Abstract
Purpose
To investigate the seroprevalence of toxocariasis in patients diagnosed as schizophrenia.
Patients and Methods
Ninety-eight schizophrenic patients hospitalized at The Elazığ Psychiatric Hospital were included in the study. Anti-Toxocara IgG and/or IgM antibodies were determined by using commercial Toxocara canis IgG and/or IgM ELISA kit.
Results
Seropositivity for T. canis was detected in 45 (45.9%) of 98 patients and 2 (2.0%) of 100 control subjects the difference was statistically significant (p < 0.001). The seroprevalence was 40.4% (19 cases) and 51.0% (26 cases) for female and male subjects, respectively (p = 0.3). When the seropositive and seronegative schizophrenic patients were compared with respect to the age group environment they were living in, occupation period of follow up and number of hospitalizations, there were no differences between the two groups (all, p > 0.05).
Conclusion
In conclusion, the schizophrenic state seems to present a high risk for Toxocara infection in Turkey.
Keywords: Toxocariasis, seroprevalence, schizophrenic patients
INTRODUCTION
Toxocariasis is a disease caused by Toxocara canis and T. cati, whose host, dogs and cats, respectively, excrete eggs in their faeces. After 1 - 3 weeks the eggs become embryonated and infectious. Humans become infected by oral ingestion of infectious eggs. The eggs hatch out in the intestine and larvae penetrate the wall and migrate to the liver and lungs. In the process body circulation organisms spread to various tissues and cause at least three syndromes in humans: visceral larva migrans syndrome, ocular larva migrans syndrome, and covert toxocariasis.1-3
A high seroprevalence of Toxocara infection has been found in developing countries where the climate is humid, which is appropriate for egg survival in soil.3-6 Human toxocariasis is common where the dog population is large but the state of hygiene is low. The highly infected population includes children, dog owners, people living in rural areas and people with pica syndrome.7-9 A high correlations between the style of life and Toxocara infection risk has been demonstrated. In addition, Toxocara infection may be increased in mentally retarded patients when adequate personal hygiene is not practised.7,10-12 Schizophrenic patients typically have poor hygiene and self-care skills. The literature about toxocariasis epidemiology in psychiatric patients is very sparse. In the present study, our aim was to investigate the seroprevalence of toxocariasis among schizophrenic patients and compare them with a healthy population in Turkey.
PATIENTS AND METHODS
Study area
The Elazig Psychiatric Hospital in which we performed this study is a regional mental hospital, one of the biggest and oldest, serving 18 surrounding provinces in Eastern Anatolian of Turkey. The hospital had a 400-bed capacity and 5200 m2 garden for the remission period of the patients.
Schizophrenic patients and control group
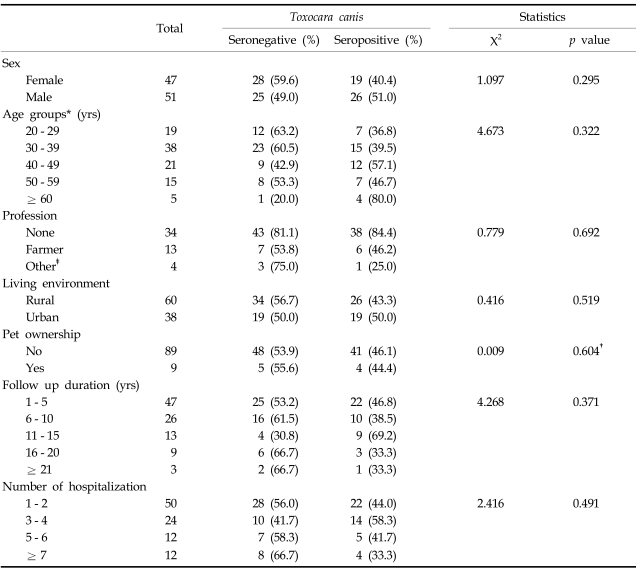
Ninety-eight schizophrenic patients were included in this study, who had been diagnosed according to the Diagnostic and Statistical Manual of Mental Disorders-IV criteria and hospitalized at Elazig Psychiatric Hospital. The patients' sera were collected when they were hospitalized. This study was performed according to the protocol approved by the Firat University Medical School's Ethics Committee and was permitted by from the authorities of Elazig Psychiatric Hospital. Since the majority (n = 93) of the patients were in the remission period of their disorder, the consent was directly obtained from them. For the other 5 patients, the consent was obtained from their relatives (n = 3) and legal guardians (n = 2). The data concerning the age, sex, environment conditions (rural or urban), profession, pet ownership, number of hospitalizations and follow-up periods were obtained from the 93 patients themselves and their medical records and from the relatives and legal guardians of the remaining 5 patients. Data are presented in Table 1.
