obtained from the Ethics Committee of Karolinska Institutet. The parents of all participating children gave their informed consent.
Measurements of sensitization
The blood samples were screened with Phadiatop® [a mixture of common inhalant allergens: birch, timothy, mugwort, cat, dog, horse, mould (Cladosporium herbarum) and house dust mite (HDM) (Dermatophagoides pteronyssinus)] and fx5® (a mixture of common food allergens: cow's milk, egg white, soy bean, peanut, cod fish and wheat) (ImmunoCAP™, Phadia AB, Uppsala, Sweden). Sera with a positive Phadiatop® or a positive fx5®, defined as IgE-ab levels ≥0.35 kUA/L, were analysed for allergen-specific IgE-ab to the airborne and food allergens listed above. Data on the prevalence of sensitization to food allergens at 4 and 8 years of age will be presented elsewhere (manuscript in preparation). Levels between 0.35 and 100 kUA/L were registered, and an IgE-ab concentration ≥100 kUA/L was in the statistical evaluation given the value of 100 kUA/L. Three percent of the analyses for allergen-specific IgE-abs failed due to a scarce amount of blood.
Statistical analysis
Prevalences are expressed in percent of the total number of observations available. Ninety-five percent confidence intervals (CIs 95%) were calculated and intervals not overlapping were considered to be statistically different. χ2-tests were used for dichotomous variables, e.g. comparisons of prevalence between groups. Allergen-specific IgE-ab concentrations were log normally distributed and subjected to a logarithmic transformation before analysis. T-tests were used for analysis of the continuous IgE-variables. IgE mean levels are presented as geometric mean levels. Multiple logistic regression models were used for calculations of odds ratios (ORs) and CI between specific sensitizing allergen at 4 years in relation to sensitization at 8 years. Adjustments in the multivariate analyses were made for parental allergy and sex, which affected the risk of sensitization to the outcome allergens tested with 10% or more. Because allergic children are more likely to be sensitized to multiple allergens, adjustments were made for each inhalant and food allergen tested at 4 years. P-values ≤0.05 were considered to be statistically significant. All analyses were undertaken with the software STATA® version 9.
Results
Children in the study group (n=2033) did not differ in any major background factor (sex, parental allergy, tobacco smoke exposure, exclusive breastfeeding, cat-ownership) compared with the original study base of 4089 children. Furthermore, no statistically significant differences in the prevalence of asthma, rhinitis, eczema or geometric mean IgE-levels to Phadiatop® and fx5® were observed between these two groups at the age of 4 and 8 (data not shown).
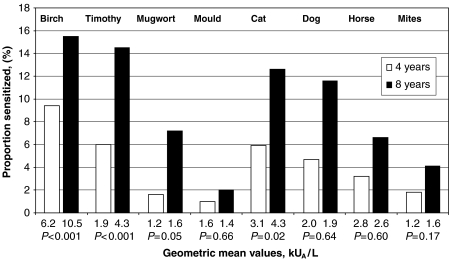
Three-hundred and nine (15%) and 510 (25%) children were sensitized to at least one of the selected inhalant allergens at 4 and 8 years of age, respectively (P<0.001). The prevalence of positive (IgE ≥0.35 kU/L) tests and the IgE-ab concentrations, presented as geometric mean, of the selected inhalant allergens in relation to age are presented in Fig. 1. The prevalence increased with age for all allergens. Both at 4 and at 8 years, birch pollen, followed by pollen of timothy, cat and dog dander were the most common sensitising allergens.
Fig. 1.
Prevalence of sensitization (IgE≥0.35 kUA/L) and geometric mean values in kUA/L to specific airborne allergens at 4 and 8 years of age in 2033 identical children.
Sensitization at 4 years of age to common inhalant allergens was persistent in most children at 8 years of age (Table 1). This was true for 97% of birch-positive children, 86% of timothy-positive, 97% mugwort-positive, 94% of cat-positive, 91% of dog-positive and 94% of horse-positive children at 4 years of age. Among these children all the allergen-specific IgE-levels increased significantly (P<0.001), except those for mould and mites. Among children with remittent sensitization, i.e. sensitization at 4 but not at 8 years, only 38% of the children were mono-sensitized and as many as 20% were sensitized to four inhalant allergens or more. The allergen-specific levels of all 48 children who remitted ranged from 0.35 to 3.92 kUA/L, geometric mean 0.75 kUA/L.
