Abstract
Rosai-Dorfman disease is a rare idiopathic disorder characterized by painless lymphadenopathy with cervical involvement in more than 80% cases. We report a case of Rosai-Dorfman disease presenting as an isolated epibulbar mass in a healthy young adult male. Epibulbar involvement in Rosai-Dorfman disease is a rare presentation as can be seen from a review of all literature. The presentation, differential diagnosis and treatment are discussed.
Keywords: Epibulbar mass, Rosai-Dorfman disease
Since the original description by Rosai and Dorfman,1 of sinus histiocytosis with massive lymphadenopathy (SHML), it has been recognized that this disease may occur in extranodal sites, often without any involvement of lymph nodes. Approximately 10% of all cases of Rosai-Dorfman disease (RDD) are associated with soft tissue involvement, and in some cases this may be the sole manifestation of the disorder.2,3 The orbit is a common extranodal site for RDD,4 epibulbar involvement is very rare.
We report a case of extranodal RDD presenting as epibulbar mass without any other manifestation. Previously only four cases of RDD presenting as epibulbar conjunctival mass have been reported (Medline search).
Case Report
A 17-year-old healthy male was seen with complaints of painless swelling over the left eye for the past four weeks. The rest of the systemic and ocular history was not significant. On examination his vision was 20/20 both eyes. On slit-lamp examination there was erythematous, subconjunctival nodular mass in the left eye [Figure 1]. The lesion had a smooth surface with normal surrounding sclera and was not tender. The mass appeared to be adherent to the underlying tissue. Anterior segment and fundus examination was otherwise normal. Systemic evaluation was negative and there was no lymphadenopathy. Hemoglobin, red blood cell count, total and differential white blood cell count, platelet count, erythrocyte sedimentation rate (ESR) and blood smear were normal. The patient underwent incision biopsy and the mass was subjected to histopathology. Hematoxylin and eosin stained sections showed a mixed cellular infiltrate, predominantly composed of histiocytes mixed with lymphocytes, including plasma cells and polymorphous nuclear leucocytes. Several of these histiocytes showed emperipolesis, displaying phagocytosed lymphocytes. Histiocytes were filled with pink cytoplasm and contained lymphocytes, a pathognomic finding also known as lymphophagocytosis [Figure 2]. Stains for bacteria, fungus and acid-fast bacilli were negative. The patient was started on systemic prednisolone (1mg/kg body weight) on a tapering dose for a period of four weeks. At six weeks follow-up there were no new lesions and the subconjunctival mass showed no increase in size. The patient was advised a follow-up after three months.
Figure 1.
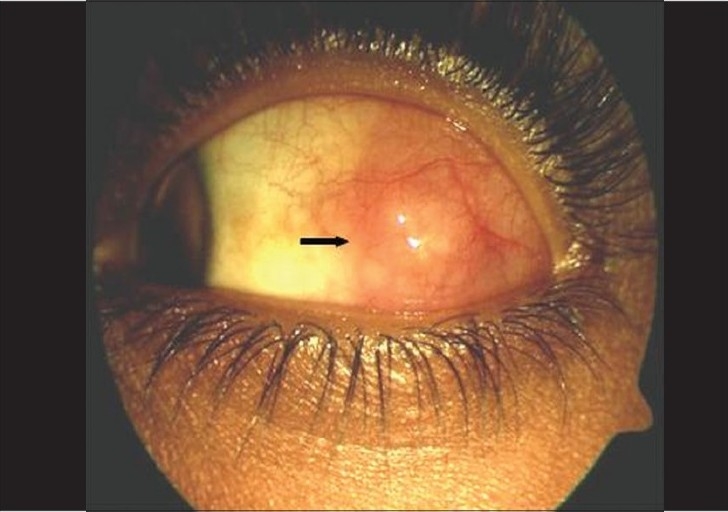
Clinical photograph demonstrating subconjunctival mass in the left eye (Black arrow)
Figure 2.