Table 1.
Characteristics of Schizophrenic Patients
*Three 18 - 19 years old persons were included in the 20 - 29 years old age group.
†Fisher's Exact Test.
‡Include civil servant, worker (no soil-related), business man etc.
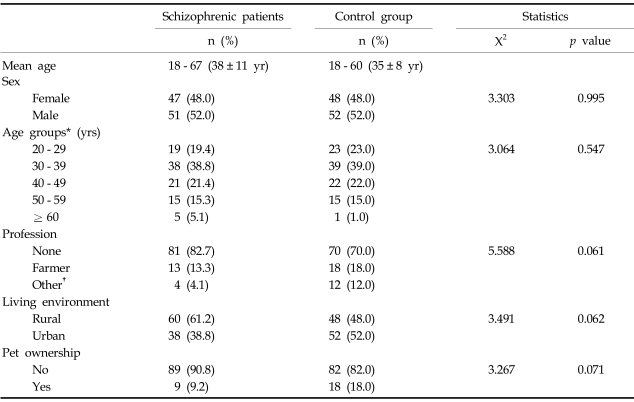
The control group was composed of healthy subjects who had similar socio-economic and environmental conditions with the schizophrenic patients (except the hospital condition and follow up duration). In addition, the controls did not have a history of major mood disorder, schizophrenia, and psychotic disorders, dementia, mental retardation or psychosis in their first-degree relatives. There were 100 volunteers (50 males and 50 females) aged 18 - 60 (35±8 year) in the control group (Table 2).
Table 2.
Comparison of Mean Age, Sex, Age Groups, Profession, Living Environment and Pet Ownership between Schizophrenic Patients and Control Group
*Three schizophrenic and control 18 - 19 years old persons were included in the 20 - 29 years age group.
†Include civil servant, worker (no soil-related), business man etc.
Serological evaluation
Blood samples (5 mL) were collected and separated serum samples were stored at -20℃ until used. Anti-Toxocara IgG and/or M antibodies were investigated in all cases by using a commercial T. canis IgG/M ELISA kit (Novum Diagnostica, Germany) containing purified specific excretory Toxocara canis antigens from the larval stage. ELISA test was performed according to the manufacturer's instruction. Absorbance at 450 nm was measured using an ELISA microtiter plate reader. Sera were diluted as 5 µL serum in 500 µL of sample diluent. Cut-off value (CO) was calculated as the mean absorbance value of the two negative control determinations plus constant factor f (0.250), and more than 10% above CO was considered to be positive. If the patient absorbance value was found between 10% above to 10% below CO (in the grey zone), a new patient sample was investigated 2 - 4 weeks later. If the results after the second test also fell in the grey zone or below, they were considered to be negative.
Investigation of soil samples
Thirty grams of soil or sand samples were taken from fifty different places in the hospital garden in order to determine the role of hospitalization in the Toxocara infection and the parasitic investigation of these samples was performed according to the ZnSO4 flotation method described by Kazacos.13
Statistical analysis
Statistical analysis was performed with the statistical package for social sciences (SPSS/PC 9.05 version, 1998) using Chi square test and Fisher's Exact test if needed. p < 0.005 was considered as statistically significant.
RESULTS
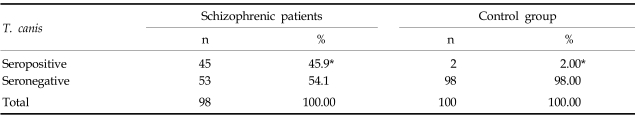
Seropositivity was detected in 45 of 98 schizophrenic patients (45.9%) and 2 out of 100 in the control subjects which showed statistically significant difference (p < 0.001) (Table 3). However, there were no significant differences between the seropositive and seronegative schizophrenic patients in respect of professions, environment conditions, following up periods and number of hospitalizations (Table 1). Even when the schizophrenic patients were divided into 10-year age groups, there was no significant difference. The seroprevalence was 40.4% (19 cases) and 51.0% (26 cases) for female and male subjects, respectively (p = 0.295) (Table 1). No significant difference was observed between the schizophrenic patients and control group in the analysis of population distribution according to mean age, sex, age groups, profession, living environment and pet ownership (Table 2). No was any Toxocara or any other helminth egg or larva was not detected in the soil and sand samples obtained from the garden of the hospital.