Table 1.
Immunoglobulin E antibody levels (geometric mean) to inhalant allergens among children sensitized at 4 or 8 years only or sensitized both at 4 and 8 years†
| At 4 but not at 8 years in 48 children | Both at 4 and 8 years in 279 children | At 8 but not at 4 years in 426 children | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Allergens | n | % | IgE (kUA/L) g/mean | n | % | IgE at 4‡ (kUA/L) g/mean | IgE at 8§ (kUA/L) g/mean | n | % | IgE (kUA/L) g/mean |
| Birch | 5 | 0.3 | 0.9 | 181 | 8.9 | 6.5* | 21.3* | 119 | 5.9 | 3.4 |
| Timothy | 16 | 0.8 | 0.8 | 101 | 5.0 | 2.2*; | 10.0* | 178 | 8.8 | 2.6 |
| Mugwort | 1 | 0.1 | 0.5 | 31 | 1.5 | 1.2* | 3.3* | 104 | 5.1 | 1.3 |
| Cat | 7 | 0.3 | 0.7 | 111 | 5.5 | 3.3* | 8.1* | 142 | 7.0 | 2.6 |
| Dog | 8 | 0.4 | 0.6 | 85 | 4.2 | 2.2* | 5.0* | 144 | 7.1 | 1.1 |
| Horse | 4 | 0.2 | 0.7 | 58 | 3 | 2.9* | 5.1* | 71 | 3.5 | 1.5 |
| Mites | 11 | 0.5 | 0.9 | 25 | 1.2 | 1.4 NS | 1.9 NS | 56 | 2.8 | 1.4 |
| Mould | 6 | 0.3 | 0.7 | 12 | 0.6 | 2.2 NS | 2.2 NS | 23 | 1.1 | 1.0 |
Internal missing: 0.9–2.2% for each allergen tested.
For all allergens, except mould and mites, the IgE antibody levels increased significantly between 4 and 8 years among those with persistent sensitisation; *P<0.001; NS, not significant.
For all allergens, except mould and mites, the IgE antibody levels were significantly higher among those with persistent sensitization compared with those with late onset sensitization, *P<0.001; NS, not significant.
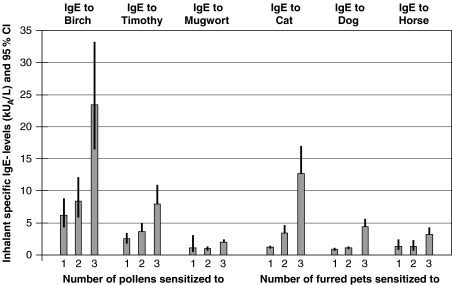
Among 8-year-old children, we analysed the association between specific IgE-ab levels (kUA/L) to the pollens and furred animals and the number of allergens (pollen and/or animal species) that the child was sensitized to (Fig. 2). With increasing number of sensitizing pollens, the IgE-ab levels to each of birch and timothy increased. This pattern was also seen in the furred pet allergens tested for.
Fig. 2.
IgE-antibody levels to inhalant allergens in 8-year-old children sensitized to one to three pollens or one to three furred pets expressed as geometric mean and 95% CI. CI, confidence interval.
We further analysed sensitization to inhalant and food allergens at 4 years of age and the risk for persistent or onset of sensitization to the four most common inhalant allergens (birch, timothy, cat and dog) at 8 years of age. A multiple logistic regression model adjusted for identified confounders such as sex and parental allergy, but also for all allergens tested (Tables 2 and 3) was used. From both tables, it is notable that the OR decreased drastically after adjustment for the other allergens. This was more pronounced for mould, mugwort and horse, but comparably less for birch and fx5®. Obviously, sensitization at 4 years of age represented the highest risk for sensitization to the same allergen at 8 years of age, corresponding to an increased risk of 20 times or more after adjustment for the other allergens. Sensitization to any pollen among the 4-year-olds increased the odds of sensitization to birch and timothy at 8 years. Furthermore, sensitization to birch pollen increased the risk significantly for sensitization to both cat and dog at 8 years. When investigating the role of sensitization at 4 years to cat, dog and horse in relation to sensitization to these animals at 8 years, the picture seen for pollens was not that obvious. Sensitization to mites at 4 years significantly increased risks of sensitization later to other inhalant allergens, but after adjustment for the other allergens tested, the risk disappeared. For mites and mould, the samples were small, and consequently the CIs were wide. Hence, interpretation needs to be made with caution.