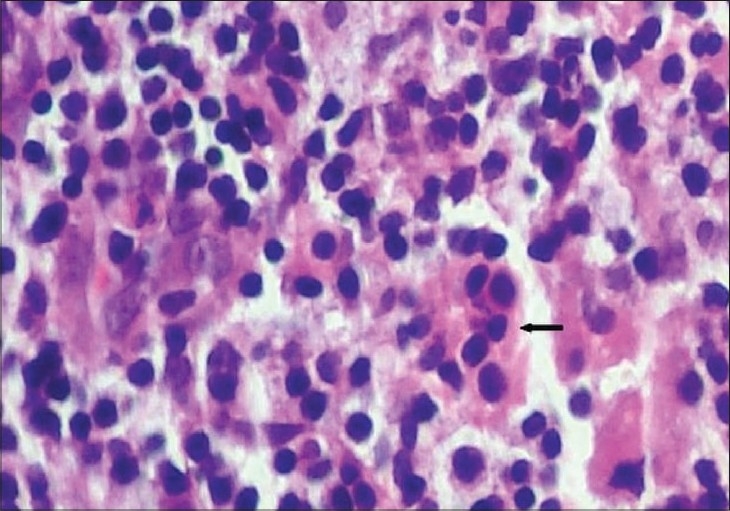
Chronic inflammatory infiltrate with lymphocytes, plasma cells, and histiocytes is present. Histiocyte with pink cytoplasm containing lymphocytes within its cytoplasm, demonstrating the characteristic histological fi nding termed emperipolesis (Black arrow) (H and E, × 200)
Discussion
Rosai and Dorfman first described sinus histiocytosis with massive lymphadenopathy in 1969.1 This disease mainly presents as a massive painless cervical adenopathy in children or young adults of African ancestry. Extranodal disease has been found to occur in 43% cases which may be widespread and most frequently involves the respiratory tract, paranasal sinuses, visceral organs, skin, bone, central nervous system, genitourinary tract, and orbit.2 Other features include low- grade fever, leukocytosis with neutrophilia, elevated ESR, and hypergammaglobulinemia.5 Ocular involvement is relatively uncommon (8.5%), and most cases have presented as lymphoproliferation in the soft tissues of the orbit and eyelids.6 Epibulbar mass as isolated finding of extranodal RDD is very rare with only four cases reported in the literature so far.7-9
The underlying cause of RDD is unclear. Epstein-Barr virus2 and human herpes virus 6,10 have been isolated in a few patients, but no clear association has been identified. Autoimmune disease, immunocompromise, and neoplastic cell disease may be a cause, but this remains unclear.2 There are rare associations with polycythemia vera, joint disease, glomerulonephritis, hematological antibodies, and Wiskott- Aldrich syndrome.2
The diagnosis of RDD is made on histopathology. Characteristic histological features are histiocytic infiltration admixed with lymphocytes and other inflammatory cells. One typical feature of this entity has been emperipolesis, with histiocytes demonstrating phagocytosed lymphocytes and plasma cells. The histiocytes are typically filled with pink cytoplasm and often contain lymphocytes, a pathognomic finding also known as lymphophagocytosis.
Histiocytes in RDD, Langerhan cell histiocytosis, and other histiocytosis express S-100, a neural tissue-specific protein; however, the pathophysiology of this S-100 expression remains obscure. Although positive staining for S-100 strongly suggests RDD, it is not absolutely required to make the diagnosis in the presence of typical histology of RDD.9 The disease is classically described to have an indolent, self-limiting course; however, this is not always the case. The various stages of disease progression are remission, recurrence, persistent but stable, primary progressive and death caused by the disease.
The therapy for RDD is yet to be determined because of the rarity of the disease and its propensity for spontaneous remission. Excision, radiation therapy, chemotherapy and systemic steroids have all been tried by different authors. The first line of interventional therapy to be considered is gross total excision along with adjuvant steroids or more aggressive chemotherapy or radiotherapy when necessary.11 In our patient the disease was stable at six weeks, however a close follow- up is needed to watch for any increase in size of the lesion or systemic spread.