Table 3.
Seropositive Subjects in Schizophrenic Patients and Control Group
*Pearson Chi-Square; x2 = 52.736.
p < 0.001.
DISCUSSION
Toxocariasis is an important health problem in developing countries and was classically described as a disease of children.5,6 It has been reported that the seroprevalence of toxocariasis varies between 1.8 - 58.3% depending on country, study group, age and socio-cultural level.7,8,14-17 There are only a few studies reporting toxocariasis prevalence in Turkey. Saglam has shown that the seroprevalence was 6% in students at veterinary college and 10% in people exposed to dogs.18 He reported no toxocaral seropositivity in controls. We have previously shown that T. canis seroprevalence was 2.6% in healthy individuals in Elazig, an urban region in Turkey.19 In the present study, we showed a T. canis seroprevalence of 45.9% in schizophrenic patients, which is much higher than in the control group.
The diagnosis of human toxocariasis currently depends on serological tests using excretory-secretory antigens from T. canis second-stage larvae (TES), because it is extremely difficult to detect an infective Toxocara larva(e) in biopsy samples. ELISA and western-blotting are the most commonly used methods to determine anti-Toxocara antibodies.15,20-24 ELISA, which is practical and inexpensive, has been particularly recommended in seroepidemiological studies.15,25,26 It has been reported that use of TES antigens in ELISA is highly specific (86 - 100%) and sensitive (80 - 100%).15,17,25,26 Cross reactions have been reported for serological tests in helminthic infections (such as brugiasis, loiasis, trichinellosis, strongyloidiasis, gnathostomiasis, angiostrongylosis, anisakiasis, ascariasis, ancylostomiasis, schistosomiasis, paragonimiasis, fascioliasis, sparganosis and spirometriasis) when the TES are applied despite use of recombinant antigens.15,21-23,26 In our region, these helminthic infections have not been reported except ascariasis (0.3 - 10.4%) and fascioliasis (2.8%).27-31 Therefore, ELISA was utilized in the present study and it is believed that our results reflect the real prevalence of toxocariasis.
A comparatively high seroprevalence of Toxocara has been reported among persons living in rural communities, in keepers of dogs and/or cats, in those with the professions involving animal contact, in meat industry workers, in epileptics, in those with a history of pica and in those institutionalisation for mental retardation.9,11
Two reports have investigated the association between toxocariasis and institutionalization.10,11 Institutes for mentally retarded children have been reported to be endemic foci of protozoan and helminth infections, including toxocariasis.11 All of our patients were in-patients and were not institutionalised. They frequently had second, third or fourth admissions in this hospital but no patient had lifetime admission. There were unattended dogs and cats in the hospital's garden that the patients used. The presence of eggs and larvae of T. canis was investigated in soil samples taken from the garden in order to determine the role of hospitalization in the Toxocara infection. No T. canis, T. cati or any other helminth egg or larvae were detected in soil samples obtained from the garden of the hospital. This indicates that the area of the hospital where the patients were visiting was not contaminated at the time the study was performed. Additionally, there was no significant difference between Toxocara seropositive and seronegative patients in terms of follow up period and number of hospitalizations. Therefore, we suggest that Toxocara seropositivity may not be related to hospitalization.
The seroprevalence of Toxocara in childhood is higher than in adulthood.1,32 All the schizophrenic patients involved in this study were adults and no difference was found between the age groups with respect to Toxocara seropositivity, indicating a low correlation with age.
The high rate of Toxocara seroprevalence determined in schizophrenic patients could not be attributed to the factors including pet ownership, living environment and profession since the control group were selected with similar characteristics. Inadequate hygiene increases the risk of Toxocara infection.7,10-12 Schizophrenic patients can be expected to behave in uncontrolled fashion with respect to hygiene. Furthermore, people exposed to more than one risk factor show higher prevalence rates. However, we did not observe any significant difference between either of the seropositive or seronegative schizophrenic patients and the control subjects in terms of the factors that increase Toxocara infection risk. Determination of high seroprevalence suggests that these subjects constitute a risk for Toxocara infection. The risk in mentally retarded cases could not be related with behavioural patterns on the basis of the present findings. Therefore, this issue awaits further investigations with a larger sample to evaluate the high seropositivity we have determined.
In conclusion, Toxocara seroprevalence (45.9%) was much higher in schizophrenic patients than in the general population. These results suggest that the schizophrenic state presents a high risk for Toxocara infection.