Table 2.
Odds ratios (ORs) for sensitization to birch, timothy, cat and dog at 8 years of age if sensitized to different allergens at 4 years of age
| Birch sensitized at 8 years (N=312) | Timothy sensitized at 8 years (N=291) | Cat sensitized at 8 years (N=255) | Dog sensitized at 8 years (N=233) | |||||
|---|---|---|---|---|---|---|---|---|
| Sensitized at 4 | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI |
| Birch, N=190I | ||||||||
| Adjusted I | 521 | 209–1299 | 18 | 13–26 | 18 | 13–26 | 25 | 18–36 |
| Adjusted II | 253 | 89–645 | 5.6 | 3.4–9.2 | 5.1 | 3.0–8.7 | 6.2 | 3.7–10 |
| Timothy, N=122 | ||||||||
| Adjusted I | 19 | 12–30 | 56.1 | 32–98 | 8.9 | 6.0–13 | 19 | 2.2–28 |
| Adjusted II | 3.7 | 1.8–7.7 | 25 | 13.0–47.0 | 1.8 | 0.9–3.5 | 5 | 2.7–9.0 |
| Mugwort, N=32 | ||||||||
| Adjusted I | 178 | 24–1315 | 206 | 28–1527 | 15 | 7.0–33 | 29 | 12–69 |
| Adjusted II | 22 | 1.8–264 | 20 | 2.0–238 | 0.8 | 0.2–2.5 | 1.1 | 0.3–3.9 |
| Mould, N=20 | ||||||||
| Adjusted I | 49 | 11–216 | 10.3 | 3.8–28 | 40 | 11–140 | 17 | 6.3–48 |
| Adjusted II | 7.9 | 0.7–90 | 0.3 | 0.1–1.5 | 13 | 2.0–32 | 0.5 | 0.1–2.9 |
| Cat, N=120 | ||||||||
| Adjusted I | 24 | 15–38.2 | 11.8 | 7.8–18 | 182 | 83–399 | 43 | 27–70 |
| Adjusted II | 3.1 | 1.2–7.8 | 1.5 | 0.7–3.1 | 68 | 26–177 | 4.6 | 2.3–9.2 |
| Dog, N=96 | ||||||||
| Adjusted I | 23 | 14–39 | 15.8 | 9.8–25 | 44 | 25–77 | 124 | 57–264 |
| Adjusted II | 2.1 | 0.7–6.2 | 2.2 | 0.9–5.4 | 4 | 1.6–10.3 | 18 | 7.0–47 |
| Horse, N=64 | ||||||||
| Adjusted I | 31 | 15–62 | 12.9 | 7.3–23 | 41 | 21–83 | 63 | 29–136 |
| Adjusted II | 1.1 | 0.3–4.5 | 1.8 | 0.7–4.5 | 2.5 | 0.9–6.9 | 3.0 | 1.1–8.2 |
| Mites, N=36 | ||||||||
| Adjusted I | 3.9 | 1.9–7.6 | 2.4 | 1.2–5.0 | 2.2 | 1.1–4.8 | 3.8 | 1.9–7.7 |
| Adjusted II | 1.0 | 0.25–3.5 | 0.3 | 0.1–1.1 | 0.1 | 0.02–0.5 | 0.6 | 0.2–2.2 |
| Fx5®, N=335 | ||||||||
| Adjusted I | 5.8 | 4.4–7.6 | 5.2 | 3.9–7.0 | 5.2 | 3.9–7.0 | 7.1 | 5.2–9.6 |
| Adjusted II | 1.7 | 1.0–2.8 | 1.8 | 1.2–2.7 | 1.7 | 1.1–2.6 | 2.2 | 1.4–3.4 |
Adjustments are made (I) parental allergy and sex, and (II) as in (I) but also for each inhalant allergen tested and fx5®.CI, confidence interval.
Table 3.