Rosai-Dorfman disease is an entity that is part of a group of orbital/systemic disorders, including xanthogranulomas and sclerosing inflammation of the orbit, which share numerous anatomic, histological and pathophysiologic features. The differential diagnosis of RDD should include orbital sclerosing inflammation, xanthogranulomatous disease, B-cell lymphoma, and benign lymphoid hyperplasia.11 Other disorders that may superficially resemble RDD include Burkitt′s lymphoma, granulocytic sarcoma, rhabdomyosarcoma, neuroblastoma and Langerhans cell histiocytosis. The growth pattern of lymphoma and lymphoid hyperplasia are similar but these lesions do not have the cicatrizing feature seen with RDD. Sclerosing inflammation and xanthogranulomas can be differentiated by histological and immunohistochemical differences.11
Although the orbit and eyelid are common extranodal sites for ocular RDD, isolated epibulbar presentation is very rare. The authors would like to highlight that RDD may present as epibulbar nodules without any other nodal or extranodal involvement in young healthy adults and should be considered in the differential diagnosis by clinicians when evaluating epibulbar masses.
Acknowledgments
Anita Borges, MD; NPIL Laboratories and Diagnostics Pvt Limited, Mumbai.
References
- 1.Rosai J, Dorfman R. Sinus histiocytosis with massive lymphadenopathy: A newly recognized clinicopathological entity. Arch Pathol. 1969;82:63–70. [PubMed] [Google Scholar]
- 2.Foucar E, Rosai J, Dorfman R. Sinus histiocytosis with massive lymphadenopathy (Rosai Dorfman disease): REVIEW of the entity. Semin Diagn pathol. 1990;7:19–70. [PubMed] [Google Scholar]
- 3.Montgomery EA, Meis JM, Frizzera G. Rosai-Dorfman disease of soft tissue. Am J Surg Pathol. 1992;16:122. doi: 10.1097/00000478-199202000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Friendly DS, Font RL, Rao NA. Orbital involvement in ′sinus histiocytosis′. Arch Ophthalmol. 1977;95:2006–11. doi: 10.1001/archopht.1977.04450110100011. [DOI] [PubMed] [Google Scholar]
- 5.Rosai J, Dorfman R. Sinus histiocytosis with massive lymphadenopathy: A benign pseudolymphomatous benign disorder. Cancer. 1970;30:1174–88. doi: 10.1002/1097-0142(197211)30:5<1174::aid-cncr2820300507>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 6.Foucar E, Rosai J, Dorfman R. The ophthalmologic manifestations of sinus histiocytosis with massive lymphadenopathy. Am J Ophthalmol. 1979;87:354–67. doi: 10.1016/0002-9394(79)90077-1. [DOI] [PubMed] [Google Scholar]
- 7.Stopak SS, Dreizen NG, Zimmerman LE, O′Neill JF. Sinus histiocytosis presenting as epibulbar mass: A clinicopathologic case report. Arch Ophthalmol. 1988;106:1426–8. doi: 10.1001/archopht.1988.01060140590029. [DOI] [PubMed] [Google Scholar]
- 8.Ireland KC, Hutchinson AK, Grossinklaus HE. Sinus histiocytosis presenting as bilateral epibulbar masses. Am J Ophthalmol. 1999;127:360–1. doi: 10.1016/s0002-9394(98)00321-3. [DOI] [PubMed] [Google Scholar]
- 9.Albini TA, Evans M, See R, Rao NA, Marback E, De Souza MM. Rosai-Dorfman disease isolated epibulbar masses in two adult patients. Br J Ophthalmol. 2005;89:241–3. doi: 10.1136/bjo.2004.048256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Levine PH, Jahan N, Murari P, Manak M, Jaffe ES. Detection of human herpes virus 6 in tissues involved by sinus histiocytosis with massive lymphadenopathy. J Infect Dis. 1992;166:291–5. doi: 10.1093/infdis/166.2.291. [DOI] [PubMed] [Google Scholar]
- 11.Mohadjer Y, Holds JB, Rootman J, Wilson MW, Gigantelli JW, Custer PL. The spectrum of Orbital Rosai Dorfman disease. Ophthal Plast Reconstr Surg. 2006;22:163–8. doi: 10.1097/01.iop.0000217563.00975.a3. [DOI] [PubMed] [Google Scholar]