ACKNOWLEDGEMENTS
We would like to express our gratitude to the chief of staff at Elazig Psychiatric Hospital for permission and his helpfulness during this study, and to all persons for their support and assistance in collecting the previously recorded data of the patients.
References
- 1.Garcia LS. Diagnostic Medical Parasitology. 4th ed. Washington, DC: American Society for Microbiology. (ASM Press); 2001. pp. 309–312. [Google Scholar]
- 2.Nathwani D, Laing RB, Currie PF. Covert toxocariasis-a cause of recurrent abdominal pain in childhood. Br J Clin Pract. 1992;46:271. [PubMed] [Google Scholar]
- 3.Magnaval JF, Glickman LT, Dorchies P, Morassin B. Highlights of human toxocariasis. Korean J Parasitol. 2001;39:1–11. doi: 10.3347/kjp.2001.39.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thompson DE, Bundy DA, Cooper ES, Schantz PM. Epidemiological characteristics of Toxocara canis zoonotic infection of children in a Caribbean community. Bull World Health Organ. 1986;64:283–298. [PMC free article] [PubMed] [Google Scholar]
- 5.Oge S, Oge H. Prevalence of Toxocara spp. eggs in the soil of public parks in Ankara, Turkey. Dtsch Tierarztl Wochenschr. 2000;107:72–75. [PubMed] [Google Scholar]
- 6.Kaplan M, Kuk S, Kalkan A. Examination of Toxocara spp. in different playgrounds in Elazig. Firat Univ J Health Sci. 2002;16:277–279. [Google Scholar]
- 7.Fenoy S, Cuellar C, Guillen JL. Serological evidence of toxocariasis in patients from Spain with a clinical suspicion of visceral larva migrans. J Helminthol. 1997;71:9–12. doi: 10.1017/s0022149x00000729. [DOI] [PubMed] [Google Scholar]
- 8.Radman NE, Archelli SM, Fonrouge RD, del V Guardis M, Linzitto OR. Human toxocarosis. Its seroprevalence in the city of La Plata. Mem Inst Oswaldo Cruz. 2000;95:281–285. doi: 10.1590/s0074-02762000000300001. [DOI] [PubMed] [Google Scholar]
- 9.Holland CV, O'Lorcain P, Taylor MR, Kelly A. Seroepidemiology of toxocariasis in school children. Parasitology. 1995;110:535–545. doi: 10.1017/s0031182000065252. [DOI] [PubMed] [Google Scholar]
- 10.Brook I, Fish CH, Schantz PM, Cotton DD. Toxocariasis in an institution for the mentally retarded. Infect Control. 1981;2:317–320. doi: 10.1017/s0195941700055375. [DOI] [PubMed] [Google Scholar]
- 11.Huminer D, Symon K, Groskopf I, Pietrushka D, Kremer I, Schantz PM, et al. Seroepidemiologic study of toxocariasis and strongyloidiasis in institutionalized mentally retarded adults. Am J Trop Med Hyg. 1992;46:278–281. doi: 10.4269/ajtmh.1992.46.278. [DOI] [PubMed] [Google Scholar]
- 12.Mohamed NH, Salem SA, Azab ME, Bebars MA, Khattab HM, Kamal AM, et al. Parasitic infections associated with mental retardation in Egypt. J Egypt Soc Parasitol. 1991;21:319–331. [PubMed] [Google Scholar]
- 13.Kazacos KR. Improved method for recovering ascarid and other helminth eggs from soil associated with epizootics and during survey studies. Am J Vet Res. 1983;44:896–900. [PubMed] [Google Scholar]
- 14.Ajayi OO, Duhlinska DD, Agwale SM, Njoku M. Frequency of human toxocariasis in Jos, Plateau State, Nigeria. Mem Inst Oswaldo Cruz. 2000;95:147–149. doi: 10.1590/S0074-02762000000200002. [DOI] [PubMed] [Google Scholar]
- 15.Park HY, Lee SU, Huh S, Kong Y, Magnaval JF. A seroepidemiological survey for toxocariasis in apparently healthy residents in Gangwon-do, Korea. Korean J Parasitol. 2002;40:113–117. doi: 10.3347/kjp.2002.40.3.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jimenez JF, Valladares B, Fernandez-Palacios JM, de Armas F, del Castillo A. A serologic study of human toxocariasis in the Canary Islands (Spain): environmental influences. Am J Trop Med Hyg. 1997;56:113–115. doi: 10.4269/ajtmh.1997.56.113. [DOI] [PubMed] [Google Scholar]