Odds Ratios (ORs) for sensitization to birch, timothy, cat and dog at 8 years of age if sensitized to different food allergens at 4 years of age adjusted for (I) parental allergy and sex and (II) as in (I) but also for each food allergen tested and Phadiatop®
| Birch sensitized at 8 (N=312) | Timothy sensitized at 8 (N=291) | Cat sensitized at 8 (N=255) | Dog sensitized at 8 (N=233) | |||||
|---|---|---|---|---|---|---|---|---|
| Sensitized at 4 | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI |
| Egg white, N=106 | ||||||||
| Adjusted I | 7.2 | 4.7–11 | 5.1 | 3.3–7.9 | 6.1 | 4.0–9.3 | 7.7 | 5.0–12 |
| Adjusted II | 1.5 | 0.7–3.2 | 0.8 | 0.4–1.7 | 1.2 | 0.6–2.4 | 1.9 | 0.9–3.9 |
| Milk, N=184 | ||||||||
| Adjusted I | 4.1 | 2.9–5.7 | 3.5 | 2.4–4.9 | 3.7 | 2.6–5.3 | 3.6 | 2.5–5.1 |
| Adjusted II | 1.4 | 0.8–2.5 | 1.2 | 0.7–2.1 | 1.3 | 0.7–2.2 | 0.7 | 0.4–1.4 |
| Wheat, N=81 | ||||||||
| Adjusted I | 15 | 9.3–26 | 12 | 7.5–20 | 11 | 6.6–17 | 13 | 8.0–21 |
| Adjusted II | 1.6 | 0.7–3.7 | 1.7 | 0.8–3.7 | 1.4 | 0.7–2.8 | 1.0 | 0.5–2.2 |
| Peanut, N=117 | ||||||||
| Adjusted I | 12 | 8.2–19 | 11 | 7.6–17 | 9.3 | 6.2–14 | 16 | 10–24 |
| Adjusted II | 1.4 | 0.7–2.7 | 2.1 | 1.2–3.8 | 1.4 | 0.8–2.6 | 3.1 | 1.7–5.7 |
CI, confidence interval.
Sensitization to food allergens (fx5®) at 4 years of age, increased the risk of onset of sensitization to birch, timothy, cat and dog, at 8 years, even after adjustments for each of the other inhalant allergens (Table 3). When analysing sensitization at 4 years to the four most common food allergens (egg, milk, wheat and peanut) only sensitization to peanut at 4 years of age was significantly associated with an increased risk of allergen-specific IgE-ab to timothy and dog at 8 years.
Discussion
The major findings in our study are that both the prevalence of sensitization and the IgE-ab concentrations among children sensitized to the most common inhalant allergens almost doubled between 4 and 8 years of age. Furthermore, the IgE-ab concentrations to important allergens seem to increase with the number of sensitizing allergens. This finding is important because it may also explain the likelihood of a more severe and brittle allergic disease among children with high IgE-ab levels [6, 9, 11, 16, 17]. Such individuals have a lesser likelihood to remit, are more likely to be sensitized to increased number of inhalant allergens and hence are more exposed in terms of a longer season or a higher dose of total allergen exposure.
The prevalence of sensitization to inhalant allergens in our study is rather similar to that in other studies [4, 8, 18], although the panorama of allergen exposure is different in different geographic areas. In northern Europe birch is the dominating allergen, and we have shown that it seems to be the most significant inhalant allergen in terms of prevalence and IgE-ab concentrations both at 4 and at 8 years of age. It also seems to be a facilitator for further development of sensitization to other major inhalant allergens. It was surprising that already at the age of 4 birch was the dominating inhalant allergen, because clinical symptoms to birch pollen allergy in Sweden are believed to have their onset at early school age.
Furthermore, proportionally fewer children had onset of sensitization to birch between 4 and 8 years as compared with the other inhalant allergens, even though IgE-ab levels to birch more than doubled. Levels and duration of exposure may have an influence on the way sensitization to a subsequent allergen occurs [19, 20]. In Northern Europe high birch pollen exposure during a very short period of time seems more hazardous compared with intermittent exposure to lower levels of pollen (grass, mugwort) or perennial exposure (furred animals) of inhalant allergens. Besides, sensitization to birch at 4 years seemed to often precede sensitization to timothy, cat and dog at 8 years. This is in line with our previous results of the 4-year follow-up [16]. One might argue that in our region, with high birch pollen counts during a limited period at spring time, sensitization to birch early in life could be a “driving force” for the sensitizing process to inhalant allergens. Hypothetically, this could have implications for therapeutic interventions such as allergen-specific immunotherapy early in life.
Sensitization to HDM and mould was rather uncommon as compared with studies from other countries or continents [5, 7, 9, 18]. This reflects a low exposure to mites around Stockholm [19, 21]. Thus, the hypothesis of high-dose exposure for induction of tolerance vs. low-dose exposure increasing the risk of sensitization, does not seem to hold true for high dose and intermittent allergen exposure from allergens of plant origin [22, 23]. IgE-ab to cat was the dominating allergen among the furred animal allergens. This has been shown by others [18]. Sensitization to dog and horse in particular was closely related to sensitization to cat. It should be noted that 73–75% of dog and 70–83% of horse-sensitized children were co-sensitized to cat at 4 or 8 years, respectively. Hence, isolated horse sensitization was uncommon. An association between early exposure to cat and sensitization to cat has been shown by others [24, 25], but to our knowledge such comparisons have not been made for exposure to horse and sensitization to horse. It is tempting to believe that sensitization to horse in young children where few have started horseback-riding is rather an indicator of sensitization to inhalant allergens in general and to furred animals in particular.
To our knowledge the dynamic process of development of specific IgE-ab against the most common inhalant allergens over time, in terms of patterns of sensitization and specific IgE-ab concentrations, has not been as thoroughly described before [26]. We could demonstrate that persistent sensitization, i.e. sensitization to the same allergens both at 4 and at 8 years was related to higher levels of that allergen at 8 years of age as compared with those with onset of sensitization between 4 and 8 years of age. Transient sensitization to food allergens in childhood is common [13, 27]. Transient sensitization to inhalant allergens has been less studied. In our cohort of 2033 children between 4 and 8 years of age, de-sensitization to an inhalant allergen varied, between 3% and 9% for birch, mugwort, cat dog and horse. Transient sensitization was more common for timothy (14%), mould (30%) and mites (31%). It is noteworthy that the allergen-specific IgE-ab concentrations among the children who went into remission when re-tested at the age of 8 years were generally low at the age of 4. This is also in line with data in adults [28].
Our data show that that there is a strong association between allergens and risk of sensitization, not only within groups of allergens, i.e. allergens of plant origin or animal origin, which has been described before [18], but also in terms of hierarchy between sensitizing allergens both at 4 and at 8 years and in particular birch as the “play mate” of further sensitization from 4 to 8 years. The ORs for sensitization to the four most common sensitizing allergens, i.e. birch, timothy, cat and dog at the age of 8 years differ considerably after adjustment of each single allergens as well as fx5® at 4 years. The unadjusted data indicate the relevance of multiple allergies for the highly atopic child, whereas the adjusted data demonstrate the role of a single sensitizing allergen and its significance for the further sensitizing process during childhood. It was interesting that a food-specific IgE-ab (fx5®) ≥0.35 kUA/L at 4 years increased the risk of sensitization to birch and timothy pollen as well as cat and dog, even after adjustment for these inhalants at the age of 4. This clearly shows that progression of sensitization may shift from foods of animal and plant origin over to pollen and animal allergens [4, 8, 9, 13].
The strength of this study is the large size, the population-based design, the relatively small loss of study subjects during the follow-up and that children from whom blood samples were obtained did not differ in any major respect as compared with those from whom no blood was drawn, even though the length of follow-up is limited. This allows us to make generalisations of the findings. However, because parental allergy was more prevalent among the studied children than among children not providing a blood sample, the prevalence of sensitization is likely to be slightly higher in the population under study as compared with the general population.
Our findings suggest that sensitization to inhalant allergens in children between 4 and 8 years of age is a dynamic process. In our region birch allergen, seems to precede, and may even be driving the further sensitizing process which may be considered for further studies on therapeutic interventions. On the other hand, sensitization to low-exposure allergens such as mugwort in our region may serve more as markers of extended sensitization in a highly atopic individual. The change in sensitization to food allergens of the participating children during the age period studied will be presented elsewhere.
We believe that the information obtained in this paper is useful in interpreting the results of IgE-testing and for assessment of the prognosis among young children sensitized to inhalant allergens.
Acknowledgments
Funding: This work was supported by the Swedish Asthma and Allergy Foundation, the Swedish Heart and Lung Foundation, the Vardal Foundation for Health Care Sciences and Allergy Research and Stockholm County Council, Stockholm, Sweden.
References
- 1.Asplund KPG, Svartengren M. Environmental Health Report 2005, extended summary Allergic diseases, pp 12–13: The National Board of Health and Welfare, Institute of Environmental Medicine (Karolinska Institutet), Stockholm Centre for Public Health (Stockholm County Council),2005.