- 17.Dubinsky P, Akao N, Reiterová K, Konáková G. Comparison of the sensitive screening kit with two ELISA sets for detection of anti-Toxocara antibodies. Southeast Asian J Trop Med Public Health. 2000;31:394–398. [PubMed] [Google Scholar]
- 18.Saglam MG. Evaluation of Toxocara canis occurrence by the ELISA method. Istanbul University, Institute of Health Sciences; 1999. Master of Philosophy (MPhil) Thesis. [Google Scholar]
- 19.Kaplan M, Gödekmerdan A, Kalkan A, Erensoy A, Ozden M. Toxocara canis Seroprevalence in Elaziğ suburb in Turkey. Firat Univ J Health Sci. 1999;13:51–54. [Google Scholar]
- 20.Akao N, Chu AE, Tsukidate S, Fujita K. A rapid and sensitive screening kit for the detection of anti-Toxocara larval ES antibodies. Parasitol Int. 1997;46:189–195. [Google Scholar]
- 21.Lynch NR, Wilkes LK, Hodgen AN, Turner KJ. Specificity of Toxocara ELISA in tropical populations. Parasite Immunol. 1988;10:323–337. doi: 10.1111/j.1365-3024.1988.tb00224.x. [DOI] [PubMed] [Google Scholar]
- 22.Ishida MM, Rubinsky-Elefant G, Ferreira AW, Hoshino-Shimizu S, Vaz AJ. Helminth antigens (Taenia solium, Taenia crassiceps, Toxocara canis, Schistosoma mansoni and Echinococcus granulosus) and cross-reactivities in human infections and immunized animals. Acta Trop. 2003;89:73–84. doi: 10.1016/j.actatropica.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 23.Gillespie SH, Bidwell D, Voller A, Robertson BD, Maizels RM. Diagnosis of human toxocariasis by antigen capture enzyme linked immunosorbent assay. J Clin Pathol. 1993;46:551–554. doi: 10.1136/jcp.46.6.551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yamasaki H, Taib R, Watanabe Y, Mak JW, Zasmy N, Araki K, et al. Molecular characterization of a cDNA encoding an excretory-secretory antigen from Toxocara canis second stage larvae and its application to the immunodiagnosis of human toxocariasis. Parasitol Int. 1998;47:171–181. [Google Scholar]
- 25.Malla N, Aggarwal AK, Mahajan RC. A serological study of human toxocariasis in north India. Natl Med J India. 2002;15:145–147. [PubMed] [Google Scholar]
- 26.Yamasaki H, Araki K, Lim PK, Zasmy N, Mak JW, Taib R, et al. Development of a highly specific recombinant Toxocara canis second-stage larva excretory- secretory antigen for immunodiagnosis of human toxocariasis. J Clin Microbiol. 2000;38:1409–1413. doi: 10.1128/jcm.38.4.1409-1413.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Godekmerdan A, Serthatlioglu S, Kalkan A, Murat A, Kaplan M. Cases of extraintestinal ascariasis. Acta Parasitol Turc. 1999;23:141–145. [Google Scholar]
- 28.Yilmaz M, Ay S, Kilic SS, Kokcam I. Distribution of intestinal parasites in school Elaziğ. Acta Parasitol Turc. 1989;13:55–58. [Google Scholar]
- 29.Yilmaz M, Ay S, Orak S, Asci Z, Yucel AY. Distribution of intestinal parasites in street-sweepers and Meat-Fish Corporation staff in Elaziğ. Acta Parasitol Turc. 1989;13:59–62. [Google Scholar]
- 30.Yilmaz M, Kokcam I, Ay S, Seckin N. Distribution of intestinal parasites in Elazığ Mental Hospital. Acta Parasitol Turc. 1989;13:51–53. [Google Scholar]
- 31.Kaplan M, Kuk S, Kalkan A, Demirdağ K, Ozdarendeli A. Fasciola hepatica seroprevalence in the Elaziğ region. Mikrobiyol Bul. 2002;36:337–342. [PubMed] [Google Scholar]
- 32.Alonso JM, Bojanich MV, Chamorro M, Gorodner JO. Toxocara seroprevalence in children from a subtropical city in Argentina. Rev Inst Med Trop Sao Paulo. 2000;42:235–237. doi: 10.1590/s0036-46652000000400010. [DOI] [PubMed] [Google Scholar]