- 2.Arshad SH, Tariq SM, Matthews S, Hakim E. Sensitization to common allergens and its association with allergic disorders at age 4 years: a whole population birth cohort study. Pediatrics. 2001;108:E33. doi: 10.1542/peds.108.2.e33. [DOI] [PubMed] [Google Scholar]
- 3.Ernst P, Ghezzo H, Becklake MR. Risk factors for bronchial hyperresponsiveness in late childhood and early adolescence. Eur Respir J. 2002;20:635–9. doi: 10.1183/09031936.02.00962002. [DOI] [PubMed] [Google Scholar]
- 4.Illi S, von Mutius E, Lau S, et al. The pattern of atopic sensitization is associated with the development of asthma in childhood. J Allergy Clin Immunol. 2001;108:709–14. doi: 10.1067/mai.2001.118786. [DOI] [PubMed] [Google Scholar]
- 5.Kurukulaaratchy RJ, Matthews S, Arshad SH. Defining childhood atopic phenotypes to investigate the association of atopic sensitization with allergic disease. Allergy. 2005;60:1280–6. doi: 10.1111/j.1398-9995.2005.00890.x. [DOI] [PubMed] [Google Scholar]
- 6.Simpson A, Soderstrom L, Ahlstedt S, Murray CS, Woodcock A, Custovic A. IgE antibody quantification and the probability of wheeze in preschool children. J Allergy Clin Immunol. 2005;116:744–9. doi: 10.1016/j.jaci.2005.06.032. [DOI] [PubMed] [Google Scholar]
- 7.Arshad SH, Kurukulaaratchy RJ, Fenn M, Matthews S. Early life risk factors for current wheeze, asthma, and bronchial hyperresponsiveness at 10 years of age. Chest. 2005;127:502–8. doi: 10.1378/chest.127.2.502. [DOI] [PubMed] [Google Scholar]
- 8.Guilbert TW, Morgan WJ, Zeiger RS, et al. Atopic characteristics of children with recurrent wheezing at high risk for the development of childhood asthma. J Allergy Clin Immunol. 2004;114:1282–7. doi: 10.1016/j.jaci.2004.09.020. [DOI] [PubMed] [Google Scholar]
- 9.Illi S, von Mutius E, Lau S, Niggemann B, Gruber C, Wahn U. Perennial allergen sensitisation early in life and chronic asthma in children: a birth cohort study. Lancet. 2006;368:763–70. doi: 10.1016/S0140-6736(06)69286-6. [DOI] [PubMed] [Google Scholar]
- 10.Kulig M, Tacke U, Forster J, et al. Serum IgE levels during the first 6 years of life. J Pediatr. 1999;134:453–8. doi: 10.1016/s0022-3476(99)70203-9. [DOI] [PubMed] [Google Scholar]
- 11.Wickman M, Lilja G, Soderstrom L, van Hage-Hamsten M, Ahlstedt S. Quantitative analysis of IgE antibodies to food and inhalant allergens in 4-year-old children reflects their likelihood of allergic disease. Allergy. 2005;60:650–7. doi: 10.1111/j.1398-9995.2004.00764.x. [DOI] [PubMed] [Google Scholar]
- 12.Marinho S, Simpson A, Lowe L, Kissen P, Murray C, Custovic A. Rhinoconjunctivitis in 5-year-old children: a population-based birth cohort study. Allergy. 2007;62:385–93. doi: 10.1111/j.1398-9995.2006.01294.x. [DOI] [PubMed] [Google Scholar]
- 13.Kulig M, Bergmann R, Klettke U, Wahn V, Tacke U, Wahn U. Natural course of sensitization to food and inhalant allergens during the first 6 years of life. J Allergy Clin Immunol. 1999;103:1173–9. doi: 10.1016/s0091-6749(99)70195-8. [DOI] [PubMed] [Google Scholar]
- 14.Wickman M, Kull I, Pershagen G, Nordvall SL. The BAMSE project: presentation of a prospective longitudinal birth cohort study. Pediatr Allergy Immunol. 2002;13(Suppl. 15):11–3. doi: 10.1034/j.1399-3038.13.s.15.10.x. [DOI] [PubMed] [Google Scholar]
- 15.Kull I, Bergstrom A, Lilja G, Pershagen G, Wickman M. Fish consumption during the first year of life and development of allergic diseases during childhood. Allergy. 2006;61:1009–15. doi: 10.1111/j.1398-9995.2006.01115.x. [DOI] [PubMed] [Google Scholar]
- 16.Ghunaim N, Wickman M, Almqvist C, Soderstrom L, Ahlstedt S, van Hage M. Sensitization to different pollens and allergic disease in 4-year-old Swedish children. Clin Exp Allergy. 2006;36:722–7. doi: 10.1111/j.1365-2222.2006.02489.x. [DOI] [PubMed] [Google Scholar]
- 17.Wickman M, Ahlstedt S, Lilja G, van Hage Hamsten M. Quantification of IgE antibodies simplifies the classification of allergic diseases in 4-year-old children. A report from the prospective birth cohort study – BAMSE. Pediatr Allergy Immunol. 2003;14:441–7. doi: 10.1046/j.0905-6157.2003.00079.x. [DOI] [PubMed] [Google Scholar]
- 18.Roberts G, Peckitt C, Northstone K, et al. Relationship between aeroallergen and food allergen sensitization in childhood. Clin Exp Allergy. 2005;35:933–40. doi: 10.1111/j.1365-2222.2005.02280.x. [DOI] [PubMed] [Google Scholar]
- 19.De Lovinfosse S, Charpin D, Dornelas A, Birnbaum J, Vervloet D. Can mite-specific IgE be used as a surrogate for mite exposure? Allergy. 1994;49:64–6. doi: 10.1111/j.1398-9995.1994.tb00776.x. [DOI] [PubMed] [Google Scholar]
- 20.Kihlstrom A, Lilja G, Pershagen G, Hedlin G. Exposure to birch pollen in infancy and development of atopic disease in childhood. J Allergy Clin Immunol. 2002;110:78–84. doi: 10.1067/mai.2002.125829. [DOI] [PubMed] [Google Scholar]
- 21.Wickman M, Nordvall SL, Pershagen G, Korsgaard J, Johansen N. Sensitization to domestic mites in a cold temperate region. Am Rev Resp Dis. 1993;148:58–62. doi: 10.1164/ajrccm/148.1.58. [DOI] [PubMed] [Google Scholar]
- 22.Custovic A, Hallam CL, Simpson BM, Craven M, Simpson A, Woodcock A. Decreased prevalence of sensitization to cats with high exposure to cat allergen. J Allergy Clin Immunol. 2001;108:537–9. doi: 10.1067/mai.2001.118599. [DOI] [PubMed] [Google Scholar]
- 23.Platts-Mills T, Vaughan J, Squillace S, Woodfolk J, Sporik R. Sensitisation, asthma, and a modified Th2 response in children exposed to cat allergen: a population-based cross-sectional study. Lancet. 2001;357:752–6. doi: 10.1016/S0140-6736(00)04168-4. [DOI] [PubMed] [Google Scholar]
- 24.Almqvist C, Egmar AC, Hedlin G, et al. Direct and indirect exposure to pets – risk of sensitization and asthma at 4 years in a birth cohort. Clin Exp Allergy. 2003;33:1190–7. doi: 10.1046/j.1365-2222.2003.01764.x. [DOI] [PubMed] [Google Scholar]
- 25.Chen CM, Rzehak P, Zutavern A, et al. Longitudinal study on cat allergen exposure and the development of allergy in young children. J Allergy Clin Immunol. 2007;119:1148–55. doi: 10.1016/j.jaci.2007.02.017. [DOI] [PubMed] [Google Scholar]
- 26.Kuehr J, Karmaus W, Frischer T, et al. Longitudinal variability of skin prick test results. Clin Exp Allergy. 1992;22:839–44. doi: 10.1111/j.1365-2222.1992.tb02829.x. [DOI] [PubMed] [Google Scholar]
- 27.Sigurs N, Hattevig G, Kjellman B, Kjellman NI, Nilsson L, Bjorksten B. Appearance of atopic disease in relation to serum IgE antibodies in children followed up from birth for 4 to 15 years. J Allergy Clin Immunol. 1994;94:757–63. doi: 10.1016/0091-6749(94)90184-8. [DOI] [PubMed] [Google Scholar]
- 28.Bodtger U, Linneberg A. Remission of allergic rhinitis: an 8-year observational study. J Allergy Clin Immunol. 2004;114:1384–8. doi: 10.1016/j.jaci.2004.08.039. [DOI] [PubMed] [Google Scholar]